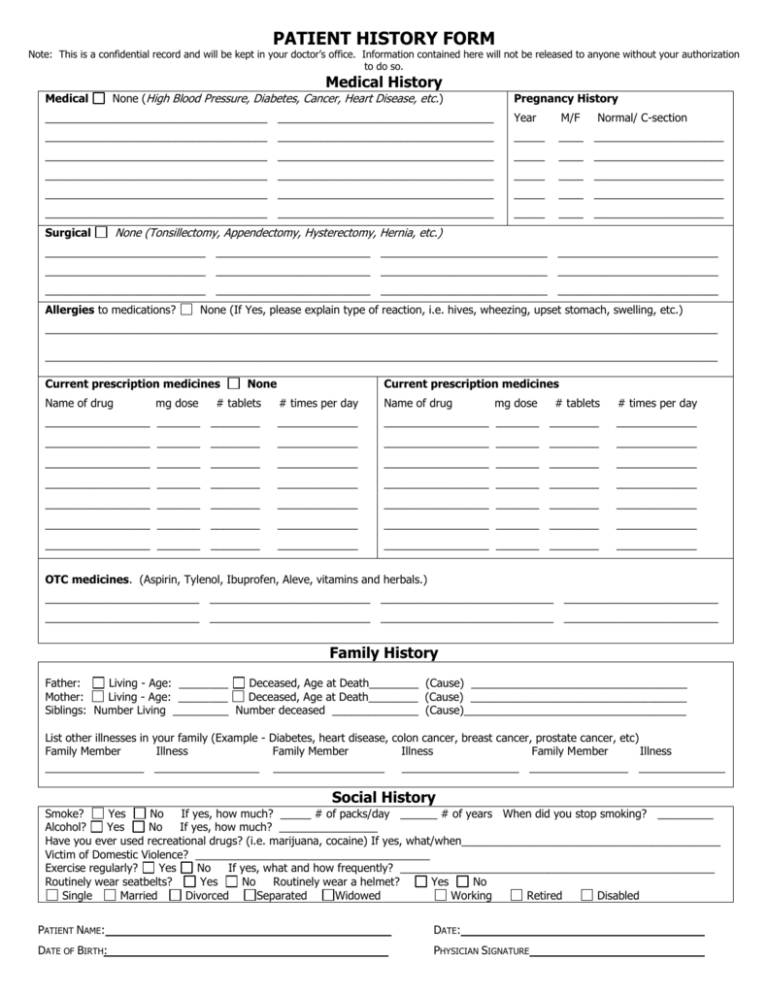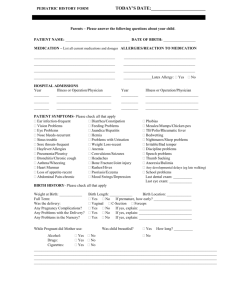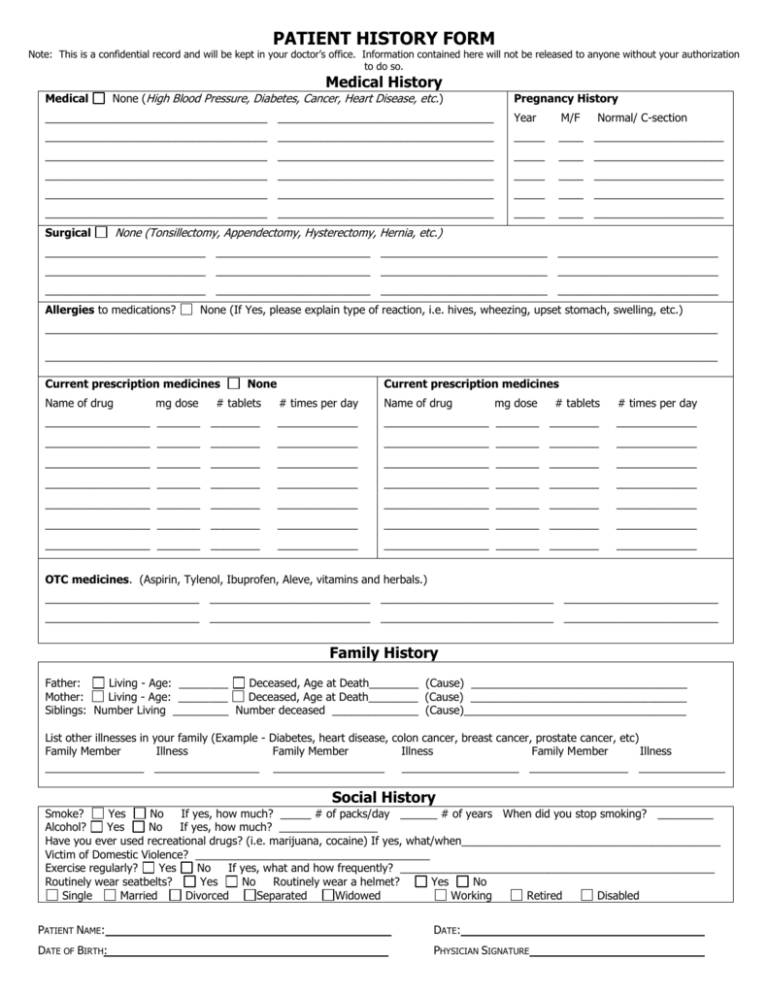
PATIENT HISTORY FORM
Note: This is a confidential record and will be kept in your doctor’s office. Information contained here will not be released to anyone without your authorization
to do so.
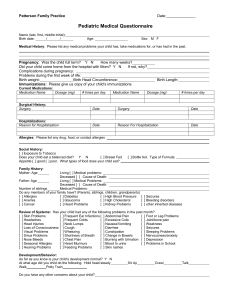
Medical History
Medical
None (High Blood Pressure, Diabetes, Cancer, Heart Disease, etc.)
Pregnancy History
____________________________________ ___________________________________
Year
M/F
____________________________________ ___________________________________
_____
____ _____________________
____________________________________ ___________________________________
_____
____ _____________________
____________________________________ ___________________________________
_____
____ _____________________
____________________________________ ___________________________________
_____
____ _____________________
____________________________________ ___________________________________
_____
____ _____________________
Surgical
Normal/ C-section
None (Tonsillectomy, Appendectomy, Hysterectomy, Hernia, etc.)
__________________________ _________________________ ___________________________ __________________________
__________________________ _________________________ ___________________________ __________________________
__________________________ _________________________ ___________________________ __________________________
Allergies to medications?
None (If Yes, please explain type of reaction, i.e. hives, wheezing, upset stomach, swelling, etc.)
_____________________________________________________________________________________________________________
_____________________________________________________________________________________________________________
Current prescription medicines
