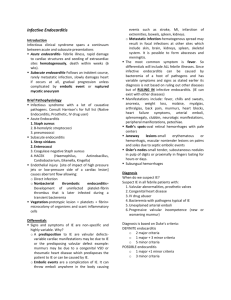
Endocarditis
advertisement

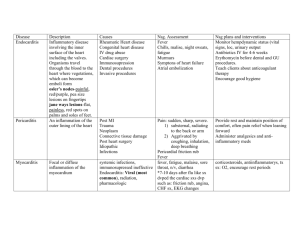
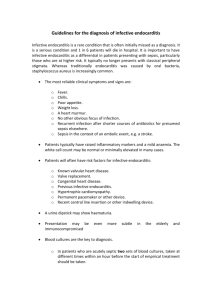
Endocarditis & Endovascular Infections Thomas Hawn, ID Fellows Course, July 2009 I. Diagnosis A. Differential Diagnosis of Infective Endocarditis (Berbari et al., 1997): A. associated with neoplasms: atrial myxoma, marantic (adenoCa), carcinoid B. associated with autoimmune: rheumatic heart disease, SLE (Libman-Sacks endocarditis), anti-phospholipid syndrome, polyarteritis nodosa, Behcet’s disease C. Postvalvular operation: thrombus, sutures D. Other: eosinophilic heart disease, ruptured mitral chordae, myxomatous degeneration B. Microbiology 1. Etiologic agents: Streptococci 60-80%: viridans 30-40%, enterococi 5-18%, other 15-25% Staphylococci 20-35%: coag positive 10-27%, coag negative 1-3% Gram-negative aerobic bacilli: 1.5-13% Fungi 2-4%, Culture negative <5-24% 2. Ratio of infective endocarditis cases to non-endocarditis bacteremia for various pathogens: S. mutans 14.2:1, S. bovis 5.9:1, S. sanguis 3:1, S. mitior 1.8:1, E. faecalis 1:1.2, S. anginosus 1:2.6, Grp G strep 1:2.9, Grp B strep 1:7.4, Grp A strep 1:32. C. Diagnostic criteria of Infective Endocarditis Table I: Modified Duke Clinical Criteria for Diagnosis of IE (Baddour et al., 2005; Durack et al., 1994) _____________________________________________________________________________________ Definite IE Pathological criteria: Microorganisms: demonstrated by culture or histology in a vegetation, in a vegetation that has embolized, or in an intracardiac abscess, or Pathologic lesions: vegetation or intracardiac abscess present, confirmed by histology showing active endocarditis. Clinical criteria, using specific definitions in Table 2 2 major criteria, or 1 major and 3 minor criteria 5 minor criteria Possible IE 1 major and 1 minor criteria 3 minor criteria Rejected Firm alternate diagnosis for manifestations of endocarditis Resolution of manifestations of endocarditis with antibiotic therapy for < 4 days, or No pathological evidence of IE at surgery or autopsy, after antibiotic therapy for < 4 days. Does not meet criteria for possible IE ______________________________________________________________________________________ Table II: Definitions of terms used in the Modified Duke criteria for the diagnosis of IE ______________________________________________________________________________________ Major criteria 1. Positive blood culture for IE A. Typical microorganism consistent with IE from 2 separate blood cultures as noted below: Viridans streptococci (including nutritionally variant strains (Abiotrophia species), Streptococcus bovis, HACEK group, Staphylococcus aureus or community-acquired enterococci, in the absence of a primary focus B. Microorganisms consistent with IE from persistently positive blood cultures as defined as (i) ≥2 positive cultures of blood samples drawn >12 hours apart (ii) all of 3 or a majority of ≥4 separate cultures of blood (with the first and last samples drawn ≥1 hour apart) (iii) single positive blood culture for Coxiella burnetti or anti-phase 1 IgG antibody titer >1:800 2. Evidence of endocardial involvement A. Positive echocardiogram* for IE defined as (i) oscillating intracardiac mass on valve or supporting structures, in the path of regurgitant jets, or on implanted material in the absence of an alternative anatomic explanation, or (ii) abscess, or (iii) new partial dehiscence of prosthetic valve, or B. New valvular regurgitation (worsening or changing or pre-existing murmur not sufficient) * TEE recommended for pts with prosthetic valve, those rated “possible IE” by clinical criteria, and those with complicated IE (i.e. paravalvular abscess). TTE recommended for remainder. Minor criteria 1. Predisposition: predisposing heart condition or intravenous drug use 2. Fever: temperature ≥ 38.0 C 3. Vascular phenomena: major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhage, and Janeway lesions (nontender, erythematous or hemorrhagic, macular or nodular lesions on pads of fingers/toes or palm/sole). 