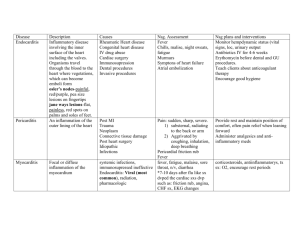
Seminar Infective endocarditis Mingfang Li, Joon Bum Kim, B K S Sastry, Minglong Chen First described more than 350 years ago, infective endocarditis represents a global health concern characterised by infections affecting the native or prosthetic heart valves, the mural endocardium, a septal defect, or an indwelling cardiac device. Over recent decades, shifts in causation and epidemiology have been observed. Echocardiography remains pivotal in the diagnosis of infective endocarditis, with alternative imaging modalities gaining significance. Multidisciplinary management requiring expertise of cardiologists, cardiovascular surgeons, infectious disease specialists, microbiologists, radiologists and neurologists, is imperative. Current recommendations for clinical management often rely on observational studies, given the limited number of well conducted randomised controlled trials studying infective endocarditis due to the rarity of the disease. In this Seminar, we provide a comprehensive overview of optimal clinical practices in infective endocarditis, highlighting key aspects of pathophysiology, pathogens, diagnosis, management, prevention, and multidisciplinary approaches, providing updates on recent research findings and addressing remaining controversies in diagnostic accuracy, prevention strategies, and optimal treatment. Introduction Infective endocarditis is defined as a disease of the endocardial surface of the heart, with infection primarily involving the cardiac valves (native or prosthetic), the mural endocardium, a septal defect, or an indwelling cardiac device. This condition can present with a broad spectrum of symptoms and signs. Infective endocarditis was first described in 1674.1 Infective endocarditis predominantly affects young adults, is subacute in nature with streptococci and enterococci as the most common pathogens, and is often linked to underlying cardiac abnormalities, such as rheumatic heart disease or congenital heart disease.2–4 However, in the late 1980s, the landscape of infective endocarditis transformed considerably mainly due to the increased availability of prosthetic heart valves, intracardiac pacemakers, and catheters. This shift made infective endocarditis more acute, affecting older individuals with a broader range of pathogens. In the era of intravascular devices, these changes in infective endocarditis are intensified by alterations in the gut and oral microbiome and widespread inflammatory response triggered by valvular pathogens. In addition, several other factors might also contribute to the changing landscape of infective endocarditis, including more efficient diagnostic methods, improved treatment rates, and an overall increase in life expectancy. Despite advancements in treatment, infective endocarditis continues to be clinically challenging with an overall mortality rate of 30%.5,6 In this context, we provide a comprehensive overview of optimal clinical practices in infective endocarditis, highlight key aspects of pathophysiology, pathogens, diagnosis, management, prevention, and multidisciplinary approaches, provide updates on recent research findings, and address remaining controversies in diagnostic accuracy, prevention strategies, and optimal treatment. Epidemiology The epidemiology of infective endocarditis has undergone considerable changes in the past few decades. Globally, both the number of cases and associated deaths www.thelancet.com Vol 404 July 27, 2024 have sharply increased over the last 30 years, rising from 478 000 in 1990 to 1 090 530 in 2019, and from 28 750 in 1990 to 66 320 in 2019.7 The annual incidence between 1970 and 2000 was about 3·0–10·0 cases per 100 000 person-years and did not have a statistically significant change.8,9 The incidence gradually increased to 13·8 per 100 000 population in 2019. Notably, men exhibit a higher incidence of infective endocarditis compared with women, with men-towomen ratios ranging from 3:2 to 9:1 in various studies.10 However, mortality-to-incidence ratios are higher in women than men, suggesting worse outcomes in female patients.11 The reason behind the sex difference remains unknown and warrants further investigation. Age is another crucial factor in infective endocarditis epidemiology. The incidence rate was higher in older people and increased over time.12,13 In 2019, patients aged 50 years and older accounted for nearly 63% of incidence and 79% of mortality, a statistically significant increase compared to 1990.7 Among the younger population, congenital heart Lancet 2024; 404: 377–92 Division of Cardiology, the First Affiliated Hospital of Nanjing Medical University, Nanjing, Jiangsu, China (M Li MD, Prof M Chen MD); Department of Thoracic and Cardiovascular Surgery, Aortic Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, South Korea (J B Kim MD); Department of Cardiology, Renova Century Hospital, Hyderabad, Telangana, India (B K S Sastry MD) Correspondence to: Prof Minglong Chen, Division of Cardiology, the First Affiliated Hospital of Nanjing Medical University, Nanjing, Jiangsu 210029, China chenminglong@njmu.edu.cn Search strategy and selection criteria We performed a literature search of the PubMed database using the search terms: “infective endocarditis”, “epidemiology”, “pathogenesis”, “manifestations”, “imaging”, “diagnosis”, “treatment”, “surgery”, and “management”. We primarily selected publications from the past decade. Studies published before 2016, the year in which the previous Seminar on infective endocarditis was published in The Lancet, were considered for inclusion if they were widely cited in the literature or in the current guidelines. Additionally, we extended our search by reviewing the reference lists cited in articles identified by this strategy and guideline statements in the diagnosis and management of infective endocarditis published by the European Society of Cardiology and the American Heart Association. Articles deemed relevant were also included. Only articles published in English were included. 377 Seminar 1) Normal endothelium Resistent to pathogen 2) Bacterial adhesion 3) Inflammatory response Risk factors • Prosthetic valve • Cardiac implantable electronic devices • Congenital heart disease • Intravenous drug use Bacteria Monocytes Platelets 4) Vegetation formation Thrombogenesis Cytokines Infective endocarditis Endothelium Figure 1: The pathophysiology of infective endocarditis Infective endocarditis begins with bacterial adhesion to tissues within the circulatory system, particularly the vascular endothelium, endocardium, and valvular apparatus. Once bacteria adhere, an inflammatory response is initiated with the involvement of inflammatory cells and is mediated by the production of multiple cytokines associated with integrins, tissue factors, and adhesion molecules. These cytokines in turn attract monocytes and platelets with the associated production of fibronectin, which leads to thrombus formation. The aggregated thrombi provide a favourable environment for bacteria to survive, constituting a vicious cycle that further activates the inflammatory cascade in an orchestrated manner against the host’s defences, eventually forming an infected vegetation. Figure created with BioRender.com. A B NCC RCC AL Pathophysiology AS PL LCC RA IVC Figure 2: Vegetations in infective endocarditis (A) Vegetations (green arrow) associated with native mitral valve. (B) Vegetations (green arrow) associated with native aortic valve. AL=anterior leaflet of the mitral valve. AS=atrial septum. IVC=inferior vena cava. LCC=left coronary sinus of the aortic valve. NCC=non-coronary sinus of the aortic valve. PL=posterior leaflet of the mitral valve. RA=right atrium. RCC=right coronary sinus of the aortic valve. disease remains the primary risk factor for infective endocarditis, while intravenous drug use has become a concerning issue. Among people aged 15–34 years, there was a marked four-fold increase in the number of hospital admissions for intravenous drug use-associated infective endocarditis from 2005 to 2016, and a nearly doubled proportion of admissions from 6·9% to 12·1%.14 Socioeconomic disparities also contribute to variations in infective endocarditis incidence. Patients from lowincome and middle-income countries exhibited more frequent complications, such as congestive heart failure and persistent fever, and had a higher mortality rate (23·7% vs 15·0%) compared with those from highincome countries, which could be attributed to delayed diagnosis and lower use of surgery.15 Rheumatic heart 378 disease, with a prevalence of 52·0% (95% CI 42·4–61·5), remains the major underlying cause of infective endocarditis in low-income countries, accounting for almost half of the cases.16,17 However, in high-income countries, due to improvements in medical care and living conditions, degenerative valve disease and congenital heart disease have gradually replaced rheumatic heart disease as the main cause of infective endocarditis.11,18,19 Bacterial adhesion to tissues within the circulatory system constitutes the initiating pathophysiological process of infective endocarditis. However, lining tissues in the circulatory system, such as the vascular endothelium, endocardium, and valvular apparatus, are not subject to such a process under normal physiological status (figure 1).20 Aggravating conditions include previous infective endocarditis, the presence of prosthetic heart valves, residual intra-cardiac shunts, cyanotic congenital heart defects, and ventricular assist devices. Of note, intravenous drug use, which is an increasing global occurrence, is associated with a markedly increased risk of infective endocarditis by repetitive introduction of contaminated particles into the circulatory system with a high recurrence rate.21 Once the initial nidus is established, an inflammatory response is initiated with the involvement of inflammatory cells and mediated by the production of multiple cytokines associated with integrins, tissue factors, and adhesion molecules.22–24 These cytokines in turn attract monocytes and platelets with the associated production of fibronectin, which leads to thrombus formation.23,24 The aggregated thrombi provide a favourable environment for bacteria to reside, constituting a vicious cycle that further activates the inflammatory cascade in an orchestrated manner against the host’s defences, eventually forming infected vegetation (figure 2). Biofilm formation plays a crucial role in the pathogenesis of infective endocarditis, particularly in www.thelancet.com Vol 404 July 27, 2024 Seminar cases involving prosthetic material. A biofilm can insulate the organisms from antibiotics in the blood­ stream and make microbiological cure impossible without surgical intervention to interrupt the biofilm and access the sequestered organisms.25 Pathogens Staphylococcus, streptococcus, and enterococcus are the top three most prevalent microorganisms, accounting for about 80% of infective endocarditis cases.12,13,15,26–28 The majority of cocci were Staphylococcus aureus, followed by viridans group streptococci. Gram-negative bacilli are also potential microorganisms, but these cases are rare. Fungus-associated infective endocarditis, mostly caused by Candida, can present in those who are under immunosuppression, accounting for 1–2% of cases.28 Furthermore, there are also some infective endocarditis cases involving multiple microorganisms.13,26 The proportion of infective endocarditis cases caused by resistant organisms has increased in recent years, which poses challenges for the treatment of this disease.29 Positive blood cultures varied in different studies ranging from 45·4 to 79·0%.12,13,15,26–28 Compared with individuals without positive blood cultures, patients with S aureus or enterococcus infections were at the highest risk of 1-year mortality.12 Diagnosis The diagnostic standard for infective endocarditis is pathological confirmation, but this is rarely available during the initial therapeutic decision. In most cases, diagnosis relies on clinical findings, microbiological data, and imaging