Name of drug
mg dose
None
Current prescription medicines
# tablets
# times per day
Name of drug
# tablets
# times per day
_________________ _______ ________
_____________
_________________ _______ ________
mg dose
_____________
_________________ _______ ________
_____________
_________________ _______ ________
_____________
_________________ _______ ________
_____________
_________________ _______ ________
_____________
_________________ _______ ________
_____________
_________________ _______ ________
_____________
_________________ _______ ________
_____________
_________________ _______ ________
_____________
_________________ _______ ________
_____________
_________________ _______ ________
_____________
_________________ _______ ________
_____________
_________________ _______ ________
_____________
OTC medicines. (Aspirin, Tylenol, Ibuprofen, Aleve, vitamins and herbals.)
_________________________ __________________________ ____________________________ _________________________
_________________________ __________________________ ____________________________ _________________________
Family History
Father:
Living - Age: ________
Deceased, Age at Death________ (Cause) ___________________________________
Mother:
Living - Age: ________
Deceased, Age at Death________ (Cause) ___________________________________
Siblings: Number Living _________ Number deceased ______________ (Cause)____________________________________
List other illnesses in your family (Example - Diabetes, heart disease, colon cancer, breast cancer, prostate cancer, etc)
Family Member
Illness
Family Member
Illness
Family Member
Illness
________________ _________________ __________________
___________________ ________________ ______________
Social History
Smoke?
Yes
No
If yes, how much? _____ # of packs/day ______ # of years When did you stop smoking? _________
Alcohol?