4. Immunologic phenomena: glomerulonephritis, Osler’s nodes (painful, nodular lesions often on pads of fingers/toes), Roth spots (oval, pale retinal lesions surrounded by hemorrhage), and rheumatoid factor 5. Microbiological evidence: positive blood culture but does not meet a major criteria as noted above or serologic evidence of active infection with organism consistent with IE (excludes single positive cultures for coagulase-negative Staphylococci and organisms that do not cause endocarditis). ______________________________________________________________________________________ D. Comments on the diagnosis of IE 1. Compared to the older von Reyn criteria from 1981 (Beth Israel criteria), the Duke criteria have improved sensitivity. Major changes included the addition of echocardiographic findings to the diagnosis, inclusion of IVDU as a risk factor, emphasis on blood cultures from organisms that are typical for IE (viridans strep, S. bovis, HACEK), or community acquired Staph aureus or enterococci, and the absence of a primary focus. (Heiro et al., 1998) 2. For 69 cases of pathologically proven IE, the sensitivity of the von Reyn criteria was 51% while it was 80% for the Duke criteria (for the the diagnosis of Definite IE). If both “Definite and Possible” endocarditis are included, then the sensitivity is 100%. The negative predictive value for the rejected category is >98%. Hard to assess specificity since the number of cases who do not have endocarditis is difficult to accurately determine (Durack et al., 1994). 2. Fever present in 87% of Durack’s cases—although a helpful criteria, its absence does not rule out IE. 3. Vascular phenomena—splinter hemorrhages and petechiae are not part of the criteria since they are thought to be nonspecific. 4. Li et al (2000) proposed modifications to the Duke criteria that were incorporated by the AHA in 2005 (Baddour et al., 2005; Li et al., 2000). These recent changes included: a. To increase specificity, the category “possible IE” was changed to cases with 1 major and 1 minor criteria or 3 minor criteria. b. S. aureus bacteremia became a major criteria regardless of the source (community or nosocomial) c. Eliminate the ECHO minor criteria since TEE’s are more widely used now d. Add Coxiella to list of major criteria (a single positive blood culture or antiphase I IgG antibody titer > 1:800). e. Use TEEs as initial test in pts with prosthetic valves, a suspected complicated IE (such as perivalvular abscess), and those in the “possible IE” category. TTE as initial test for all others. F. Diagnosis of unusual pathogens & work-up for culture-negative endocarditis (Berbari et al., 1997) Table III Exposure Epidemic Birds Nosocomial, immuosuppression EtOHism, homeless Animals STD, sexually active Common pathogens Legionella C. psittaci Fungi Bartonella quintana Coxiella burnetti Brucella species Neisseria gonorrhea Diagnostic methods Special instructions to lab to culture for fastidious organisms—subculture to BCYE media, consider urinary antigen for L. pneumophilia Complement fixation, ELISA Extended incubation of blood cultures Fastidious organism bld cx with subculture to chocolate agar CFA titers to phase I & II antigens Bld cx with lysis centrifugation, serology Bld cx. Commercial systems may contain polyanetholesulfonate which inhibits Neisseria. A recent series of 348 subjects with blood culture negative endocarditis from France: 167 (48%) were Coxiella burnetti, 99 (28%) were Bartonella (Houpikian and Raoult, 2005). II. Risk Factors & Prevention 1. What are risk factors for IE? (Steckelberg and Wilson, 1993) Baseline incidence in general population is 4.9/100,000 person years. Conditions with increased risk: prior endocarditis 740/100,000; congenital heart disease: overall 120, VSD 220 with medical management, VSD with surgical management 60, aortic stenosis 180, pulmonic stenosis 20, prosthetic cardiac valve 308-383, rheumatic heart disease 440, mitral valve prolapse with murmur 52, MVP without murmer 4.6. For prevention of endocarditis during procedures, see AHA recommendations (Dajani et al., 1997). 2. Are recent dental procedures a risk factor? Controversial. Historically, dental procedures have been implicated as a risk factor for endocarditis. New AHA guidelines include re-evaluation of the data and argues that dental treatment is not a major risk factor for IE. In one case-control study with 546 subjects. Dental treatment was no more frequent than controls in the preceding 3 months (Strom et al., 1998). Estimates of the cumulative exposure to bacteremia indicates that daily activities lead to a much greater burden of bacteremia than dental procedures. Cumulative exposure of annual bacteremia (CE)=PxIxTxF, where P=prevalence of bacteremia expressed as a percentage prevalence related to the procedure, I=intensity of bacteremia in cfu/ml; T=length of bacteremia in minutes; f=frequency of bacteremia events in one year. Risk of cumulative exposure to bacteremia in one year (CFU minutes per ml per year) compared to tooth extraction (Roberts, 1999): Table IV ____________________________________________________________________________________________________ Risk relative to a tooth extraction Tooth extraction (permanent tooth) 1 Flossing 365,000 Dental exam 222 Brushing teeth 702,556 Mucoperiosteal surgery ~5555 Chewing 136,778 Baseline activities of daily life 1,693,556 NT tube 166 2. Prevention of endocarditis (Wilson et al., 2007) New 2007 guidelines have dramatically altered the 1997 recommendations. 