results. Clinical features In general, one should consider the possibility of infective endocarditis in any patient with sepsis of unknown origin or fever accompanied by risk factors. Initial clinical assessment of patients with suspicious symptoms involves evaluating risk factors and exploring supportive medical history and examination findings. Core cardiac risk factors include previous infective endocarditis, prosthetic heart valves, valvular heart disease, transvenous cardiac implantable electronic devices (CIEDs) or ventricular assist devices, congenital heart disease, and hypertrophic cardiomyopathy. Of note, in low-income countries (especially in Africa), rheumatic heart disease remains the most prevalent risk factor for infective endocarditis in adults.16 Non-cardiac risk factors include older age, male sex, central venous or arterial catheter, intravenous drug use, immunosuppression, recent dental or surgical procedures, poor dental hygiene, recent hospitalisation, and haemodialysis. Furthermore, physical examinations can reveal various clinical signs, such as fever, heart murmurs, petechiae, Osler nodes, Janeway lesions, and splenomegaly. However, the diagnosis of infective endocarditis should not be excluded www.thelancet.com Vol 404 July 27, 2024 based on clinical examination alone due to the overall low sensitivity and specificity of clinical signs. According to the European Society of CardiologyEURObservational Research Programme (ESC-EORP) EURO-ENDO (European infective endocarditis) registry, the most predominant clinical symptoms in 3116 patients were fever in 2421 (77·7%) cases and congestive heart failure in 848 (27·2%) cases. Cardiac murmurs, identified as the most frequent sign, were reported in 2010 (64·5%) of these cases. Other symptoms and signs were less common: septic shock in 209 (6·7%) cases, cardiogenic shock in 72 (2·3%), syncope in 81 (2·7%), Janeway lesions in 109 (3·5%), Osler’s nodes in 59 (1·9%), and Roth’s spots in 44 (1·4%) cases.30 Symptomatic embolic complications were present on hospital admission in 788 (25·3%) of 3116 cases, including cerebral in 352 (11·3%) cases, splenic in 177 (5·7%), pulmonary in 199 (6·4%), renal in 78 (2·5%), hepatic in 16 (0·5%), and in 93 (3·0%) cases for other peripheral embolic events. Conduction abnormalities were detected on admission in 358 (11·5%) of 3116 total cases and included first-degree atrioventricular block in 252 (8·1%) and third-degree atrioventricular block in 87 (2·8%) of total cases. Another frequent complication was paravalvular abscess seen in 367 (11·8%) of total cases.30 Infective endocarditis is associated with a wide range of complications (figure 3). Routine laboratory investigation often yields non-specific results, reflecting the complex Cerebrum • Ischaemic stroke • Abscess • Intracranial haemorrhage • Intracerebral abscess • Meningitis • Infective intracranial aneurysms Eye • Roth spots Heart • Congestive heart failure • Valvular dysfunctions • Arrhythmias • Myocardial abscesses • Myocardial infarction Kidney • Acute kidney injury • Glomerulonephritis • Infarction Musculoskeletal complications • Myalgias • Arthralgias • Osteomyelitis Skin • Janway lesions • Osler nodes Embolic complications • Spleen • Lung • Kidney • Liver • Splinter haemorrhages Other symptoms • Fever • Hepatosplenomegaly • Metastatic infection Figure 3: The complications of infective endocarditis Infective endocarditis is associated with a wide range of complications, including cardiac complications (eg, heart failure, valve perforation, valvular incompetence, periannular and myocardial abscesses, arrhythmias, or myocardial infarction), neurologic complications (eg, ischaemic stroke, intracranial haemorrhage, intracerebral abscess, meningitis, or infective intracranial aneurysms), systemic embolisation (involving the spleen, the kidney, the liver, peripheral arteries, or the iliac or mesenteric arteries), renal complications (eg, acute kidney injury due to immune-mediated glomerulonephritis or focal infarction secondary to emboli), musculoskeletal complications (eg, myalgias, arthralgias, or osteomyelitis), pulmonary complications (right-sided vegetation leading to pulmonary embolism, disseminated pulmonary abscesses, pneumonia, or empyema), metastatic infection (including septic embolisation, metastatic abscesses, and mycotic aneurysm), and complications related to medical or surgical therapy. Figure was created with BioRender.com. 379 Seminar pathophysiology involved in infective endocarditis.31 Biomarkers might have a role in initial risk assessment and monitoring the response to antibiotic therapy. Future studies are warranted to assess potential diagnostic biomarkers, including N-terminal-pro-B-type natriuretic peptide, cystatin C, lipopolysaccharide-binding protein, troponins, aquaporin-9, S100 calcium-binding protein A11, E-selectin, VCAM-1, and interleukin-6.32,33 Microbiology Positive blood cultures remain the cornerstone of diagnosis in infective endocarditis. Before administering antibiotics, a standardised blood culture process that involves obtaining at least three separate sets of blood cultures at 30-min intervals is imperative.34,35 Blood cultures can be collected at any time, irrespective of the peaks of fever.36 Gram staining serves as the initial step for presumed identification after positive blood cultures, enabling clinicians to promptly initiate empirical antibiotic treatment. Moreover, despite the considerable advancements in rapid susceptibility testing, the minimal inhibitory concentrations based on susceptibility testing remain the gold standard for selecting appropriate antibiotics.37 Blood culture-negative infectious endocarditis refers to cases of infectious endocarditis where the pathogenic microorganisms cannot be cultivated using the usual blood culture methods and accounts for approximately 2·5–31·0% of all infectious endocarditis presentations.38,39 The primary cause of blood culture-negative infectious endocarditis is the administration of antibiotics before obtaining cultures, resulting in false-negative results. Blood culture-negative infectious endocarditis can also result from fungi or fastidious bacteria, especially A B C LA MV AV AL D AL AR RV E RV RA MV AV LV PL LV LA LV RV PL LA Aorta RCC AV LA LA LA Figure 4: Imaging results of infective endocarditis (A) Three-dimensional transoesophageal echocardiogram (TOE) with MV vegetation (white arrow). (B) TOE with MV vegetation (white arrow) and AV vegetation (white arrow) and colour doppler flow imaging with AV regurgitation. (C) Four-chamber view of transthoracic echocardiography (TTE) with MV vegetation (white arrow). (D) TTE with AV annular abscess (white arrows). (E) Cardiac computed tomography with MV vegetation (white arrow) and AV vegetation (green arrow) in one single patient (left: aortic sinus view, and right: three-chamber view). AL=anterior leaflet of the MV. AR=AV regurgitation. AV=aortic valve. LA=left atrium. LV=left ventricle. MV=mitral valve. PL=posterior leaflet of the MV. RA=right atrium. RCC=right coronary sinus of the AV. RV=right ventricle. 380 obligate intracellular bacteria (eg, Coxiella burnetiid, Bartonella spp, and Brucella spp) that require specialised culture media for isolation.40 The HACEK group of organisms (Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella corrodens, and Kingella) are known as blood culture-negative organisms that predominantly affect individuals with heart disease or artificial valves.41 In cases of C burnetiid and Bartonella spp, systematic serological testing or PCR assays might be required to facilitate the identification of causative bacteria.40,42 Culturing HACEK organisms used to be difficult; however, when using current automated blood culture systems, an incubation period of 5 days is adequate for detecting the HACEK group.43,44 Some other advanced technologies, such as molecular analysis (16S ribosomal RNA for bacteria and 18S ribosomal RNA for fungi) and meta-genomic nextgeneration sequencing are becoming increasingly crucial in diagnosing and managing blood culture-negative infectious endocarditis.45,46 Imaging Echocardiography is the primary diagnostic tool, with additional modalities aiding when confirming the diagnosis, assessing complications, and identifying the source of bacteraemia. Transthoracic echocardiography is commonly the initial imaging modality for suspected infective endocarditis, with a high specificity (>90%) and modest sensitivity (75%) in detecting vegetation.47 Transoesophageal echocardiography provides higher sensitivity than transthoracic echocardiography for diagnosing infective endocarditis;48 therefore, when there is a strong suspicion of infective endocarditis, but the transthoracic echocardiography results are negative or the image quality is suboptimal, transoesophageal echo­ cardiog­raphy should be performed.36 In cases of suspected prosthetic or intravascular device-related infective endocarditis, transoesophageal echocardio­graphy should be performed irrespective of high-quality transthoracic echocardiography imaging.48 Moreover, transoesophageal echocardiography could also be needed to screen for specific complications (eg, perivalvular abscess) in patients with known severe pathogens such as staphylococcus.49 Additionally, a repeat echocardio­ graphy should be considered 5–7 days later to identify complications or if clinical suspicion of infective endocarditis is high.50,51 Although not commonly used, three-dimensional transoesophageal echocardiography can provide additional information on vegetation size and morphology beyond conventional transoesophageal echocardiography, leading to a more accurate prediction of the embolism risk associated with infectious endocarditis (figure 4A–D).52,53 When echocardiography is contraindicated or incon­ clusive in patients with suspected infective endocarditis, cardiac computed tomography CT might be considered as an alternative (figure 4E). Although inferior to transoesophageal echocardiography in detecting vegetations, cardiac CT surpasses transoesophageal www.thelancet.com Vol 404 July 27, 2024 Seminar echocardiography in assessing paravalvular and periprosthetic complications.54–56 The [¹⁸F]fluorodeoxy­ glucose ([¹⁸F]FDG)-PET-CT show an 86% sensitivity and 84% specificity for suspected prosthetic valve endocarditis and can aid in differentiating alternative diagnoses.57–59 In comparison to CT, MRI has a higher sensitivity for detecting cerebral lesions, making it a valuable tool for both diagnosing and monitoring associated neurological complications, such as ischaemic lesions and cerebral microbleeds.60,61 CT angiography can also detect complications such as mycotic arterial aneurysms, including those affecting the CNS.62 Thrombolytic therapy is not recommended in patients with infective endocarditis and stroke, but thrombectomy can be considered in specific cases of large vessel occlusion.63,64 Neurosurgical treatment or endovascular therapy should be considered in cases of large intracranial infective cerebral aneurysms, ruptured aneurysms, or unruptured aneurysms that do not respond to optimal antibiotic therapy.65 Moreover, whole-body and brain CT are valuable for assessing systemic complications, assisting in the identification of distant lesions and sources of bacteraemia. In some instances, integrating multiple imaging modalities is needed to improve accuracy of diagnosing infective endocarditis. The 2023 Duke–International Society for Cardiovascular Infectious Diseases criteria for infective endocarditis The Duke criteria for infective endocarditis were initially proposed in 1994 and refined in 2000 as the modified Duke criteria.66,67 In response to the evolving understanding of infective endocarditis, the 2023 Duke–ISCVID (the International Society for Cardiovascular Infectious Diseases) criteria were proposed as the most recent update to the modified Duke criteria.68 The Duke–ISCVID criteria mainly proposed the number of new additions (appendix pp 3–6). First, new microbiology diagnostics (enzyme immunoassay for Bartonella species, PCR, amplicon and metagenomic