Yes
No
If yes, how much? ________________
Have you ever used recreational drugs? (i.e. marijuana, cocaine) If yes, what/when__________________________________________
Victim of Domestic Violence? ______________________________________
Exercise regularly?
Yes
No
If yes, what and how frequently? ___________________________________________________
Routinely wear seatbelts?
Yes
No
Routinely wear a helmet?
Yes
No
Single
Married
Divorced
Separated
Widowed
Working
Retired
Disabled
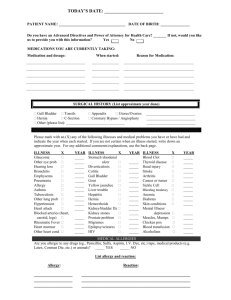
PATIENT NAME:
DATE:
DATE OF BIRTH:
PHYSICIAN SIGNATURE
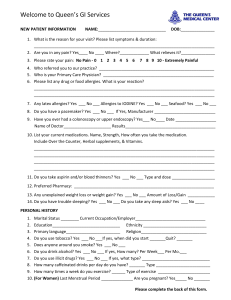
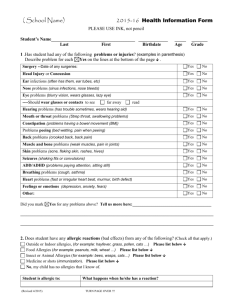
Review of Systems
Do you now or have you had any problems related to the following systems?
Circle Yes or No.
Constitutional Symptoms
Weight change
Y
Chills/Fever/night sweats
Y
Sleep Problems
Y
Have you gotten shorter?
Y
Other
Eyes
Double vision
Glaucoma
Cataracts
Other
Ear/Nose/Throat/Mouth
Hearing changes
Sore throat
Sinus problem
(Comments)
N
N
N
N
Y
Y
Y
N
N
N
Y
Y
Y
N
N
N
Y
Y
Y
Y
Y
N
N
N
N
N
Y
Y
Y
N
N
N
Y
N
Other
Cardiovascular
Chest pain
Irregular heartbeat
Swelling in ankles
High blood pressure
Heart attack
Other
Psychologic
Are you generally happy?
Do you feel depressed?
Do you feel anxious?
Do you feel safe in your
home?
Genitourinary
Change in stream
Nocturia (getting up at night)
Urinary frequency > 8 times/day
Burning with urination
Other:
Musculoskeletal
Bone pain
Muscle pain
Joint pain
Other
Integumentary (Skin)
Rash
Lumps or bumps
Moles, skin tags
Skin cancer
Other
Neurological
Tremors
Dizziness/ Vertigo
Numbness/tingling
Stroke/TIA
(Comments)
Y
Y
Y
Y
N
N
N
N
Y
Y
Y
N
N
N
Y
Y
Y
Y
N
N
N
N
Y
Y
Y
Y
N
N
N
N
Y
Y
Y
N
N
N
Y
Y
Y
Y
N
N
N
N
Y
N
Other
Respiratory
Wheezing /Asthma/ COPD
Frequent cough
Shortness of breath
Other
Endocrine
Excessive thirst
Too hot/cold
Tired/sluggish
Other
Hematologic/Lymphatic
Swollen glands
Blood clotting problem
Bruising
Transfusion
Other
Allergic/Immunologic
Hay Fever
Drug allergies
Food allergies
Other
Y
Y
Y
N
N
N
Other:
Sexual History
Y
Y
Y
Y
N
N
N
N
Y
Y
Y
N
N
N
Immunizations:
Date of last Tetanus________________________
Date of last Flu Shot_______________________
Date of last Pneumonia Shot_________________
Physician comments:
Patient Name
Gastrointestinal
Abdominal pain
Nausea/vomiting
GERD / Ulcers
Constipation/Diarrhea/Blood in
stools
Sexual problems?
Other (i.e. sexual trauma)
Exams
Date of Last Dental Exam ______________________________
Date of Last Eye Exam _________________________________
Women:
Date of Last Period___________________________________
Date of Last Pap ____________________________________
Date of Last Mammogram ____________________________
Men:
Date of Last Prostate Exam ____________________________
DOB