1997 guidelines stratified individuals into risk categories by host risks and procedural risks and then made recommendations. The 2007 guidelines emphasize that most IE occurs as a result of sporadic, transient bacteremias associated with daily living rather than procedures. Hence, the benefits of prophylaxis for medical procedures is unlikely to be significant. Summary of major changes: 1. more limited set of cardiac conditions are recommended for prophylaxis (no longer recommended for MVP with regurgitation, RHD, and more limited #of CHD. 2. simplified list of which procedures qualify (no GU/GI, criteria for dental procedure straightforward) Table V ___________________________________________________________________________________________________ Cardiac conditions associated with highest risk from IE & for which prophylaxis is recommended: 1. Prosthetic cardiac valve 2. Previous IE 3. Congenital Heart Disease: A. unrepaired cyanotic CHD, including palliative shunts & conduits B. Completely repaired CHD with prosthetic material or device, during the first 6 months after the procedure C. Repaired CHD with residual defects at the site or adjacent to the site of a prosthetic patch or device 4. Cardiac transplant recipients who develop cardiac valvulopathy Procedures for which endocarditis is recommended for the above categories of patients: 1. All dental procedures that involve manipulation of gingival tissue or the periapical region of teeth or perforation of the oral mucosa. 2. Respiratory tract or infected skin/soft tissue procedures 3. NOT recommended for GU or GI procedures solely to prevent IE Oral Regimens for a dental procedure: Amoxicillin 2g po 30-60 min prior to procedure If allergic to PCN or ampicillin: Cephalexin 2g or Clindamycin 600 mg or azithromycin/clarithromycin 500 mg ____________________________________________________________________________________________________ III. Treatment Table VI: Treatment of Endocarditis (Baddour et al., 2005) ______________________________________________________________________________________ A. i. ii. iii. iv. Viridans streptococci & S. bovis, PCN susceptible (MIC ≤0.12 g/ml) PCN G 12-18 mU iv/day x 4 wks, ceftriaxone 2g iv or im qd x 4 wks, PCN G 12-18 mU iv qd + gentamicin 3 mg/kg iv qd x 2 wks, vancomycin 1g iv bid x 4 wks (for -lactam allergic pts) B. Viridans Streptococci & S. bovis, relatively resistant to PCN (MIC > 0.12 g/ml & ≤ 0.5 g/ml) i. PCN G 24 mU iv/day x 4 wks + gentamicin 3 mg/kg iv qd x 2 wks ii. ceftriaxone 2g iv/day x 4 wks + gentamicin 3 mg/kg iv qd x 2 wks ii. vancomycin 1g iv bid x 4 wks (for -lactam allergic pts) C. Enterococci, Abiotrophia defective, Granulicatella species, & Viridans strep with PCN MIC >5 g/ml i. PCN G 18-30 mU iv/day x 4-6 wks + gentamicin 1 mg/kg iv q8h x 4-6 wks ii. ampicillin 12 g/day iv divided in 6 doses x 4-6 wks + gentamicin 1 mg/kg iv q8h x 4-6 wks iii. vancomycin 1g iv bid x 6 wks (for -lactam allergic pts) + gentamicin 1 mg/kg iv q8h x 6 wks D. Staphylococcus in the absence of prosthetic material MSSA: i. nafcillin or oxacillin 2g iv q4h + option of adding gentamicin 1 mg/kg iv q8h ii. cefazolin 2g iv q8h + option of adding gentamicin 1 mg/kg iv q8h iii. vancomycin 1g iv bid x 6 wks x 3-5 days x 6 wks x 3-5 days x 6 wks (for -lactam allergic pts) MRSA: vancomycin 1g iv bid x (for -lactam allergic pts) E. Staphylococcus in the presence of prosthetic material MSSA: nafcillin or oxacillin 2g iv q4h + rifampin 300 mg iv/po q8h + gentamicin 1 mg/kg iv q8h MRSA: vancomycin 1g iv bid + rifampin 300 mg po q8h + gentamicin 1 mg/kg iv q8h 6 wks x > 6 wks x > 6 wks x 2 wks x 4-6 wks x > 6 wks x 2 wks F. HACEK organisms i. ceftriaxone 2g iv/im qd x 4 wks (or other 3rd or 4th gen. ceph.) ii. ampicillin-sulbactam 12g iv/day divided in 4 doses x 4 wks iii. ciprofloxacin 500 mg po bid or 400 mg iv bid x 4 wks ______________________________________________________________________________________ IV. Management of