sequencing, and in situ hybridisation) and imaging ([¹⁸F]FDG-PET-CT, and cardiac CT) were introduced. Second, intraoperative inspection was included as a new major clinical criterion. Third, the list of typical microorganisms causing infective endocarditis was expanded, considering some pathogens typical only in the presence of intracardiac prostheses. Fourth, specific requirements for timing and separate venepunctures for blood cultures were eliminated. Last, additional predisposing conditions including transcatheter valve implants, CIED, and previous infective endocarditis criteria were clarified.68 An external validation study showed that the 2023 Duke–ISCVID criteria were more sensitive than the modified Duke criteria (84·2% vs 74·9%, p<0·001) without significant loss of specificity.69 However, these criteria should be used with caution as they serve as a diagnostic guide rather than a substitute for clinical judgement.70 www.thelancet.com Vol 404 July 27, 2024 Initial empirical therapy Endocarditis Treatment Duration ·· Ampicillin, cloxacillin, ceftriaxone, or vancomycin* plus gentamycin Until the pathogen is identified Based on results of blood culture Bacteria Streptococci NVE Ceftriaxone plus gentamycin 4 weeks Streptococci PVE Ceftriaxone + gentamycin 6 weeks Staphylococci NVE Flucloxacillin or cefazolin or vancomycin based on sensitivity† 4–6 weeks Staphylococci PVE Flucloxacillin, vancomycin‡, or cefazolin plus gentamycin and rifampicin 6 weeks Enterococci NVE Ampicillin plus gentamycin, vancomycin plus gentamycin, or ampicillin plus ceftriaxone 6 weeks Enterococci PVE Ampicillin plus gentamycin, vancomycin plus gentamycin, or ampicillin plus ceftriaxone 6 weeks NVE or PVE Should be based on epidemiological factors and in consultation with infectious disease expert Variable Culture negative NVE=native valve endocarditis. PVE=prosthetic valve endocarditis. *Vancomycin for patients who are sensitive to penicillin. †In penicillin-sensitive patients with methicillin-sensitive organisms, use cefazolin or vancomycin. ‡Daptomycin and linezolid can be used when vancomycin is ineffective or cannot be used. Table 1: Antibiotic choice and duration of therapy in the treatment of infective endocarditis Management Antibiotics: principles and methods If patients have an acute presentation, intravenous antibiotic therapy should be started immediately after obtaining blood samples for culture. The choice of antibiotics depends on factors, such as underlying cardiac disease, presence of infected foreign body implants, epidemiological factors, the local community’s pattern of microbial sensitivity, and the patient’s immunological status. Infectious diseases experts should be involved from the beginning. For insidious clinical presentation, one can wait for blood culture results before initiating antibiotics and if needed, repeat blood cultures. There are few randomised controlled trials (RCTs) available to inform therapy decisions for antibiotics, and recommendations rely primarily on guidelines.36 Many recommendations stem from expert consensus, small studies, retrospective studies, or registries.71 The details of the antibiotic choice and the duration of treatment are listed in table 1 (appendix p 7). The choice of antibiotics, dose, and duration are dependent upon the minimal inhibitory concentrations in blood culture. Treatment decisions are based on clinical features and serological tests. Treatment of infective endocarditis can be divided into two phases (appendix p 8).36 During the early critical phase, surgical or other appropriate interventions are made while the patient is receiving intravenous antibiotics. This phase lasts until the patient becomes afebrile with sterile blood cultures. After a week or 10 days of effective antibiotic therapy, patients enter the continuation phase. Patients with complex infections should continue treatment in hospital to receive a complete course of parenteral antibiotics. The POET (Partial Oral Treatment of See Online for appendix 381 Seminar Endocarditis) trial has shown that oral antibiotic therapy can be considered during the continuation phase in stable patients who no longer require any surgery or have embolic phenomena.72 If good compliance can be assured, patients can be discharged home with full 4–6 weeks of intravenous antibiotic therapy or selected oral drugs that reach effective bactericidal blood levels. Close postdischarge monitoring and completion of the full course of treatment is mandatory. Surgery: principles and methods Surgical indication and timing for patients with infective endocarditis are mainly based on the 2023 ESC guidelines.36 The data supporting most of the other recommendations are derived from large non-randomised studies, expert consensus, or small-scale studies. Surgical indications for infective endocarditis can be best summarised by the triad, which refers to: (1) heart failure, (2) uncontrolled infection, and (3) embolic prevention (appendix p 9).36 Manifestations of heart failure as the surgical trigger include refractory pulmonary oedema, cardiogenic shock, dyspnoeic symptoms, or echocardio­ graphic signs of poor haemodynamic tolerance caused by severe dysfunctions of affected heart valves. Representative clinical scenarios of uncontrolled infection can be categorised into local structural complications and more general situations that correspond to medical treatment failure. Local structural failures include abscesses, pseudo­ aneurysms, fistula, prosthetic dehiscence, and the development of a new atrioventricular conduction block. General situations refer to infective endocarditis caused by fungi or organisms resistant to multi-antimicrobial drugs and persistent or progressive diseases despite adequate antibiotic therapy for sufficient periods. For embolic prevention, vegetation with a size of 10 mm or more has been suggested as the definite surgical trigger (class I recommendation) in the presence of embolic episodes; however, those without clinical evidence of embolism have been given a lower level of surgical recommendation (class IIB).36 These traditional surgical indications have recently been challenged by a study from South Korea, the only RCT on intervention in infective endocarditis.73 While the presence of severe dysfunction or large vegetation (≥10 mm) without relevant symptoms has not been considered for urgent surgery in the traditional approach, the trial enrolled asymptomatic patients with infective endocarditis presenting with severe dysfunction of affected valves accompanied by large vegetations.73 Although the rates of death did not differ between the early surgery group and the conventional medical treatment group, the difference stemmed from the fact that the rate of embolic events was significantly in favour of early surgery (0% vs 21%, p=0·005). The findings advocate early surgery for infective endocarditis in the presence of severe valvular dysfunction and large vegetation even in asymptomatic individuals. 382 Risks imbedded in surgical therapy are also an important consideration for decision making.74 For instance, a non-negligible proportion of patients who have clear surgical indications might not be offered operations based on perceived unacceptable surgical risks, with a resultant worse prognosis.75,76 To aid the decision making in this complex scenario of infective endocarditis, several surgical risk scoring systems have been developed.77–81 However, since these scoring systems are based on retrospective data, their performances are variable and none of these are generalised in daily clinical practices, which calls for the development of scoring systems from prospective data entailing greater predictive capacity. In adult patients, homografts can serve as an alternative to mechanical or bioprosthetic valves in acute aortic valve endocarditis due to their lower susceptibility to infections and high degree of resistance to recurrent infection.82 However, the use of homografts also poses specific considerations, such as availability, durability, and the risk of homograft degeneration over time. Therefore, further investigation into the indications, surgical techniques, outcomes, and potential complications associated with the use of homograft aortic valves in prosthetic or complex aortic infection is warranted. Among people with intravenous drug use-associated infective endocarditis, early survival rates were favourable, while the long-term prognosis was compromised.14,83 Compared with non-drug users, they had longer hospital stays and higher rates of readmission, largely due to approximately a third of patients resuming drug injection upon re-admission. In this specific population, surgical intervention does not offer a long-term survival advantage.83–85 Consequently, both addiction treatment (ie, detoxification, medicationassisted treatment, behavioural therapy, psychosocial support, and relapse prevention) and infection prevention play crucial roles in managing this population. The management of major complications Major complications of infective endocarditis often involve valvular dysfunction, heart failure, embolisation, and infectious complications. Management of these major complications requires a multidisciplinary approach involving cardiologists, infectious disease specialists, cardiac surgeons, radiologists, neurologists, and other health-care professionals. In addition, early recognition, timely medical or surgical intervention, and close monitoring are essential in mitigating the effects of complications and improving the overall prognosis of individuals affected by infective endocarditis. Adjunctive medical therapy RCTs that specifically addressed antithrombotic or anticoagulant therapy in infective endocarditis-related stroke prevention or treatment were scarce. Infective endocarditis alone does not necessitate the use of these medications, but bleeding complications or strokes www.thelancet.com Vol 404 July 27, 2024 Seminar might justify their interruption or discontinuation. It is generally accepted to bridge with low molecular weight heparin or unfractionated heparin rather than oral anticoagulants in the initial stage of infective endocarditis, particularly for patients requiring surgery. Antiplatelet agents showed mixed results in infective endocarditis.86 Current guidelines advise against the routine initiation of antiplatelet agents, while maintaining long-term use in those with low bleeding risk is considered reasonable. Discussion within the endocarditis team is warranted when facing the challenge of antithrombotic or anticoagulant therapy. Long-term prognosis and ongoing care Long-term survival rates for patients with infective endocarditis approximate to 85–90% at year 1 and 70–80% at 5 years.87–91 The main risk factors for poor prognosis include recurrence of infective endocarditis, heart failure, older age, comorbidities, and double valve infection.87,90–92 Studies reported various recurrence rates, with a range between 2% and 9%.87,88,90,91,93–96 Post-discharge monitoring for relapses and reinfections of infective endocarditis is of great importance, and it is crucial to differentiate between the two since reinfections are associated with worse outcomes compared with relapses.97 Conceptually, relapse refers to a repeat episode of the infection by the same microorganism, which usually indicates ineffective antibiotic treatment.90 Reinfection, caused by another microorganism, usually occurs 6 months after the initial episode.97 Treatment for relapse should include intravenous antibiotics for an additional 4–6 weeks, and cardiac surgery should be considered for a persistent focus of infection.87,91–93,96 During the discharge follow-up, it is essential to educate patients on recurrence risks and prevention strategies. Education should include at least one clinical reassessment in the first year and annually thereafter. Patients should be vigilant for new onset symptoms of fever, chills, or other signs indicating recurrence and should also be monitored for secondary heart failure, although the need for late valve surgery is quite low.92 