Guidelines for the diagnosis of infective endocarditis
advertisement

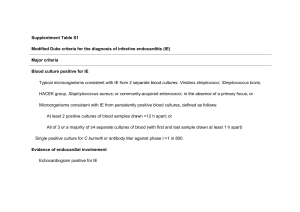
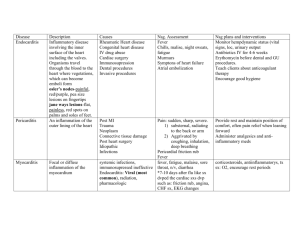
Guidelines for the diagnosis of infective endocarditis Infective endocarditis is a rare condition that is often initially missed as a diagnosis. It is a serious condition and 1 in 6 patients will die in hospital. It is important to have infective endocarditis as a differential in patients presenting with sepsis, particularly those who are at higher risk. It typically no longer presents with classical peripheral stigmata. Whereas traditionally endocarditis was caused by oral bacteria, staphylococcus aureus is increasingly common. The most reliable clinical symptoms and signs are: o o o o o o o Fever. Chills. Poor appetite. Weight loss. A heart murmur. No other obvious focus of infection. Recurrent infection after shorter courses of antibiotics for presumed sepsis elsewhere. o Sepsis in the context of an embolic event, e.g. a stroke. Patients typically have raised inflammatory markers and a mild anaemia. The white cell count may be normal or minimally elevated in many cases. Patients will often have risk factors for infective endocarditis: o o o o o o o Known valvular heart disease. Valve replacement. Congenital heart disease. Previous infective endocarditis. Hypertrophic cardiomyopathy. Permanent pacemaker or other device. Recent central line insertion or other indwelling device. A urine dipstick may show haematuria. Presentation may be immunocompromised Blood cultures are the key to diagnosis. even more subtle in the elderly and o In patients who are acutely septic two sets of blood cultures, taken at different times within an hour before the start of empirical treatment should be taken. o In relatively well patients, antibiotics should be delayed pending investigation. o Three sets of blood cultures should be taken but with at least 6 h between sampling times; the aim is to demonstrate the presence of sustained or persistent bacteraemia. o Meticulous aseptic technique is required to avoid contamination with skin commensals. Guidance on blood culture collection is on the infection control pages of the Trust intranet. o The volume of blood collected is also important: the bottles should be properly filled. o There is no need to collect successive blood cultures from separate sites. o Positive blood cultures from a single set out of a series should be interpreted with caution. o Cultures should be collected from peripheral veins, not indwelling vascular devices, unless paired collections are made to diagnose catheter-related bloodstream infection. o If blood cultures remain negative after 48 hours, consider repeating a further 3 sets of blood cultures and take clotted blood for serological investigation, e.g. Q fever, Bartonella. Consider fungal IE, especially if immunocompromised. o Where the diagnosis of IE is suspected in patients already on antibiotics, consideration should be given to discontinuing them to obtain viable bacteria from blood cultures. Antibiotics may need to be discontinued for 7-10 days before cultures become positive. o If the patient remains febrile after seven days of treatment, cultures should be repeated. Transthoracic echocardiography should be considered where o Blood cultures are positive for an organism that typically causes IE and there are other features to suggest endocarditis or risk factors for endocarditis, or no other obvious source of infection. o The patient has a persistent inflammatory state and no other cause has been found. o Blood cultures are negative, but there are strong clinical grounds to suspect infective endocarditis. o Note that transthoracic echocardiography is neither 100% sensitive or specific and a normal transthoracic echocardiogram does not exclude endocarditis. o Transoesophageal echocardiography may be considered after a transthoracic echo after discussion with a cardiologist. The detailed management of infective endocarditis is beyond the scope of this guideline, but links can be found below. The trust policy for antibiotic usage in patients with infective endocarditis (either suspected or confirmed) can be found here. o Patients with suspected infective endocarditis do not necessarily need immediate antibiotics unless clinically unwell and advice should be sought from the infection specialists and/or cardiologists before commencing antibiotics. o Patients may be started on antibiotics prior to a definitive diagnosis if blood cultures are positive, after discussion with the infection specialist. o All cases of confirmed endocarditis should be managed by the cardiologists on Fielding ward/CCU in conjunction with the infection specialists. Further reading o BSAC 2011 Guidelines for Infective Endocarditis o ESC 2009 Guidelines for Infective Endocarditis o The Modified Duke Criteria