Complications A. Prognostication: How accurately can mortality be predicted based on presenting features? Hasbun et al (2003) (Hasbun et al., 2003) Retrospective observational cohort study. N=513 with left-sided native valve endocarditis. Relative risk of unadjusted association of variables and 6 –month mortality: Immunocompromosed: relative risk=1.86 (95% CI= 1.23-2.59), fever 1.62 (1.04-2.30), mental status 2.26 (1.49-3.06), CHF 2.09 (1.39-2.92), aortic valve vs. other 1.41 (0.92-2.02), vegetation absent vs. present 1.02, disabling emboli 1.25 (0.711.97), 0-1 vs. >2 emboli 0.79, blood culture with pathogen other than Viridans strep 4.26, pathogen other than S. aureus 1.59 (1.04-2.25), pathogen other than Enterococcus 1.87 (1.12-2.71), medical treatment only 2.12 (1.29-3.16) Adjusted analysis revealed 5 independent variables: Mental status 1.98 (1.14-2.93), comorbidity score 1.76, CHF 1.91, medical Rx 2.45, Microbiology: Staph aureus 3.56; bug other than Viridans strep 4.87. B. Embolization 1. Embolization Risks: Occurs in 22-50% of cases. Highest risk occurs with aortic and mitral valve infections, IE due to S. aureus, Candida, HACEK, and Abiotrophia organisms. Greatest risk is during the 1st 2 wks (13 events per 1000 patient days compared to <1.2) 2. Prediction of embolization: Very difficult to predict which individuals will have emboli. Size of vegetation on Echo has not been uniformaly helpful in predicting embolization. Some studies suggest that vegetations > 1 cm have a higher risk of embolization, but others have not confirmed this. The highest rate of emboli was seen with vegetations on the anterior leaflet of the mitral valve. An increase in size of vegetations after 4-8 weeks of therapy increased the risk of emboli in one study. C. Congestive Heart Failure: CHF indicates a poor prognosis if medical therapy alone is employed and is also a powerful predictor of poor surgical outcome. Delaying surgery to the point of decompensation increases mortality (from 6-11% to 17-33%). D. Indications for valve surgery: Table VII: Features suggesting potential need for surgical intervention ______________________________________________________________________________________ Vegetation Persistent vegetation after systemic embolization: Anterior mitral leaflet vegetation, particularly >1 cm One or more embolic events during the 1st 2 wks of therapy 2 or more embolic events during or after antimicrobial therapy (not cutaneous) Increase in vegetation size after 4 weeks of antimicrobial therapy Valvular dysfunction Acute aortic or mitral insufficiency with signs of ventricular failure Heart failure unresponsive to medical therapy Valve perforation or rupture Perivalvular extension Valvular dehiscence, rupture, or fistula New heart block Large abscess, or extension of abscess despite appropriate antimicrobial therapy. ______________________________________________________________________________________ E. Mycotic Aneurysms Extracranial Most are asymptomatic. Surgical intervention is strongly advised. Intracranial See below. F. Management of Neurologic Complications of Infective Endocarditis Questions: -Should neurologic complications from IE affect the timing of cardiovascular surgery? -Should patients with IE be screened for cerebral mycotic aneurysms? 1. Background Central nervous system complications occur in 20-40% of patients with infective endocarditis. The types of complications compiled from 1014 patients from several different studies include: embolus (13.4%), meningitis (7.0%), encephalopathy (6.4%), headache (3.7%), hemorrhage (3.6%), seizure (3.5%), abscess (1.9%), mycotic aneurysm (1.5%) (Tunkel, 1993). 2. When should cardiac surgery be performed in patients with neurologic complications from IE? There is general agreement that cerebral hemorrhage is associated with a higher risk of peri-operative mortality and post-operative stroke. However, for other types of CNS complications the data is not as clear. Four studies have addressed the question with 2 studies favoring waiting at least 2 weeks and 2 others finding no difference in immediate versus delayed surgery. The best data on this question is from Eishi et al who found that a delay in cardiac surgery resulted in a lower complication rate (Eishi, 1995). Eishi retrospectively evaluated 181 patients with cerebral complications of IE. For pts with cerebral infarction (n=68), the mortality rate and cerebral complication rate decreased when surgery was delayed: 66.3% & 45.3% for surgery at less than 24h, 31.3% & 43.8% at 