Additionally, recommendations for maintaining good oral health and skin hygiene, including avoiding tattoos and piercings, should be provided to minimise the risk for infection.98 Prevention The development of infective endocarditis requires the aforementioned risk factors, bloodstream entry of pathogens, and a competent host immune response. The role of predisposing risk factors is highlighted by Thornhill and colleagues who reported that annually 280 cases per 100 000 patients at moderate risk and 497 per 100 000 patients at high risk had an incident of infective endocarditis based on their predisposing risk factors, respectively.99 Entry portals for bacteria and fungi vary, including skin, oral cavity, gastrointestinal, or www.thelancet.com Vol 404 July 27, 2024 genitourinary infections; direct inoculation in drug users; unsafe vascular punctures; and health-care exposure.64,100–104 Prevention strategies for infective endocarditis should address the underlying risk factors prevalent in all regions of the world. Particularly, implementing primary and secondary prevention measures for acute rheumatic fever and rheumatic heart disease is crucial to alleviate the burden of infective endocarditis in Africa, given that rheumatic heart disease is the most important risk factor for infective endocarditis across the continent. Primary prevention measures for acute rheumatic fever and rheumatic heart disease include promoting awareness, administering antibiotic prophylaxis, and improving access to health care. Secondary prevention involves longterm antibiotic treatment, regular medical follow-ups, and health promotion to reduce complications. Historically, antibiotic prophylaxis was widely advocated before various medical and dental procedures for individuals at increased risk of infective endocarditis, encompassing both moderate-risk and high-risk categories. However, in the mid-2000s, the American Heart Association and ESC restricted antibiotic prophylaxis use solely to individuals at high risk undergoing invasive dental procedures, such as manipulation of the gingival tissue or periapical region around the teeth and perforation of the oral mucosa due to concerns regarding the lack of evidence for the efficacy of antibiotic prophylaxis, the risk of adverse drug reactions to antibiotic prophylaxis antibiotics, and the potential for antibiotic resistance.105,106 However, in the last decade there has been much new evidence on the association between invasive dental procedures and subsequent infective endocarditis, and the efficacy, safety, and cost-effectiveness of antibiotic prophylaxis in preventing infective endocarditis.107 Most importantly, two large US studies using both casecrossover and cohort methodologies—one in patients with employer-provided medical and dental insurance coverage and the other in Medicaid patients—have both shown the efficacy of antibiotic prophylaxis in reducing the risk of infective endocarditis following invasive dental procedures for patients at high risk, thereby supporting the guideline recommendations.108,109 Notably, despite the availability of only one of these two studies at the time, the 2023 ESC guidelines upgraded the classification of the recommendation for antibiotic prophylaxis before invasive dental procedures in patients at high risk from class IIa (weight of evidence, opinion in favour of usefulness, and efficacy) to class I (evidence or agreement on the treatment or procedure being beneficial, useful, and effective).36 Furthermore, the level of evidence supporting this recommendation was elevated from level C (consensus opinion of experts, small studies, retrospective studies, or registries) to level B (data derived from a single randomised clinical trial or large non-randomised studies) for individuals with a previous history of infective endocarditis. Moreover, recent studies have elucidated the 383 Seminar minimal risk of adverse drug reactions associated with amoxicillin antibiotic prophylaxis and underscored the cost-effectiveness of antibiotic prophylaxis in preventing infective endocarditis.110,111 However, it is essential to recognise that not all viridans group streptococci-infective endocarditis cases stem from invasive dental procedures. Many could arise from daily activities, such as tooth brushing, flossing, and chewing food, particularly in individuals with poor oral hygiene. A recent case–control study has revealed that even individuals at moderate risk with poor oral hygiene are at significantly increased risk of developing infective endocarditis compared with those with better oral hygiene.104 This highlights the importance of promoting and maintaining optimal oral hygiene in preventing infective endocarditis in populations at moderate risk and high risk. Furthermore, emerging evidence challenges the notion that antibiotic prophylaxis was abandoned for some invasive medical and surgical procedures by the guidelines in the mid-2000s.105,106 Recent studies have suggested that the abandonment of antibiotic prophylaxis for procedures, such as permanent pacemaker and defibrillator implan­ tation, upper and lower gastrointestinal endoscopy, and bronchoscopy might have been premature.102,103 Reconsidering antibiotic prophylaxis coverage for some invasive procedures is recommended by the most recent ESC guidelines and the American Heart Association’s recent scientific advisory.36,112 Rational antibiotic selection should target viridans group streptococci, particularly penicillin and cephalosporins, due to their lower rates of Clostridioides difficile infection compared with clindamycin.113 Amoxicillin, despite lacking RCTs, seems to be the most widely used with the lowest overall adverse drug reactions.114,115 If used, oral administration and a single dose are preferred (single 2 g in most countries and 3 g in the UK). In addition, patients at high risk should follow general prevention measures, including maintaining good cutaneous hygiene, avoiding self-medication with antibiotics, applying strict infection control for any at-risk procedure, and reducing catheter-associated bacteraemia by optimising central venous catheter care. Patients with a fever of unknown origin should promptly report it to their physicians for early infective endocarditis screening. Special entities Prosthetic valve infective endocarditis With the increasing number of patients receiving prosthetic heart valve implantation (who serve as the denominator population for potential infectious complications thereafter), prosthetic valve endocarditis, which is one of the most challenging clinical scenarios of infective endocarditis, has been an important clinical issue in the current era.116 Large-scale observational studies have shown a rapid increase in the incidence of prosthetic valve endocarditis and a stable increase in overall infective endocarditis. The incidence rate of 384 prosthetic valve endocarditis is reportedly 0·3–1·2 per 100 person-years, accounting for 20–30% of all infective endocarditis that has been even higher in most recent years.6,27,30,117,118 In one of the largest observational studies with 39 199 patients undergoing aortic valve replacement, prosthetic valve endocarditis is more common with biological than with mechanical prostheses, but the absolute difference is as small as 2·2% versus 1·5% over 12 years, making it hard to detect in smaller studies or perceivable in daily practices.119 Prosthetic valve endocarditis can be categorised into two forms, occurring within 1 year (early form) or after (late form) following prosthetic valve replace­ment surgery. Statistically significant differences have been noted between early and late prosthetic valve endocarditis in terms of microbiological pro­ files.120 Early prosthetic valve endocarditis is closely associated with perioperative infections with common pathogens including S aureus, coagulase-negative staphylococci, Gram-negative pathogens, and fungi.121 Mycobacterium chimaera residing in the heat-exchange system of the cardiopulmonary bypass machine has also been identified as an important pathogen for early prosthetic valve endocarditis, presenting diagnostic challenges due to its indolent presentation but high mortality risk.122 Meanwhile, late prosthetic valve endocarditis usually follows the pattern of infective endocarditis in native valves, with viridans group streptococci being the most frequent pathogens.121 Cardiac implantable electronic devices With the rising number of CIEDs, the incidence of CIED infection is increasing. A National Inpatient Sample Database study showed that the incidence escalated from 1·45% in 2000 to 3·41% in 2012.123 The infection could involve different parts of the device, including the generator, device leads, and the native cardiac structure alone or in combination. The mortality is higher for patients with CIED endocarditis than for those with generator pocket infection.124 Major risk factors for CIEDrelated infective endocarditis include haematoma formation and revisions with the reopening of the pocket.125,126 Clinical signs of leads or endocardium infection include fever, chills, and embolic events with or without the signs of generator pocket infection (pain, swelling, tenderness, purulent discharge, etc). Transthoracic echocardiography and transoesophageal echocardio­ graphy are both recommended in patients with suspected CIED-related infective endocarditis.127–129 However, repeated transthoracic echocardio­ graphy or transoesophageal echocardiography might be necessary, as the initial absence of vegetation does not rule out infective endocarditis. [¹⁸F]FDG-PET-CT has emerged as a great tool for assessing CIED-related infective endocarditis.57,130 The management of a definite CIED infection involves early and complete system extraction www.thelancet.com Vol 404 July 27, 2024 Seminar and empirical antibiotic therapy targeting methicillinresistant S aureus and Gram-negative bacteria.130 System extraction should be performed in centres with expertise and without delay.131,132 During the decision-making process, factors such as pacemaker dependency, patient frailty, lead dwell time, and procedural risks including the possibility of lifethreatening tamponade, should be carefully considered. Percutaneous extraction is preferred except when the vegetation is larger than 20 mm or when valve surgery is indicated.133 Congenital heart disease The incidence rate of infective endocarditis in children with congenital heart disease is low, with an estimated rate of 0·041 per 100 person-years,134 but as the surgical outcomes of children with congenital heart disease have improved, more adults now live with congenital heart disease than children in recent years. As a result, the incidence rate of infective endocarditis in adults with congenital heart disease is reported as around 0·13 per 100 person-years—higher than in children with con­ genital heart disease—and is around 30-fold higher than in the general population.135 Congenital heart disease at increased risk of infective endocarditis includes untreated cyanotic congenital heart disease and status postprosthetic material placed in the circulatory system, such as valved conduits or systemic to pulmonary shunts.99,135,136 The risk of infective endocarditis in the cyanotic functional single ventricle group is known to be particularly high, with a relative risk of six compared with biventricular diseases.30 Transcatheter device-closure of atrial or ventricular septal defects is also known to be associated with a risk of infective endocarditis, but only within 6 months after intervention.135 Left ventricular assist device-related infection With the increasing number of patients on left ventricular assist devices (LVADs) worldwide over the past two decades, LVAD-associated infections have been on the rise and are one of the leading causes of mortality in patients with LVADs. Two major modes of infection are defined as LVAD-specific and LVAD-related infections. LVAD-specific infections refer to infections that are unique to patients with LVADs and might involve the pump, cannula, pump pocket, or driveline.137 Meanwhile, LVAD-related infections encompass non-endovascular infections, such as mediastinitis and the endovascular infections including bloodstream infections and infective endocarditis, all of which might also occur in patients without LVADs. Even though LVAD-related infections might not originate from LVADs per se, secondary involvement of the device is possible and it is generally difficult to make a confirmative diagnosis. Data from the International Society for Heart and Lung Transplantation Registry for Mechanically Assisted Circulatory Support covering 10 171 patients provided the www.thelancet.com Vol 404 July 27, 2024 most robust analyses on infections in LVAD patients to date. This registry showed that the LVAD-specific infection rate was 17·3%, which comprised infections in the driveline (82·9%), the pocket (12·8%), and the pump or cannula (4·3%).138 LVAD-related infections were a smaller category constituting 4·9%: 47·5% bloodstream infections and 47·5% mediastinitis. 