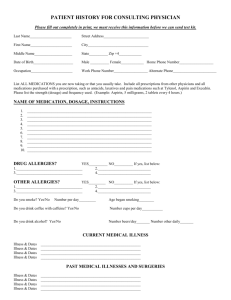
New patient information form
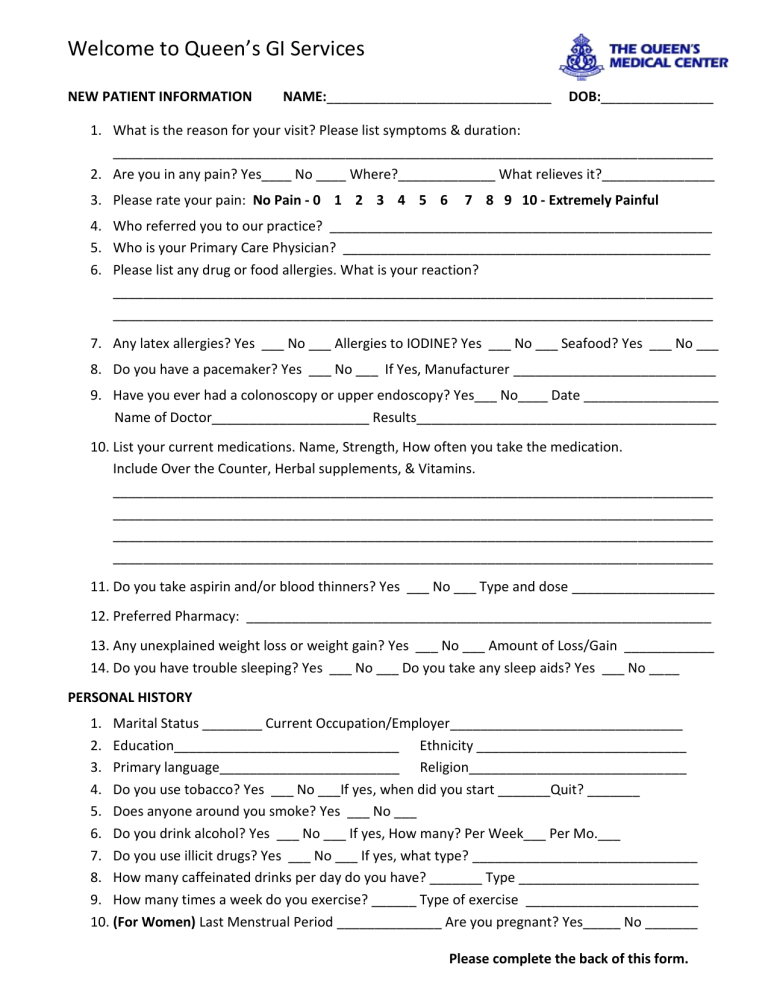
Welcome to Queen’s GI Services
NEW PATIENT INFORMATION NAME:______________________________ DOB:_______________
1.
What is the reason for your visit? Please list symptoms & duration:
________________________________________________________________________________
2.
Are you in any pain? Yes____ No ____ Where?_____________ What relieves it?_______________
3.
Please rate your pain: No Pain - 0 1 2 3 4 5 6 7 8 9 10 - Extremely Painful
4.
Who referred you to our practice? ___________________________________________________
5.
Who is your Primary Care Physician? _________________________________________________
6.
Please list any drug or food allergies. What is your reaction?
________________________________________________________________________________
________________________________________________________________________________
7.
Any latex allergies? Yes ___ No ___ Allergies to IODINE? Yes ___ No ___ Seafood? Yes ___ No ___
8.
Do you have a pacemaker? Yes ___ No ___ If Yes, Manufacturer ___________________________
9.
Have you ever had a colonoscopy or upper endoscopy? Yes___ No____ Date __________________
Name of Doctor_____________________ Results________________________________________
10.
List your current medications. Name, Strength, How often you take the medication.
Include Over the Counter, Herbal supplements, & Vitamins.
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
11.