2-7 days, 16.7% &16.7% at 8-14 days, 10% &10% at 15-21 days, 26.3% &10.5% at 22-28 days, and 7.0% &2.3% for those operated after 4 weeks. For patients with hemorrhagic infarction, the complication rate remained high at 4 weeks (19% with complications). Ting et al found that only preoperative hemorrhage was associated with mortality and postoperative stroke (Ting, 1991). However, a large percentage of these patients were asymptomatic. By comparison, all of the subjects in Eishi’s study were symptomatic. Summary: While there are no prospective randomized trials to assess this question, there is some data to suggest that waiting 2 weeks for cardiac surgery improves the outcome of pts with cerebral infarcts associated with septic emboli. 3. Should patients with IE be screened for cerebral mycotic aneurysms? Intracranial mycotic aneurysms (ICMA) occur in around 1.2 to 5% of pts with IE. The incidence of ICMA in asymptomatic versus symptomatic patients is not known. Mortality varies from 30% for unruptured to 80% for ruptured ICMAs. Expert opinion suggests that (Baddour et al., 2005): 1) In the absence of clinical signs or symptoms of ICMAs, routine screening with imaging studies is not warranted. 2) Imaging procedures to detect ICMAs are indicated for those with sxs (localized or severe HA, sterile meningitis, or focal neurological signs). Conventional angiography remains the gold standard although the sensitivity of MRAs is good for aneurysms greater than 5mm. 3) Treatment of detected aneurysms: 37% will heal on antibiotics alone (Bingham, 1977). There are no data which can prospectively identify pts at risk for imminent rupture. Some guidelines for deciding on surgical intervention include: a) a single ICMA distal to the first bifurcation of a major artery (i.e. MCA) should be monitored with serial angiograms and excised promptly if it enlarges or bleeds. b) ICMAs proximal to the first bifurcation are less amenable to surgery. c) If cardiac valve replacement is indicated, a bioprosthetic valve may be preferred to avoid anti-coagulation. Due to the paucity of data in this area, it is difficult to assess the wisdom of these recommendations. Data clearly shows that some aneurysms will resolve with medical therapy alone. Based on this, it seems reasonable to not screen asymptomatic individuals with the intent to perform immediate surgery. However, it may be worthwhile to do so for establishing a baseline and influencing the length of treatment (i.e., treat with antibiotics until the aneurysm resolves). V. Endovascular Catheter-Related Infections A. Diagnosis (Mermel et al., 2009) If an intravascular central venous catheter (CVC)-related infection is suspected: 1. 2 sets of blood cultures, with one drawn percutaneously, should be obtained (AII) 2. Paired quantitative blood cultures or paired qualitative blood cultures with a continuously monitored differential time to positivity are recommended for the diagnosis, especially if the long term catheter cannot be removed (AII) (Siegman-Igra et al., 1997). 3. If the catheter is removed, quantitative or semi-quantitative cultures of the catheter are recommended (AII) (criteria for positivity >15 CFU per catheter by semi-quantitative method, >100 CFU by quantitative method). Culture of catheters should only be done when an infection is suspected For paired quantitative blood cultures, if the colony count is at least 3-fold greater from the catheter compared to the vein, then it is predictive of a catheter related infection. For unpaired quantitative blood cultures, >100 CFU/ml is predictive of a catheter infection. For differential time to positivity, a 2 hour time difference predicts a catheter infection. Data (Blot et al., 1999; Blot et al., 1998; Gaur et al., 2003; Mermel et al., 2001; O'Grady et al., 2002; Siegman-Igra et al., 1997) Paired quantitative Unpaired quantitative Sens 79 78 Spec 94 96 Reference and notes Siegman-Igra, meta-analysis (cath:vein ratio>3-10:1) Siegman-Igra, meta-analysis (CFU/ml>15-100) Differential time to positivity 89 96 94 100 100 91 Gaur et al, n=33 (time>120 minutes) Blot et al (1998), n=64, (time > 120 minutes) Blot et al (1999), n=28, (time > 120 minutes) B. Management (see IDSA guidelines) (Mermel et al., 2001; O'Grady et al., 2002): Removable CVC 1. For extraluminal infections (tunnel infections, port abscess), remove line and treat with antibiotics for 10-14 days. For intraluminal infections: 2. Is if a complicated or uncomplicated infection? Complicated infections might have persistent bacteremia, septic emboli, endocarditis. If complicated, remove line and treat for extended period (depending on complications and organism, generally at least 4-6 weeks). 