1-year mortality rate after initial infection was 13·6% for driveline, 34·0% for pocket infections, and 41·5% for pump or cannula.138 Patients with LVAD-specific infections were found to have shorter median survival than those with LVADrelated infections. 139 Complete removal of the LVAD either by device exchange or by heart transplantation is optional, but with high risk in the setting of LVAD-associated endocarditis. For instance, in a recent meta-analysis on LVAD-associated endocarditis that involved 16 articles with 26 patients, the surgical mortality rate was as high as 28·6%, although it was lower than 72·6% for antibiotic therapy alone (p=0·07).140 Notably, within the surgical therapy group, there was no significant difference in the mortality rates between device exchange and heart transplantation (20·0% vs 33·3%, p=0·23). These findings indicate that further research is needed to optimise the therapeutic options for infectious complications occurring in LVADs.140 Transcatheter valve prosthetics and other intracardiac devices The risk of infective endocarditis is higher within the first year following transcatheter aortic valve implantation (TAVI). The incidence of infective endocarditis following TAVI ranges from 0·3 to 1·9 per 100 person-years, which is comparable with that observed in surgical aortic valve replacement (SAVR).141–145 However, the mortality was higher for patients with infective endocarditis following TAVI than for those following SAVR,143,144 which might be attributed to the older age and more comorbidities in that population. As for the treatment, antimicrobial therapy for infective endocarditis post-TAVI is similar to that of prosthetic valve endocarditis. Approximately 19% of cases of infective endocarditis following TAVI require cardiac surgery, whereas the rate is around 50% for infective endocarditis associated with SAVR.146 Cardiac surgeries in patients post-TAVI pose considerable risks due to advanced age, increased comorbidities, and the potential for complex surgical interventions because of the self-expanding devices in the ascending aorta. Cardiac surgery is considered first when combining any complications, particularly severe prosthetic failure or heart failure. Compared with antibiotics alone, cardiac surgery was not associated with reduced all-cause inhospital or 1-year mortality in post-TAVI infective endocarditis.146 Notably, the incidence of TAVI-associatedinfective endocarditis has decreased in recent years, particularly due to improvements in procedures and refinements of devices.147 385 Seminar The incidence of transcatheter pulmonary valve implantation varies from 1·6 to 4·0 per 100 personyears.148–155 Data on the incidence, outcomes, and treatment of infective endocarditis are restricted in patients with transcatheter mitral and tricuspid valve interventions, septal defect closure devices, left atrial appendage closure devices, vascular grafts, vena cava filters, and central venous system ventriculoatrial shunts. These patients are considered to have increased infective endocarditis risk in the first 6 months after the procedure.36 Hypertrophic cardiomyopathy Hypertrophic cardiomyopathy is an unusual cause of infective endocarditis, with an estimated incidence of 1·4 cases per 1000 person-years.156 Earlier reports suggested that patients with left ventricular outflow tract obstruction and left atrial dilatation are at high risk of endocarditis. However, later studies did not confirm this.157 The microbial spectrum, antibiotic choice, and outcomes of patients with hypertrophic cardiomyopathy are similar to those of other patients with streptococcal infections and could be more common. At present, antibiotic prophylaxis is not recommended. A strong argument is made by Dominguez and colleagues that patients with hypertrophic cardiomyopathy should receive antibiotic prophylaxis.158 Right-sided infective endocarditis Right-sided endocarditis is seen in about 5–10% of patients and its incidence has been increasing.159 Patients with congenital heart disease, CIED, indwelling intravenous catheters, chronic haemodialysis, intravenous drug use, and who are immunocompromised are predisposed.159 Pulmonary symptoms such as cough and haemoptysis are common. The tricuspid valve is often affected, with staphylococcus being the predominant organism. The prognosis is better compared with leftsided endocarditis. Although 90% of the patients respond to medical therapy, patients who are immuno­ compromised and those with fungal infections have a poor prognosis. Surgery is considered when the patient has persistent bacteraemia, right heart failure, respiratory failure, or has vegetations larger than 20 mm.160 Tricuspid valve repair is preferred over replacement.161 The endocarditis team The complexity of infective endocarditis necessitates diverse decision-making strategies and a multidisciplinary approach. The endocarditis team could facilitate early and accurate diagnosis of the primary disease and complications, initiating timely antibiotic therapy, determining the type and duration of antibiotics, and recommending early surgery.162–165 Previous studies have shown that the team-based approach reduced 1-year mortality by 7·5% to 10·3% in mixed cohorts.164,166 The core members of the endocarditis team typically include cardiologists, cardiovascular surgeons, infectious disease specialists, and microbiologists.167,168 The specific 386 makeup of the team should be tailored to meet the clinical needs of the patients and the capabilities of the health-care centre. In facilities without cardiovascular surgeons (known as referring centres), it is crucial to establish communication with fully equipped centres (referred to as heart valve centres) to coordinate optimal patient transfer timing for advanced diagnosis and treatment. These teams should maintain frequent communication and operate under standardised regulations to ensure effective management of infective endocarditis.167 Knowledge gaps The number of well-conducted RCTs studying infective endocarditis is restricted due to the rarity of the disease. Current recommendations often rely on observational studies. Considerable knowledge gaps need to be addressed in the field of infective endocarditis. Key areas lacking robust evidence extend across various aspects of infective endocarditis, including but not restricted to some areas (table 2). Accuracy of diagnosis There is no consensus on the most accurate diagnostic schema for infective endocarditis. Continued efforts are required to improve the accuracy of diagnostic testing for culture-negative infective endocarditis and elusive pathogens, such as Bartonella, C burnetiid, and fungi. The methodology to assess the size of the vegetation needs to be standardised. More research is needed to evaluate the diagnostic performance of intracardiac echocardiography in prosthetic-valve endocarditis and [¹⁸F]FDG-PET-CT in native-valve endocarditis. The role of molecular rapid diagnostic tests and [¹⁸F]FDG-PET-CT on outcomes in infective endocarditis needs to be clarified. Prevention strategies Further research is necessary to better define which patients would benefit from antibiotic prophylaxis and which invasive procedure requires antibiotic prophylaxis to prevent infective endocarditis. There is a need for robust evidence on the efficacy of various antibiotic prophylaxis regimens in preventing infective endo­ carditis. The effect of antibiotic prophylaxis on antimicrobial resistance needs to be determined. Optimal treatment There are uncertainties regarding the efficacy of empirical antibiotic regimens in treating known or suspected infective endocarditis, the efficacy and safety of recommended antimicrobial treatment regimens and new combinations of antimicrobials, and the effectiveness of combined antifungal therapy. Additionally, questions remain about the optimal medical strategies for specific pathogens, such as highly penicillin-resistant oral streptococci, staphylococci, high level aminoglycosideresistant Enterococcus faecalis, and vancomycin-resistant www.thelancet.com Vol 404 July 27, 2024 Seminar Knowledge gaps that need strong evidence from further research Proposed study designs Diagnosis Diagnostic schema Which diagnostic schema is the most accurate? What is the diagnostic accuracy of the different schema in diverse care settings? A Microbiology What is the accuracy of diagnostic testing for Bartonella infective endocarditis? A Microbiology What is the accuracy of diagnostic testing for Coxiella burnetii (Q fever) infective endocarditis? A Microbiology What is the accuracy of diagnosis of culture-negative infective endocarditis using molecular rapid diagnostic tests, or the determination of bacterial or fungal cell-free DNA in blood samples? A Microbiology What is the role of molecular and biochemical indicators to establish the diagnosis in fungal endocarditis? B Microbiology What is the effect of molecular rapid diagnostic tests on outcomes in infective endocarditis? C A Imaging What is the standard method to assess the size of the vegetations? Imaging What is the diagnostic performance of intracardiac echocardiography in prosthetic valve endocarditis? A Imaging What is the role of scoring systems in the identification of patients who might require a transoesophageal echocardiogram in the diagnosis of infective endocarditis? B Imaging What is the role of repeat echocardiograms in patients with an initial negative study suspected of having infective endocarditis or in patients with an established diagnosis of infective endocarditis? B Imaging What is the role of [¹⁸F]FDG-PET-CT in native valve endocarditis? B Imaging What is the ability of [¹⁸F]FDG-PET-CT to affect clinical outcomes of infective endocarditis? C Prevention Antibiotic prophylaxis Which patients can benefit from antibiotic prophylaxis to prevent infective endocarditis? C Antibiotic prophylaxis Which invasive procedure requires antibiotic prophylaxis to prevent infective endocarditis? C Antibiotic prophylaxis What is the efficacy of various antibiotic prophylaxis regimens in preventing infective endocarditis? C Antibiotic prophylaxis What is the effect of antibiotic prophylaxis on antimicrobial resistance? D or E Treatment Antimicrobial treatment What is the efficacy of different empirical antibiotic regimen therapies in treating known or suspected infective endocarditis? C Antimicrobial treatment What is the efficacy and safety of recommended antimicrobial treatment regimens and new combinations of antimicrobials? C Antimicrobial treatment What is the effective antibiotic treatment in patients with highly penicillin-resistant oral streptococci infective endocarditis? C or E Antimicrobial treatment What is the best medical strategy in staphylococcal infective endocarditis? C or E Antimicrobial treatment What are the effective antibiotic treatments for patients with high level aminoglycoside-resistant Enterococcus faecalis infective endocarditis and hypersensitivity to β-lactams? C or E Antimicrobial treatment What are the effective treatments for vancomycin-resistant enterococcal infective