Do you take aspirin and/or blood thinners? Yes ___ No ___ Type and dose ___________________
12.
Preferred Pharmacy: ______________________________________________________________
13.
Any unexplained weight loss or weight gain? Yes ___ No ___ Amount of Loss/Gain ____________
14.
Do you have trouble sleeping? Yes ___ No ___ Do you take any sleep aids? Yes ___ No ____
PERSONAL HISTORY
1.
Marital Status ________ Current Occupation/Employer_______________________________
2.
Education______________________________ Ethnicity ____________________________
3.
Primary language________________________ Religion_____________________________
4.
Do you use tobacco? Yes ___ No ___If yes, when did you start _______Quit? _______
5.
Does anyone around you smoke? Yes ___ No ___
6.
Do you drink alcohol? Yes ___ No ___ If yes, How many? Per Week___ Per Mo.___
7.
Do you use illicit drugs? Yes ___ No ___ If yes, what type? ______________________________
8.
How many caffeinated drinks per day do you have? _______ Type ________________________
9.
How many times a week do you exercise? ______ Type of exercise _______________________
10.
(For Women) Last Menstrual Period ______________ Are you pregnant? Yes_____ No _______
Please complete the back of this form.
Medical history: Please indicate chronic conditions or if you are currently experiencing:
CONSTITUTIONAL:
Change in activity
Change in appetite
Chills
Night sweats
HENT:
Hearing loss
Sinus problems
Dental problems
Dentures/Partials
EYES:
Visual changes
Fatigue
Fever
Unexpected weight change
Mouth sores
Sore throat
Trouble swallowing
Voice change
Eye problems
RESPIRATORY:
Sleep Apnea
CPAP machine use
Cough
Shortness of breath
Wheezing
Asthma
CARDIOVASCULAR:
Chest pain
Leg swelling
Heart disease
Defibrillator/Pacemaker
Palpitations Heart murmur
High blood pressure Heart surgery
GASTROINTESTINAL:
Poor appetite Constipation
Difficulty swallowing Diarrhea
Heartburn/Indigestion Nausea/Vomiting
Acid Reflux Rectal pain
Ulcer
Abdominal bloating
Abdominal pain
Rectal bleeding
Blood in stool
Hemorrhoids
Rectal soiling/leakage
Liver problems
Colon/stomach polyps
Hernia
ENDOCRINE:
Diabetes
Thyroid problems
Hypoglycemia
GENITOURINARY:
Painful urination
Bloody urine
Kidney problems
Frequent urination
Genital lesions
MUSCULOSKELETAL:
Joint pain
Back pain
Muscle weakness
Muscle pain
SKIN:
Rashes
Lesions or wounds
Skin problems
Jaundice
NEUROLOGIC:
Headaches
Numbness
Seizures
HEMATOLOGIC:
Bleeding problems
Bruises easily
Loss of consciousness
Weakness
Stroke
Enlarged lymph nodes
Anemia/Low blood count
PSYCHIATRIC:
Depression
Anxiety
Mental disturbance
Sleep disturbance
INFECTIONS:
Hepatitis (Type:___) Tuberclosis (TB)
HIV
MRSA
AIDS
Stool C-Diff
Do you have a history of cancer? Yes ___ No ___
Type:________________________________________
Please list any surgeries:
_____________________________________________
_____________________________________________
_____________________________________________
Have you ever had any problems with anesthesia?
Yes ______ No ______
Medical Problems:(i.e. Diabetes, High Blood Pressure):
_____________________________________________
_____________________________________________
_____________________________________________
Family History
Mother:
Living ___ Deceased ___ Illness___________________
Father:
Living ___ Deceased ___ Illness___________________
Sisters: How many? _____
Living ___ Deceased ___ Illness___________________
Brothers: How many? ____
Living ___ Deceased ___ Illness___________________
Children: How many?_____
Living ___ Deceased ___ Illness___________________
Does anyone in your family have a history of cancer, bowel disease, or autoimmune illness?
_____________________________________________
_____________________________________________
Thank you for taking the time to complete this form.