2. For uncomplicated luminal infections: a. S. aureus: remove CVC, Rx for 14 days, strongly consider TEE. b. Gram negative: Remove CVC, Rx for 14 days. c. Candida: remove CVC, Rx for 14 days d. Coagulase-negative staphylococcus: consider retaining catheter and treating with systemic antibiotic + antibiotic lock therapy for 10-14 days. If catheter is removed, treat for 5-7 days. Tunneled CVC or implantable device 1. For extraluminal infections (tunnel infections, port abscess), remove line and treat with antibiotics for 10-14 days. For intraluminal infections: 2. Complicated: same as above. 3. For uncomplicated luminal infections: The guidelines are similar to those for removable lines. The difference lies in the strength of the recommendation and degree of insistence on CVC removal. There is acknowledgement that some clinicians will strongly prefer to attempt to salvage the CVC without removal. a. S. aureus: Primary rec: remove CVC, Rx for 14 days, strongly consider TEE. If salvage Rx chosen & TEE negative, Rx for 4-6 wks with systemic abx and antibiotic lock therapy. b. Gram negative: Primary rec: remove CVC, Rx for 14 days. If salvage Rx chosen, Rx for 14 days with systemic abx and antibiotic lock therapy. c. Candida: Remove CVC, Rx for 14 days. Salvage treatment should not be attempted. d. Coagulase-negative staphylococcus: may retain CVC and treat with systemic antibiotic x 7d + antibiotic lock therapy for 10-14 days. If catheter is removed, treat for 5-7 days (most clinicians would attempt to salvage the line). VI. Common questions to the ID consult service: 1. Does every patient with S. aureus bacteremia need prolonged iv abx? a transesophageal ECHO? should the line be removed? Recommendations for the treatment of S. aureus bacteremia (SAB) continue to evolve. There are no randomized trials evaluating the optimal length of treatment for uncomplicated SAB (normal ECHO, negative surveillance cultures 2-4 d after starting therapy, removable focus of infection, not immunocompromised, rapid clinical resolutions of sxs within 72h of starting abx and removing focus of infection, and no indwelling prosthetic devices or underlying heart disease). For uncomplicated SAB, many would treat for 14 days. In one study of pts with SAB, TTE had a sensitivity of only 32% for IE while TEE (used as a gold standard) had a sensitivity of 100% (Fowler et al., 1997). Even if SAB is nosocomially acquired, there is a high risk of IE (46% of pts with S. aureus IE in one study had nosocomial SAB (Fowler et al., 1999)). TEEs may actually be cost-effective compared to empiric treatment of 2-4 wks (Rosen et al., 1999). Due to the high rates of IE complicating SAB, evidence is accumulating to perform a TEE before deciding to treat as uncomplicated bacteremia for 14 days. Removal of lines is strongly advised. In one study, 56.5% of pts who did not have their line removed had a relapse (compared to a 22.3% failure rate for those who had their line removed (Fowler et al., 1998). For an excellent review of the management of line infections, see Mermel et al (2001) (Mermel et al., 2001). In summary: 1) 2 wks of treatment is probably adequate for uncomplicated SAB, 2) remove all lines if possible, 3) there is some evidence that TEEs should be strongly considered in all patients before deciding to treat as uncomplicated SAB. The standard of care is not settled on the role of TEEs. 2. Which patients with IE can be treated for only 2 weeks? Are there any oral options for treating endocarditis? A. Patients with PCN susceptible viridans streptococci & S. bovis (MIC ≤0.1 g/ml) can be treated with 2 weeks of penicillin and gentamicin (left or right-sided lesions). B. Uncomplicated right-sided endocarditis caused by S. aureus in injection drug users can also be treated with 2 weeks of therapy (DiNubile, 1994; Heldman et al., 1996). Some patients with a h/o IDU leave the hospital against medical advice before completing a full course of therapy which has raised interest in designing effective shorter-course regimens. For uncomplicated, right-sided IE due to MSSA (no metastatic foci of infection), 2 week regimens of nafcillin + aminoglycoside have efficacy rates of greater than 95% and are considered appropriate treatment. For oral regimens, the only data concerns IDUs with right-sided S. aureus. One study (Heldman et al) compared 28 days of iv treatment (oxacillin or vancomycin + gentamicin for the 1 st 5 days) versus 5 days of iv treatment (oxacillin or vancomycin + gentamicin) followed by 23 days of oral ciprofloxacin and rifampin (Heldman et al., 1996). The oral and iv regimens were similarly effective. A previous, uncontrolled study had found a cipro-rifampin oral regimen to be effective in 10 patients (Dworkin et al., 1989). While this oral regimen is rarely used and is not appropriate for standard care, it may provide an alternative for patients who refuse iv therapy. 