endocarditis? C or E Antimicrobial treatment What is the efficacy of combined antifungal therapy? C or E Antimicrobial treatment Are dual regimens, as used in the POET study,72 required for effective treatment? C Antimicrobial treatment To what extent is intravenous lead-in therapy needed before transitioning to oral therapy? C or E Antimicrobial treatment What is the duration of antibiotic therapy for infective endocarditis? C or E Surgery C What is the indication and timing of surgical treatment in patients with infective endocarditis? Surgery What is the need and timing of coronary angiogram before endocarditis surgery? C Surgery What is the timing and sequence of surgical interventions in patients with multiple septic sources? C or E C or E Surgery What is the efficacy and safety of vegetation extraction systems in right-sided infective endocarditis? Anticoagulation What is the appropriate anticoagulation regimen in patients with prosthetic valve endocarditis that is complicated by haemorrhagic stroke? C or E Management of other main complications What is the efficacy and safety of mechanical thrombectomy in infective endocarditis-related embolic strokes? C or E Management of other main complications What is the timing and safety of splenectomy for splenic abscess complicating infective endocarditis in relation to surgical valve treatment? E Long-term outcomes Outcomes What are the optimal timing, duration, methods, and components of rehabilitation? C Outcomes What is the efficacy of rehabilitation? C Outcomes What are the patient-reported outcomes during short-term and long-term follow-up? B [¹⁸F]FDG-PET-CT=[¹⁸F]fluorodeoxyglucose-PET-CT scan. A=multicentre prospective comparative studies. B=multicentre prospective observational studies. C=multicentre randomised controlled trials. D=multicentre prospective interventional studies. E=large-scale prospective registries with analysis performed with artificial intelligence. Table 2: Knowledge gaps in the field of infective endocarditis enterococci. The necessity of the dual antibiotic regimens used in the POET study need to be clarified. Further research is required to establish the extent of intravenous lead-in therapy before transitioning to oral therapy, the www.thelancet.com Vol 404 July 27, 2024 duration of antibiotic therapy, the indication and timing for surgical intervention, and the need for and timing of a coronary angiogram before endocarditis surgery. Other areas needing clarification include the timing and 387 Seminar sequence of interventions in patients with multiple septic sources, the appropriate anticoagulation regimen in patients with prosthetic valve endocarditis affected by haemorrhagic stroke, the efficacy and safety of mechanical thrombectomy in infective endocarditis-related embolic strokes, and the timing and safety of splenectomy for splenic abscess complicating infective endocarditis in relation to surgical valve treatment. Long-term outcomes and other considerations The optimal timing, duration, methods, components, and efficacy of rehabilitation need to be determined. There are a paucity of data on the short-term and longterm patient-reported outcomes, including recurrence rates, post-treatment sequelae, and the effect on quality of life. The use of artificial intelligence remains underexplored in patient management, such as identifying patients at high risk, predicting the appropriateness of surgical intervention and surgical timing, or better characterising vegetations to predict response to antibiotic therapy or risk of complications. Further research is also needed in post-discharge rehabilitation efficacy, patient-centred care, shared decision making, and sex-specific considerations. Management of specific situations, such as transcatheter valve therapies, left atrial appendage occlusion, CIED reimplantation following device removal after CIED infection, CIED removal in patients with leftsided infective endocarditis, and right-sided infective endocarditis demands rigorous study as well. Conclusion Infective endocarditis remains a formidable challenge, emphasising the need for a multidisciplinary approach in both management and research. Despite progress, crucial questions persist demanding urgent RCTs to enhance our understanding of infective endocarditis. Advances in microbiological services, imaging technology, and artificial intelligence-driven machine learning offer promising avenues for improved patient outcomes. Only with coordinated and sustained efforts can we effectively confront the evolving nature of infective endocarditis and strive for continued advancements in patient care and outcomes. Contributors ML, JBK, BKSS, and MC jointly drafted and revised the manuscript. 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Declaration of interests We declare no competing interests. 23 Acknowledgments The authors are grateful to Yanjuan Zhang, Le Geng, and Jun Wang for assistance with images. 24 References 1 Geller SA. Infective endocarditis: a history of the development of its understanding. Autops Case Rep 2013; 3: 5–12. 2 Lerner PI, Weinstein L. Infective endocarditis in the antibiotic era. N Engl J Med 1966; 274: 199–206. 3 Lerner PI, Weinstein L. Infective endocarditis in the antibiotic era. N Engl J Med 1966; 274: 259–66. 388 4 25 26 Lerner PI, Weinstein L. Infective endocarditis in the antibiotic era. N Engl J Med 1966; 274: 388–93. Hackett AJ, Stuart J. Infective endocarditis: identification and management in the emergency department. Emerg Med Pract 2020; 22: 1–24. Wang A, Athan E, Pappas PA, et al. Contemporary clinical profile and outcome of prosthetic valve endocarditis. JAMA 2007; 297: 1354–61. Chen H, Zhan Y, Zhang K, et al. The global, regional, and national burden and trends of infective endocarditis from 1990 to 2019: results from the Global Burden of Disease Study 2019. Front Med 2022; 9: 774224. Tleyjeh IM, Steckelberg JM, Murad HS, et al. Temporal trends in infective endocarditis: a population-based study in Olmsted County, Minnesota. JAMA 2005; 293: 3022–28. Slipczuk L, Codolosa JN, Davila CD, et al. Infective endocarditis epidemiology over five decades: a systematic review. PLoS One 2013; 8: e82665. Polishchuk I, Stavi V, Awesat J, et al. Sex differences in infective endocarditis. Am J Med Sci 2021; 361: 83–89. Hammond-Haley M, Hartley A, Al-Khayatt BM, et al. Trends in the incidence and mortality of infective endocarditis in high-income countries between 1990 and 2019. Int J Cardiol 2023; 371: 441–51. Shah ASV, McAllister DA, Gallacher P, et al. Incidence, microbiology, and outcomes in patients hospitalized with infective endocarditis. Circulation 2020; 141: 2067–77. Li HL, Tromp J, Teramoto K, et al. Temporal trends and patterns of infective endocarditis in a Chinese population: a territory-wide study in Hong Kong (2002–2019). Lancet Reg Health West Pac 2022; 22: 100417. Yucel E, Bearnot B, Paras ML, et al. Diagnosis and management of infective endocarditis in people who inject drugs: JACC state-of-theart review. J Am Coll Cardiol 2022; 79: 2037–57. Sengupta SP, Prendergast B, Laroche C, et al. Socioeconomic variations determine the clinical presentation, aetiology, and outcome of infective endocarditis: a prospective cohort study from the ESC-EORP EURO-ENDO (European Infective Endocarditis) registry. Eur Heart J Qual Care Clin Outcomes 2022; 9: 85–96. Noubiap JJ, Nkeck JR, Kwondom BS, Nyaga UF. Epidemiology of infective endocarditis in Africa: a systematic review and metaanalysis. Lancet Glob Health 2022; 10: e77–86. Njuguna B, Gardner A, Karwa R, Delahaye F. Infective endocarditis in low- and middle-income countries. Cardiol Clin 2017; 35: 153–63. Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med 2009; 169: 463–73. Nappi F, Martuscelli G, Bellomo F, Avtaar Singh SS, Moon MR. Infective endocarditis in high-income countries. Metabolites 2022; 12: 682. Lockhart PB, Brennan MT, Sasser HC, Fox PC, Paster BJ, Bahrani-Mougeot FK. Bacteremia associated with toothbrushing and dental extraction. Circulation 2008; 117: 3118–25. Kim JB, Ejiofor JI, Yammine M, et al. Surgical outcomes of infective endocarditis among intravenous drug users. J Thorac Cardiovasc Surg 2016; 152: 832–41.e1. Widmer E, Que YA, Entenza JM, Moreillon P. New concepts in the pathophysiology of infective endocarditis. Curr Infect Dis Rep 2006; 8: 271–79. Moreillon P, Que YA, Bayer AS. Pathogenesis of streptococcal and staphylococcal endocarditis. Infect Dis Clin North Am 2002; 16: 297–318. Mancini S, Oechslin F, Menzi C, et al. Marginal role of von Willebrand factor-binding protein and coagulase in the initiation of endocarditis in rats with catheter-induced aortic vegetations. Virulence 2018; 9: 1615–24. Vestby LK, Grønseth T, Simm R, Nesse LL. Bacterial biofilm and its role in the pathogenesis of disease. Antibiotics 2020; 9: 59. Urina-Jassir M, Jaimes-Reyes MA, Martinez-Vernaza S, Quiroga-Vergara C, Urina-Triana M. Clinical, microbiological, and imaging characteristics of infective endocarditis in Latin America: a systematic review. Int J Infect Dis 2022; 117: 312–21. www.thelancet.com Vol 404 July 27, 2024 Seminar 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 Toyoda N, Chikwe J, Itagaki S, Gelijns AC, Adams DH, Egorova NN. Trends in infective endocarditis in California and New York State, 1998–2013. JAMA 2017; 317: 1652–60. Ambrosioni J, Hernández-Meneses M, Durante-Mangoni E, et al. Epidemiological changes and improvement in outcomes of infective endocarditis in Europe in the twenty-first century: an International Collaboration on Endocarditis (ICE) prospective cohort study (2000–2012). Infect Dis Ther 2023; 12: 1083–101. Tarakji KG, Ellis CR, Defaye P, Kennergren C. Cardiac implantable electronic device infection in patients at risk. Arrhythm Electrophysiol Rev 2016; 5: 65–71. Habib G, Erba PA, Iung B, et al. Clinical presentation, aetiology and outcome of infective endocarditis. Results of the ESC-EORP EURO-ENDO (European infective endocarditis) registry: a prospective cohort study. Eur Heart J 2019; 40: 3222–32. Niederman MS, Baron RM, Bouadma L, et al. Initial antimicrobial management of sepsis. Crit Care 2021; 25: 307. Snipsøyr MG, Ludvigsen M, Petersen E, Wiggers H, Honoré B. A systematic review of biomarkers in the diagnosis of infective endocarditis. Int J Cardiol 2016; 202: 564–70. Snipsøyr MG, Wiggers H, Ludvigsen M, et al. Towards identification of novel putative biomarkers for infective endocarditis by serum proteomic analysis. Int J Infect Dis 2020; 96: 73–81. Cockerill FR 3rd, Wilson JW, Vetter EA, et al. Optimal testing parameters for blood cultures. Clin Infect Dis 2004; 38: 1724–30. Lee A, Mirrett S, Reller LB, Weinstein MP. Detection of bloodstream infections in adults: how many blood cultures are needed? J Clin Microbiol 2007; 45: 3546–48. Delgado V, Ajmone Marsan N, de Waha S, et al. 2023 ESC guidelines for the management of endocarditis. Eur Heart J 2023; 44: 3948–4042. Burckhardt I, Zimmermann S. Susceptibility testing of bacteria using Maldi-Tof mass spectrometry. Front Microbiol 2018; 9: 1744. Brouqui P, Raoult D. Endocarditis due to rare and fastidious bacteria. Clin Microbiol Rev 2001; 14: 177–207. Fournier PE, Thuny F, Richet H, et al. Comprehensive diagnostic strategy for blood culture-negative endocarditis: a prospective study of 819 new cases. Clin Infect Dis 2010; 51: 131–40. Fournier PE, Gouriet F, Casalta JP, et al. Blood culture-negative endocarditis: improving the diagnostic yield using new diagnostic tools. Medicine 2017; 96: e8392. Das M, Badley AD, Cockerill FR, Steckelberg JM, Wilson WR. Infective endocarditis caused by HACEK microorganisms. Annu Rev Med 1997; 48: 25–33. Shapira L, Rasis M, Binsky Ehrenreich I, et al. Laboratory diagnosis of 37 cases of Bartonella endocarditis based on enzyme immunoassay and real-time PCR. J Clin Microbiol 2021; 59: e02217–20. Ransom EM, Alipour Z, Wallace MA, Burnham CA. Evaluation of optimal blood culture incubation time to maximize clinically relevant results from a contemporary blood culture instrument and media system. J Clin Microbiol 2021; 59: e02459–20. Petti CA, Bhally HS, Weinstein MP, et al. Utility of extended blood culture incubation for isolation of Haemophilus, Actinobacillus, Cardiobacterium, Eikenella, and Kingella organisms: a retrospective multicenter evaluation. J Clin Microbiol 2006; 44: 257–59. Liesman RM, Pritt BS, Maleszewski JJ, Patel R. Laboratory diagnosis of infective endocarditis. J Clin Microbiol 2017; 55: 2599–608. Li SL, Zhao X, Tao JZ, Yue ZZ, Zhao XY. Application of metagenomic next-generation sequencing in patients with infective endocarditis. Front Cell Infect Microbiol 2023; 13: 1107170. Habib G, Badano L, Tribouilloy C, et al. Recommendations for the practice of echocardiography in infective endocarditis. Eur J Echocardiogr 2010; 11: 202–19. Bai AD, Steinberg M, Showler A, et al. Diagnostic accuracy of transthoracic echocardiography for infective endocarditis findings using transesophageal echocardiography as the reference standard: a meta-analysis. J Am Soc Echocardiogr 2017; 30: 639–46. Rasmussen RV, Høst U, Arpi M, et al. Prevalence of infective endocarditis in patients with Staphylococcus aureus bacteraemia: the value of screening with echocardiography. Eur J Echocardiogr 2011; 12: 414–20. www.thelancet.com Vol 404 July 27, 2024 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 Vieira ML, Grinberg M, Pomerantzeff PM, Andrade JL, Mansur AJ. Repeated echocardiographic examinations of patients with suspected infective endocarditis. Heart 2004; 90: 1020–24. