EASTPOINTE FAMILY PHYSICIANS
advertisement

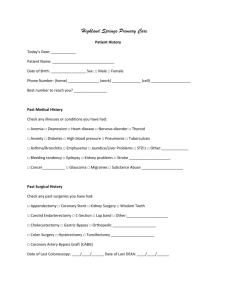
TODAY’S DATE:________________________ PEDIATRIC HISTORY FORM Parents – Please answer the following questions about your child. PATIENT NAME: __________________________________ DATE OF BIRTH: _________________ MEDICATION – List all current medications and dosages ALLERGIES/REACTION TO MEDICATION ___________________________________________ ______________________________________ ___________________________________________ ______________________________________ ___________________________________________ ______________________________________ ___________________________________________ _______________Latex Allergy: Yes No HOSPITAL ADMISSIONS Year Illness or Operation/Physician ________ _____________________________ Year _________ Illness or Operation/Physician ____________________________ ________ _____________________________ _________ ____________________________ ________ _____________________________ _________ ____________________________ PATIENT SYMPTOMS- Please check all that apply Ear infection-frequent Diarrhea/Constipation Vision Problems Feeding Problems Eye Problems Jaundice/Hepatitis Nose bleeds-recurrent Hernia Sinus trouble Problems with Urination Sore throats-frequent Weight Loss-recent Hayfever/Allergies Anemia Pneumonia/Pleurisy Convulsions/Seizures Bronchitis/Chronic cough Headaches Asthma/Wheezing Bone Fracture/Joint injury Heart Murmur Rashes/Hives Loss of appetite-recent Psoriasis/Eczema Abdominal Pain-chronic Mood Swings/Depression Phobias Measles/Mumps/Chicken pox TB/Polio/Rheumatic fever Bedwetting Nightmares/Sleep problems Irritable/Bad temper Discipline problems Speech problems Thumb Sucking Anorexia/Bulimia Any developmental delays (eg late walking) School problems Last dental exam: __________ Last eye exam: ____________ BIRTH HISTORY- Please check all that apply Weight at Birth: ____________ Full Term: Was the delivery: Any Pregnancy Complications? Any Problems with the Delivery? Any Problems in the Nursery? While Pregnant did Mother use: Birth Length: ____________ Birth Location: _____________ Yes No If premature, how early? ____________________ Vaginal C-Section Forceps Yes No If yes, explain: ____________________________ Yes No If yes, explain: ____________________________ Yes No If yes, explain: ____________________________ Was child breastfed? Yes How long? __________ Alcohol: Yes No No Drugs: Yes No Cigarettes: Yes No _________________________________________________________________________________________________ _________________________________________________________________________________________________ _________________________________________________________________________________________________ _________________________________________________________________________________________________ PATIENT NAME: ______________________________________________________________ SOCIAL HISTORY- Please circle the appropriate answer Yes No Anyone smoke in the home? Yes No Do parents/caregivers consume Alcohol/Drugs? Yes No Do parents/caregivers have any concerns about Smoking/Alcohol/Drug use by child or his/her peers? Yes No Do parents (or adolescent) have concerns about Sex/Birth Control for adolescent? Yes No Are there any Guns in the house? Are they locked up/out of reach? Yes No Yes No Are all Medicines/Chemicals out of reach? Yes No Is Syrup of Ipecac available in home? Yes No Do parents know CPR? Yes No Does child use seatbelts/car seat every car ride? Do parents? Yes No Yes No Do you have smoke detectors/fire escape plan? Yes No Does child wear helmet when biking/roller blading? Do parents? Yes No FEMALES ONLY-Skip this section if patient is not menstruating. Ever had Pap Smear: Yes No Date of last pap: ____________ Last Menstrual Period: _______________ Flow is: Heavy Moderate Light Flow is: Regular Age at first menses______years old How often are periods? Every ________days. How long are periods? __________days Irregular FAMILY HISTORY-Has any blood relatives suffered from the following? If yes, list who. Heart Murmur _______________ High Blood Pressure _______________ Stroke _______________ Heart Disease _______________ Migraine _______________ Skin Problems _______________ Diabetes _______________ Psoriasis/Eczema _______________ Cancer _______________ Liver Disease/Hepatitis _______________ Arthritis _______________ Lung Disease _______________ Asthma _______________ Tuberculosis _______________ Sickle Cell Dz. _______________ Alcohol/Drug Abuse _______________ Anemia _______________ Mental Illness _______________ Kidney Disease _______________ Depression _______________ Allergies _______________ Thyroid Problems _______________ Glaucoma _______________ HIV/AIDS _______________ MOTHER FATHER BROTHERS & SISTERS NAME ____________________ ____________________ ____________________ ____________________ ____________________ ____________________ ____________________ AGE _____ _____ _____ _____ _____ _____ _____ GENERAL HEALTH Good Poor Deceased __________________ Good Poor Deceased __________________ Good Poor Deceased __________________ Good Poor Deceased __________________ Good Poor Deceased __________________ Good Poor Deceased __________________ Good Poor Deceased __________________ _________________________________________________________________________________________________ _________________________________________________________________________________________________ Signature of person completing form: ________________________/Relationship to child: __________Date: __________ HISTORY REVIEWED BY: _______________________________________________ Signature of Physician/Physician Assistant/ M.A ___/____/____ Date