3. Given the inconvenient dosing of nafcillin (q4h), is it truly better than a 1 st generation cephalosporin (i.e. cefazolin at q8h) for treating S. aureus endocarditis? Is it OK to use ceftriaxone with qd dosing for S. aureus? The standard of care for treating MSSA has evolved to include a penicillinase-resistant penicillin (nafcillin or oxacillin). There have been no prospective randomized trials in humans comparing nafcillin with cefazolin. The data rests on a few case reports of significant failure rates of cefazolin and IE. The data arguing in favor of nafcillin over 1 st generation cephalosporins are: A. In vitro data: Nafcillin has a lower MIC (0.25 g/ml) for S. aureus than cephalosporins (cefazolin 1 g/ml, ceftriaxone 2 g/ml). While this is true, the peak drug level/MIC ratio is extremely high for all of them (nafcillin 320, cefazolin 188, ceftriaxone 112). A level of 10-12 is thought to represent a saturated peak/MIC level for most infections (especially since beta-lactams have time-dependent or concentration-independent killing properties). B. The inoculum effect: Argument: The MIC of nafcillin remains low even at the high concentration of bacteria found in vegetations. In contrast, the MIC is raised for cefazolin and the MBC is so high that there is no bactericidal activity. While some data supports this, other studies contradict it. C. Animal model: Argument: nafcillin sterilizes vegetations more quickly and is thus more effective in animal models of endocarditis. The data does not uniformly support this point either. Overall, the data is inconclusive comparing nafcillin and cefazolin or any other cephalosporin. Due to the standard of care that has evolved, nafcillin continues to be the drug of choice for MSSA IE even though the data do not correspond to the strength of the preference. With continuous infusion pumps, nafcillin has become much easier to give as home therapy and this option will be available for most patients. References: Baddour, L. M., Wilson, W. R., Bayer, A. S., Fowler, V. G., Jr., Bolger, A. F., Levison, M. E., Ferrieri, P., Gerber, M. A., Tani, L. Y., Gewitz, M. H., et al. (2005). Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: endorsed by the Infectious Diseases Society of America. Circulation 111, e394-434. Berbari, E. F., Cockerill, F. R., 3rd, and Steckelberg, J. M. (1997). Infective endocarditis due to unusual or fastidious microorganisms. Mayo Clin Proc 72, 532-542. Bingham, W. (1977). Treatment of intracranial mycotic aneurysms. J Neurosurg 46, 428-437. Blot, F., Nitenberg, G., Chachaty, E., Raynard, B., Germann, N., Antoun, S., Laplanche, A., Brun-Buisson, C., and Tancrede, C. (1999). Diagnosis of catheter-related bacteraemia: a prospective comparison of the time to positivity of hub-blood versus peripheral-blood cultures. Lancet 354, 1071-1077. Blot, F., Schmidt, E., Nitenberg, G., Tancrede, C., Leclercq, B., Laplanche, A., and Andremont, A. (1998). Earlier positivity of centralvenous- versus peripheral-blood cultures is highly predictive of catheter-related sepsis. J Clin Microbiol 36, 105-109. Dajani, A. S., Taubert, K. A., Wilson, W., Bolger, A. F., Bayer, A., Ferrieri, P., Gewitz, M. H., Shulman, S. T., Nouri, S., Newburger, J. W., et al. (1997). Prevention of bacterial endocarditis. Recommendations by the American Heart Association. Jama 277, 1794-1801. DiNubile, M. J. (1994). Short-course antibiotic therapy for right-sided endocarditis caused by Staphylococcus aureus in injection drug users. Ann Intern Med 121, 873-876. Durack, D. T., Lukes, A. S., and Bright, D. K. (1994). New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med 96, 200-209. Dworkin, R. J., Lee, B. L., Sande, M. A., and Chambers, H. F. (1989). Treatment of right-sided Staphylococcus aureus endocarditis in intravenous drug users with ciprofloxacin and rifampicin. Lancet 2, 1071-1073. Eishi, K. (1995). Surgical management of infective endocarditis associated with cerebral complications. J Thorac Cardiovasc Surg 110, 