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation 2015; 132: 1435–86. Liu YW, Tsai WC, Lin CC, et al. Usefulness of real-time threedimensional echocardiography for diagnosis of infective endocarditis. Scand Cardiovasc J 2009; 43: 318–23. Berdejo J, Shibayama K, Harada K, et al. Evaluation of vegetation size and its relationship with embolism in infective endocarditis: a real-time 3-dimensional transesophageal echocardiography study. Circ Cardiovasc Imaging 2014; 7: 149–54. Feuchtner GM, Stolzmann P, Dichtl W, et al. Multislice computed tomography in infective endocarditis: comparison with transesophageal echocardiography and intraoperative findings. J Am Coll Cardiol 2009; 53: 436–44. Kim IC, Chang S, Hong GR, et al. Comparison of cardiac computed tomography with transesophageal echocardiography for identifying vegetation and intracardiac complications in patients with infective endocarditis in the era of 3-dimensional images. Circ Cardiovasc Imaging 2018; 11: e006986. Oliveira M, Guittet L, Hamon M, Hamon M. Comparative value of cardiac CT and transesophageal echocardiography in infective endocarditis: a systematic review and meta-analysis. Radiol Cardiothorac Imaging 2020; 2: e190189. Wang TKM, Sánchez-Nadales A, Igbinomwanhia E, Cremer P, Griffin B, Xu B. Diagnosis of infective endocarditis by subtype using 18F-fluorodeoxyglucose positron emission tomography/ computed tomography: a contemporary meta-analysis. Circ Cardiovasc Imaging 2020; 13: e010600. Duval X, Le Moing V, Tubiana S, et al. Impact of systematic wholebody 18F-fluorodeoxyglucose PET/CT on the management of patients suspected of infective endocarditis: the prospective multicenter TEPvENDO study. Clin Infect Dis 2021; 73: 393–403. de Camargo RA, Sommer Bitencourt M, Meneghetti JC, et al. The role of 18F-fluorodeoxyglucose positron emission tomography/ computed tomography in the diagnosis of left-sided endocarditis: native vs prosthetic valves endocarditis. Clin Infect Dis 2020; 70: 583–94. Snygg-Martin U, Gustafsson L, Rosengren L, et al. Cerebrovascular complications in patients with left-sided infective endocarditis are common: a prospective study using magnetic resonance imaging and neurochemical brain damage markers. Clin Infect Dis 2008; 47: 23–30. Cooper HA, Thompson EC, Laureno R, et al. Subclinical brain embolization in left-sided infective endocarditis: results from the evaluation by MRI of the brains of patients with left-sided intracardiac solid masses (EMBOLISM) pilot study. Circulation 2009; 120: 585–91. Huang JS, Ho AS, Ahmed A, Bhalla S, Menias CO. Borne identity: CT imaging of vascular infections. Emerg Radiol 2011; 18: 335–43. Feil K, Küpper C, Tiedt S, et al. Safety and efficacy of mechanical thrombectomy in infective endocarditis: a matched case-control analysis from the German Stroke Registry–endovascular treatment. Eur J Neurol 2021; 28: 861–67. Caldonazo T, Musleh R, Moschovas A, et al. Antithrombotic therapy in patients with infective endocarditis. JACC Adv 2024; 3: 100768. Park W, Ahn JS, Park JC, Kwun BD, Lee DH. Treatment strategy based on experience of treating intracranial infectious aneurysms. World Neurosurg 2017; 97: 351–59. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Am J Med 1994; 96: 200–09. Li JS, Sexton DJ, Mick N, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 2000; 30: 633–38. Fowler VG Jr, Durack DT, Selton-Suty C, et al. The 2023 Duke– International Society for Cardiovascular Infectious Diseases Criteria for Infective Endocarditis: updating the modified Duke criteria. Clin Infect Dis 2023; 77: 518–26. 389 Seminar 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 390 van der Vaart TW, Bossuyt PMM, Durack DT, et al. External validation of the 2023 Duke–International Society for Cardiovascular Infectious Diseases Diagnostic Criteria for Infective Endocarditis. Clin Infect Dis 2004; 78: 922–29. Prendergast BD. Diagnostic criteria and problems in infective endocarditis. Heart 2004; 90: 611–13. Martí-Carvajal AJ, Dayer M, Conterno LO, Gonzalez Garay AG, Martí-Amarista CE. A comparison of different antibiotic regimens for the treatment of infective endocarditis. Cochrane Database Syst Rev 2020; 5: CD009880. Iversen K, Ihlemann N, Gill SU, et al. Partial oral versus intravenous antibiotic treatment of endocarditis. N Engl J Med 2019; 380: 415–24. Kang DH, Kim YJ, Kim SH, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med 2012; 366: 2466–73. Jussli-Melchers J, Friedrich C, Mandler K, et al. Risk factor analysis for 30-day mortality after surgery for infective endocarditis. Thorac Cardiovasc Surg 2024; published online Feb 19. https://doi.org/10.1055/s-0044-1779709. Vallejo Camazon N, Mateu L, Cediel G, et al. Long-term antibiotic therapy in patients with surgery-indicated not undergoing surgery infective endocarditis. Cardiol J 2021; 28: 566–78. Iung B, Doco-Lecompte T, Chocron S, et al. Cardiac surgery during the acute phase of infective endocarditis: discrepancies between European Society of Cardiology guidelines and practices. Eur Heart J 2016; 37: 840–48. Park LP, Chu VH, Peterson G, et al. Validated risk score for predicting 6-month mortality in infective endocarditis. J Am Heart Assoc 2016; 5: e003016. Fernandez-Felix BM, Barca LV, Garcia-Esquinas E, et al. Prognostic models for mortality after cardiac surgery in patients with infective endocarditis: a systematic review and aggregation of prediction models. Clin Microbiol Infect 2021; 27: 1422–30. Chu VH, Park LP, Athan E, et al. Association between surgical indications, operative risk, and clinical outcome in infective endocarditis: a prospective study from the International Collaboration on Endocarditis. Circulation 2015; 131: 131–40. Varela Barca L, Fernández-Felix BM, Navas Elorza E, et al. Prognostic assessment of valvular surgery in active infective endocarditis: multicentric nationwide validation of a new score developed from a meta-analysis. Eur J Cardiothorac Surg 2020; 57: 724–31. Varela Barca L, Navas Elorza E, Fernández-Hidalgo N, et al. Prognostic factors of mortality after surgery in infective endocarditis: systematic review and meta-analysis. Infection 2019; 47: 879–95. Musci M, Weng Y, Hübler M, et al. Homograft aortic root replacement in native or prosthetic active infective endocarditis: twenty-year singlecenter experience. J Thorac Cardiovasc Surg 2010; 139: 665–73. Rudasill SE, Sanaiha Y, Mardock AL, et al. Clinical outcomes of infective endocarditis in injection drug users. J Am Coll Cardiol 2019; 73: 559–70. Arjomandi Rad A, Zubarevich A, Osswald A, et al. The surgical treatment of infective endocarditis: a comprehensive review. Diagnostics 2024; 14: 464. Straw S, Baig MW, Gillott R, et al. Long-term outcomes are poor in intravenous drug users following infective endocarditis, even after surgery. Clin Infect Dis 2020; 71: 564–71. Chan KL, Dumesnil JG, Cujec B, et al. A randomized trial of aspirin on the risk of embolic events in patients with infective endocarditis. J Am Coll Cardiol 2003; 42: 775–80. Scheggi V, Merilli I, Marcucci R, et al. Predictors of mortality and adverse events in patients with infective endocarditis: a retrospective real world study in a surgical centre. BMC Cardiovasc Disord 2021; 21: 28. Yoshioka D, Toda K, Yokoyama JY, et al. Diabetes mellitus adversely affects mortality and recurrence after valve surgery for infective endocarditis. J Thorac Cardiovasc Surg 2018; 155: 1021–29. Ternhag A, Cederström A, Törner A, Westling K. A nationwide cohort study of mortality risk and long-term prognosis in infective endocarditis in Sweden. PLoS One 2013; 8: e67519. Fernández-Hidalgo N, Almirante B, Tornos P, et al. Immediate and long-term outcome of left-sided infective endocarditis. A 12-year prospective study from a contemporary cohort in a referral hospital. Clin Microbiol Infect 2012; 18: E522–30. 91 Thuny F, Giorgi R, Habachi R, et al. Excess mortality and morbidity in patients surviving infective endocarditis. Am Heart J 2012; 164: 94–101. 92 Martínez-Sellés M, Muñoz P, Estevez A, et al. Long-term outcome of infective endocarditis in non-intravenous drug users. Mayo Clin Proc 2008; 83: 1213–17. 93 Citro R, Chan KL, Miglioranza MH, et al. Clinical profile and outcome of recurrent infective endocarditis. Heart 2022; 108: 1729–36. 94 Agrawal A, Virk HUH, Riaz I, et al. Predictors of 30-day readmissions in patients with infective endocarditis: a national population based cohort study. Rev Cardiovasc Med 2020; 21: 123–27. 95 Freitas-Ferraz AB, Tirado-Conte G, Vilacosta I, et al. Contemporary epidemiology and outcomes in recurrent infective endocarditis. Heart 2020; 106: 596–602. 96 Alagna L, Park LP, Nicholson BP, et al. Repeat endocarditis: analysis of risk factors based on the International Collaboration on Endocarditis – prospective cohort study. Clin Microbiol Infect 2014; 20: 566–75. 97 Chu VH, Sexton DJ, Cabell CH, et al. Repeat infective endocarditis: differentiating relapse from reinfection. Clin Infect Dis 2005; 41: 406–09. 98 Hays LH. Infective endocarditis: call for education of adults with CHD: review of the evidence. Cardiol Young 2016; 26: 426–30. 99 Thornhill MH, Jones S, Prendergast B, et al. Quantifying infective endocarditis risk in patients with predisposing cardiac conditions. Eur Heart J 2018; 39: 586–95. 100 Duval X, Millot S, Chirouze C, et al. Oral streptococcal endocarditis, oral hygiene habits, and recent dental procedures: a case-control study. Clin Infect Dis 2017; 64: 1678–85. 101 Sy RW, Kritharides L. Health care exposure and age in infective endocarditis: results of a contemporary population-based profile of 1536 patients in Australia. Eur Heart J 2010; 31: 1890–97. 102 Janszky I, Gémes K, Ahnve S, Asgeirsson H, Möller J. Invasive procedures associated with the development of infective endocarditis. J Am Coll Cardiol 2018; 71: 2744–52. 103 Thornhill MH, Crum A, Campbell R, et al. Temporal association between invasive procedures and infective endocarditis. Heart 2023; 109: 223–31. 104 Lockhart PB, Chu V, Zhao J, et al. Oral hygiene and infective endocarditis: a case control study. Oral Surg Oral Med Oral Pathol Oral Radiol 2023; 136: 333–42. 105 Wilson W, Taubert KA, Gewitz M, et al. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation 2007; 116: 1736–54. 106 Habib G, Hoen B, Tornos P, et al. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Eur Heart J 2009; 30: 2369–413. 107 Thornhill M, Prendergast B, Dayer M, Frisby A, Baddour LM. Endocarditis prevention: time for a review of NICE guidance. Lancet Reg Health Eur 2024; 39: 100876. 108 Thornhill MH, Gibson TB, Yoon F, et al. Antibiotic prophylaxis against infective endocarditis before invasive dental procedures. J Am Coll Cardiol 2022; 80: 1029–41. 109 Thornhill MH, Gibson TB, Yoon F, et al. Endocarditis, invasive dental procedures, and antibiotic prophylaxis efficacy in US Medicaid patients. Oral Dis 2024; 30: 1591–605. 110 Thornhill MH, Dayer MJ, Prendergast B, Baddour LM, Jones S, Lockhart PB. Incidence and nature of adverse reactions to antibiotics used as endocarditis prophylaxis. J Antimicrob Chemother 2015; 70: 2382–88. 111 Franklin M, Wailoo A, Dayer MJ, et al. The cost-effectiveness of antibiotic prophylaxis for patients at risk of infective endocarditis. Circulation 2016; 134: 1568–78. 112 Baddour LM, Janszky I, Thornhill MH, et al. Nondental invasive procedures and risk of infective endocarditis: time for a revisit: a science advisory from the American Heart Association. Circulation 2023; 148: 1529–41. www.thelancet.com Vol 404 July 27, 2024 Seminar 113 Brown KA, Khanafer N, Daneman N, Fisman DN. Meta-analysis of antibiotics and the risk of community-associated Clostridium difficile infection. Antimicrob Agents Chemother 2013; 57: 2326–32. 114 Thornhill MH, Dayer MJ, Durkin MJ, Lockhart PB, Baddour LM. Risk of adverse reactions to oral antibiotics prescribed by dentists. J Dent Res 2019; 98: 1081–87. 115 Wilson WR, Gewitz M, Lockhart PB, et al. Prevention of viridans group streptococcal infective endocarditis: a scientific statement from the American Heart Association. Circulation 2021; 143: e963–78. 116 Pyo WK, Kim HJ, Kim JB, et al. Comparative surgical outcomes of prosthetic and native valve endocarditis. Korean Circ J 2021; 51: 504–14. 117 Moreillon P, Que YA. Infective endocarditis. Lancet 2004; 363: 139–49. 118 Hoen B, Alla F, Selton-Suty C, et al. Changing profile of infective endocarditis: results of a 1-year survey in France. JAMA 2002; 288: 75–81. 119 Brennan JM, Edwards FH, Zhao Y, et al. Long-term safety and effectiveness of mechanical versus biologic aortic valve prostheses in older patients: results from the Society of Thoracic Surgeons Adult Cardiac Surgery National Database. Circulation 2013; 127: 1647–55. 120 López J, Revilla A, Vilacosta I, et al. Definition, clinical profile, microbiological spectrum, and prognostic factors of early-onset prosthetic valve endocarditis. Eur Heart J 2007; 28: 760–65. 121 Moriyama N, Laakso T, Biancari F, et al. Prosthetic valve endocarditis after transcatheter or surgical aortic valve replacement with a bioprosthesis: results from the FinnValve Registry. EuroIntervention 2019; 15: e500–07. 122 Kohler P, Kuster SP, Bloemberg G, et al. Healthcare-associated prosthetic heart valve, aortic vascular graft, and disseminated Mycobacterium chimaera infections subsequent to open heart surgery. Eur Heart J 2015; 36: 2745–53. 123 Joy PS, Kumar G, Poole JE, London B, Olshansky B. Cardiac implantable electronic device infections: who is at greatest risk? Heart Rhythm 2017; 14: 839–45. 124 Viganego F, O’Donoghue S, Eldadah Z, et al. Effect of early diagnosis and treatment with percutaneous lead extraction on survival in patients with cardiac device infections. Am J Cardiol 2012; 109: 1466–71. 125 Birnie DH, Healey JS, Wells GA, et al. Continued vs interrupted direct oral anticoagulants at the time of device surgery, in patients with moderate to high risk of arterial thrombo-embolic events (BRUISE CONTROL-2). Eur Heart J 2018; 39: 3973–79. 126 Birnie DH, Healey JS, Wells GA, et al. Pacemaker or defibrillator surgery without interruption of anticoagulation. N Engl J Med 2013; 368: 2084–93. 127 Victor F, De Place C, Camus C, et al. Pacemaker lead infection: echocardiographic features, management, and outcome. Heart 1999; 81: 82–87. 128 Fowler VG Jr, Li J, Corey GR, et al. Role of echocardiography in evaluation of patients with Staphylococcus aureus bacteremia: experience in 103 patients. J Am Coll Cardiol 1997; 30: 1072–78. 129 Vilacosta I, Sarriá C, San Román JA, et al. Usefulness of transesophageal echocardiography for diagnosis of infected transvenous permanent pacemakers. Circulation 1994; 89: 2684–87. 130 Blomström-Lundqvist C, Traykov V, Erba PA, et al. European Heart Rhythm Association (EHRA) international consensus document on how to prevent, diagnose, and treat cardiac implantable electronic device infections-endorsed by the Heart Rhythm Society (HRS), the Asia Pacific Heart Rhythm Society (APHRS), the Latin American Heart Rhythm Society (LAHRS), International Society for Cardiovascular Infectious Diseases (ISCVID) and the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Europace 2020; 22: 515–49. 131 Lin AY, Saul T, Aldaas OM, et al. Early versus delayed lead extraction in patients with infected cardiovascular implantable electronic devices. JACC Clin Electrophysiol 2021; 7: 755–63. 132 Le KY, Sohail MR, Friedman PA, et al. Impact of timing of device removal on mortality in patients with cardiovascular implantable electronic device infections. Heart Rhythm 2011; 8: 1678–85. www.thelancet.com Vol 404 July 27, 2024 133 De Ciancio G, Erpelding ML, Filippetti L, et al. Adherence to diagnostic and therapeutic practice guidelines for suspected cardiac implantable electronic device infections. Arch Cardiovasc Dis 2021; 114: 634–46. 134 Rushani D, Kaufman JS, Ionescu-Ittu R, et al. Infective endocarditis in children with congenital heart disease: cumulative incidence and predictors. Circulation 2013; 128: 1412–19. 135 Kuijpers JM, Koolbergen DR, Groenink M, et al. Incidence, risk factors, and predictors of infective endocarditis in adult congenital heart disease: focus on the use of prosthetic material. Eur Heart J 2017; 38: 2048–56. 136 Ly R, Compain F, Gaye B, et al. Predictive factors of death associated with infective endocarditis in adult patients with congenital heart disease. Eur Heart J Acute Cardiovasc Care 2021; 10: 320–28. 137 Hannan MM, Husain S, Mattner F, et al. Working formulation for the standardization of definitions of infections in patients using ventricular assist devices. J Heart Lung Transplant 2011; 30: 375–84. 138 Hannan MM, Xie R, Cowger J, et al. Epidemiology of infection in mechanical circulatory support: a global analysis from the ISHLT Mechanically Assisted Circulatory Support Registry. J Heart Lung Transplant 2019; 38: 364–73. 139 Blanco-Guzman MO, Wang X, Vader JM, Olsen MA, Dubberke ER. Epidemiology of left ventricular assist device infections: findings from a large nonregistry cohort. Clin Infect Dis 2021; 72: 190–97. 140 Patel S, Rizvi SSA, Choi JH, et al. Management and outcomes of left ventricular assist device-associated endocarditis: a systematic review. Ann Cardiothorac Surg 2019; 8: 600–09. 141 Stortecky S, Heg D, Tueller D, et al. Infective endocarditis after transcatheter aortic valve replacement. J Am Coll Cardiol 2020; 75: 3020–30. 142 Regueiro A, Linke A, Latib A, et al. Association between transcatheter aortic valve replacement and subsequent infective endocarditis and in-hospital death. JAMA 2016; 316: 1083–92. 143 Butt JH, Ihlemann N, De Backer O, et al. Long-term risk of infective endocarditis after transcatheter aortic valve replacement. J Am Coll Cardiol 2019; 73: 1646–55. 144 Fauchier L, Bisson A, Herbert J, et al. Incidence and outcomes of infective endocarditis after transcatheter aortic valve implantation versus surgical aortic valve replacement. Clin Microbiol Infect 2020; 26: 1368–74. 145 Kolte D, Goldsweig A, Kennedy KF, et al. Comparison of incidence, predictors, and outcomes of early infective endocarditis after transcatheter aortic valve implantation versus surgical aortic valve replacement in the United States. Am J Cardiol 2018; 122: 2112–19. 146 Mangner N, del Val D, Abdel-Wahab M, et al. Surgical treatment of patients with infective endocarditis after transcatheter aortic valve implantation. J Am Coll Cardiol 2022; 79: 772–85. 147 Mentias A, Girotra S, Desai MY, et al. Incidence, predictors, and outcomes of endocarditis after transcatheter aortic valve replacement in the United States. JACC Cardiovasc Interv 2020; 13: 1973–82. 148 McElhinney DB, Sondergaard L, Armstrong AK, et al. Endocarditis after transcatheter pulmonary valve replacement. J Am Coll Cardiol 2018; 72: 2717–28. 149 Bos D, De Wolf D, Cools B, et al. Infective endocarditis in patients after percutaneous pulmonary valve implantation with the stentmounted bovine jugular vein valve: clinical experience and evaluation of the modified Duke criteria. Int J Cardiol 2021; 323: 40–46. 150 Georgiev S, Ewert P, Eicken A, et al. Munich comparative study: prospective long-term outcome of the transcatheter melody valve versus surgical pulmonary bioprosthesis with up to 12 years of follow-up. Circ Cardiovasc Interv 2020; 13: e008963. 151 Gröning M, Tahri NB, Søndergaard L, Helvind M, Ersbøll MK, Ørbæk Andersen H. Infective endocarditis in right ventricular outflow tract conduits: a register-based comparison of homografts, Contegra grafts and Melody transcatheter valves. Eur J Cardiothorac Surg 2019; 56: 87–93. 152 Lluri G, Levi DS, Miller E, et al. Incidence and outcome of infective endocarditis following percutaneous versus surgical pulmonary valve replacement. Catheter Cardiovasc Interv 2018; 91: 277–84. 153 Malekzadeh-Milani S, Houeijeh A, Jalal Z, et al. French national survey on infective endocarditis and the Melody valve in percutaneous pulmonary valve implantation. Arch Cardiovasc Dis 2018; 111: 497–506. 391 Seminar 154 McElhinney DB, Zhang Y, Aboulhosn JA, et al. Multicenter study of endocarditis after transcatheter pulmonary valve replacement. J Am Coll Cardiol 2021; 78: 575–89. 155 Nordmeyer J, Ewert P, Gewillig M, et al. Acute and midterm outcomes of the post-approval MELODY Registry: a multicentre registry of transcatheter pulmonary valve implantation. Eur Heart J 2019; 40: 2255–64. 156 Spirito P, Rapezzi C, Bellone P, et al. Infective endocarditis in hypertrophic cardiomyopathy: prevalence, incidence, and indications for antibiotic prophylaxis. Circulation 1999; 99: 2132–37. 157 Sims JR, Anavekar NS, Bhatia S, et al. Clinical, radiographic, and microbiologic features of infective endocarditis in patients with hypertrophic cardiomyopathy. Am J Cardiol 2018; 121: 480–84. 158 Dominguez F, Ramos A, Bouza E, et al. Infective endocarditis in hypertrophic cardiomyopathy: a multicenter, prospective, cohort study. Medicine 2016; 95: e4008. 159 Shmueli H, Thomas F, Flint N, Setia G, Janjic A, Siegel RJ. Right-sided infective endocarditis 2020: challenges and updates in diagnosis and treatment. J Am Heart Assoc 2020; 9: e017293. 160 Pettersson GB, Hussain ST. Current AATS guidelines on surgical treatment of infective endocarditis. Ann Cardiothorac Surg 2019; 8: 630–44. 161 Yanagawa B, Elbatarny M, Verma S, et al. Surgical management of tricuspid valve infective endocarditis: a systematic review and metaanalysis. Ann Thorac Surg 2018; 106: 708–14. 162 El-Dalati S, Cronin D, Riddell J 4th, et al. The clinical impact of implementation of a multidisciplinary endocarditis team. Ann Thorac Surg 2022; 113: 118–24. 392 163 Camou F, Dijos M, Barandon L, et al. Management of infective endocarditis and multidisciplinary approach. Med Mal Infect 2019; 49: 17–22. 164 Kaura A, Byrne J, Fife A, et al. Inception of the ‘endocarditis team’ is associated with improved survival in patients with infective endocarditis who are managed medically: findings from a beforeand-after study. Open Heart 2017; 4: e000699. 165 Davierwala PM, Marin-Cuartas M, Misfeld M, Borger MA. The value of an “endocarditis team”. Ann Cardiothorac Surg 2019; 8: 621–29. 166 Botelho-Nevers E, Thuny F, Casalta JP, et al. Dramatic reduction in infective endocarditis-related mortality with a management-based approach. Arch Intern Med 2009; 169: 1290–98. 167 Mestres CA, Paré JC, Miró JM. Organization and functioning of a multidisciplinary team for the diagnosis and treatment of infective endocarditis: a 30-year perspective (1985–2014). Rev Esp Cardiol 2015; 68: 363–68. 168 El-Dalati S, Cronin D, Riddell J 4th, et al. A step-by-step guide to implementing a multidisciplinary endocarditis team. Ther Adv Infect Dis 2021; 8: 20499361211065596. Copyright © 2024 Elsevier Ltd. All rights reserved, including those for text and data mining, AI training, and similar technologies. www.thelancet.com Vol 404 July 27, 2024