1745-1755. Fowler, V. G., Jr., Li, J., Corey, G. R., Boley, J., Marr, K. A., Gopal, A. K., Kong, L. K., Gottlieb, G., Donovan, C. L., Sexton, D. J., and Ryan, T. (1997). Role of echocardiography in evaluation of patients with Staphylococcus aureus bacteremia: experience in 103 patients. J Am Coll Cardiol 30, 1072-1078. Fowler, V. G., Jr., Sanders, L. L., Kong, L. K., McClelland, R. S., Gottlieb, G. S., Li, J., Ryan, T., Sexton, D. J., Roussakis, G., Harrell, L. J., and Corey, G. R. (1999). Infective endocarditis due to Staphylococcus aureus: 59 prospectively identified cases with follow-up. Clin Infect Dis 28, 106-114. Fowler, V. G., Jr., Sanders, L. L., Sexton, D. J., Kong, L., Marr, K. A., Gopal, A. K., Gottlieb, G., McClelland, R. S., and Corey, G. R. (1998). Outcome of Staphylococcus aureus bacteremia according to compliance with recommendations of infectious diseases specialists: experience with 244 patients. Clin Infect Dis 27, 478-486. Gaur, A. H., Flynn, P. M., Giannini, M. A., Shenep, J. L., and Hayden, R. T. (2003). Difference in time to detection: a simple method to differentiate catheter-related from non-catheter-related bloodstream infection in immunocompromised pediatric patients. Clin Infect Dis 37, 469-475. Epub 2003 Jul 2030. Hasbun, R., Vikram, H. R., Barakat, L. A., Buenconsejo, J., and Quagliarello, V. J. (2003). Complicated left-sided native valve endocarditis in adults: risk classification for mortality. Jama 289, 1933-1940. Heiro, M., Nikoskelainen, J., Hartiala, J. J., Saraste, M. K., and Kotilainen, P. M. (1998). Diagnosis of infective endocarditis. Sensitivity of the Duke vs von Reyn criteria. Arch Intern Med 158, 18-24. Heldman, A. W., Hartert, T. V., Ray, S. C., Daoud, E. G., Kowalski, T. E., Pompili, V. J., Sisson, S. D., Tidmore, W. C., vom Eigen, K. A., Goodman, S. N., et al. (1996). Oral antibiotic treatment of right-sided staphylococcal endocarditis in injection drug users: prospective randomized comparison with parenteral therapy. Am J Med 101, 68-76. Houpikian, P., and Raoult, D. (2005). Blood culture-negative endocarditis in a reference center: etiologic diagnosis of 348 cases. Medicine (Baltimore) 84, 162-173. Li, J. S., Sexton, D. J., Mick, N., Nettles, R., Fowler, V. G., Jr., Ryan, T., Bashore, T., and Corey, G. R. (2000). Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30, 633-638. Mermel, L. A., et al. (2009). Clinical Practice Guidelines for the diagnosis and management of intravascular catheter-related infections: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis 49, 1-45. O'Grady, N. P., Alexander, M., Dellinger, E. P., Gerberding, J. L., Heard, S. O., Maki, D. G., Masur, H., McCormick, R. D., Mermel, L. A., Pearson, M. L., et al. (2002). Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. MMWR Recomm Rep 51, 1-29. Roberts, G. J. (1999). Dentists are innocent! "Everyday" bacteremia is the real culprit: a review and assessment of the evidence that dental surgical procedures are a principal cause of bacterial endocarditis in children. Pediatr Cardiol 20, 317-325. Rosen, A. B., Fowler, V. G., Jr., Corey, G. R., Downs, S. M., Biddle, A. K., Li, J., and Jollis, J. G. (1999). Cost-effectiveness of transesophageal echocardiography to determine the duration of therapy for intravascular catheter-associated Staphylococcus aureus bacteremia. Ann Intern Med 130, 810-820. Siegman-Igra, Y., Anglim, A. M., Shapiro, D. E., Adal, K. A., Strain, B. A., and Farr, B. M. (1997). Diagnosis of vascular catheter-related bloodstream infection: a meta-analysis. J Clin Microbiol 35, 928-936. Steckelberg, J. M., and Wilson, W. R. (1993). Risk factors for infective endocarditis. Infect Dis Clin North Am 7, 9-19. Strom, B. L., Abrutyn, E., Berlin, J. A., Kinman, J. L., Feldman, R. S., Stolley, P. D., Levison, M. E., Korzeniowski, O. M., and Kaye, D. (1998). Dental and cardiac risk factors for infective endocarditis. A population-based, case-control study. Ann Intern Med 129, 761-769. Ting, W. e. a. (1991). Valve replacement in patients with infective endocarditis and cerebral septic emboli. Ann Thorac Surg 51, 18-22. Tunkel, A., Kaye, D (1993). Neurologic complications of infective endocarditis. Neurologic Clinics 11, 419-440. Wilson, W., Taubert, K. A., Gewitz, M., Lockhart, P. B., Baddour, L. M., Levison, M., Bolger, A., Cabell, C. H., Takahashi, M., Baltimore, R. S., et al. (2007). Prevention of Infective Endocarditis. Guidelines From the American Heart Association. A Guideline From the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation.