LEVAQUIN® (levofloxacin IV/tablets)
advertisement
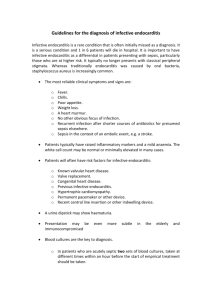
A 44-year-old man with a 2-month history of weight loss, fatigue, cough, and night sweats Joe Kovaz, M.D. December 8, 2004 No financial disclosures 9/2/04 44 yo man with the following problems: – Ischemic Heart Disease (stenting of right coronary artery 10/01) – Ventricular Septal Defect and Atrial Septal Defect – Tobacco Addiction (2 packs daily for many years) – Type II Diabetes Mellitus – Obstructive Sleep Apnea – Hyperlipidemia – Hypertension – Chronic cellulitis/erysipelas of left leg 9/2/04 Discontinued all of his medications one week prior to his visit because: “They were killing me.” – Simvastatin 80 mg – Niaspan 2000 mg – Losartan/hydrochlorothiazide 100/25 – Aspirin 325 mg – Atenolol 100 mg – Spironolactone 25 mg twice a day – Metformin 500 mg twice a day – Flonase Had multiple dental extractions done in early June while taking dicloxacillin 1 gram twice a day and benzathine penicillin 1.2 million units every four weeks. Had been on this regimen since 9/03. Felt somewhat better after stopping his medications, but still had a cough and night sweats. Past Medical History Chronic cellulitis/erysipelas began in 10/02 after he was hit in the left leg with a sledge hammer by one son and a week later with a brick by another son. Admitted for incision and drainage of an abscess of the left leg. …had six additional episodes of cellulitis from 10/02 to 8/03 which responded to oral antibiotics, except for one episode requiring admission. Past Medical History, continued 8/21/03 First seen by Dr. Vogelman, who initiated treatment with dicloxacillin for recurrent cellulitis and terbinafine for tenia pedis. 9/4/03 Benzathine penicillin 1.2 million units intramuscularly every four weeks was added for strep coverage. Past Medical History, continued Last seen by Dr. Vogelman on 8/26/04 who stopped antibiotics due to complete clearing of cellulitis/erysipelas. Noted anemia (Hct 33) as well as a 2 month history of weight loss, fatigue, myalgias, and night sweats. Physical Exam Pulse: 112 bpm BP: 148/80 mmHg Temperature: 99°F Chest: Clear Heart: Harsh IV/VI systolic murmur along the left sternal margin, apex and base. Well healed scar, left leg Initial Lab and X-Rays Sed Rate: 115 Normal PA and Lateral Chest Film/Sinus Series Additional Lab and Imaging Studies Initial blood culture grew Strep viridans (within 18 hours) followed by two subsequent sets which also grew Strep viridans (6 of 6 bottles) Transthoracic echocardiogram—no vegetations. VSD and ASD noted. Transesophageal echocardiogram—sub-pulmonic pedunculated mass in the RV outflow tract. Located where flow across the VSD hits the outflow track. Pulmonic regurgitation. Hospital Course Admitted and started on intravenous penicillin. Gentamycin was added later. Infectious disease consult—Strep viridans probably due to dental work. MIC Ceftriaxone .064 s Penicillin .064-.125 s Discharged on Ceftriaxone 2 grams IV daily. “I never knew I could feel this good.” Learning Objectives Recognize the protean signs and symptoms associated with bacterial endocarditis Become familiar with the common microorganisms which cause acute and subacute bacterial endocarditis Become familiar with the Modified Duke Criteria for the diagnosis of infective endocarditis Review the current recommendations for the treatment of, and prophylaxis for infective endocarditis Definition Microbial infection of a cardiac valve or mural endocardium Mortality – – – – Almost 100% in preantibiotic era 10% streptococcal endocarditis 35% staphylococcal endocarditis 25-50% with prosthetic valve endocarditis 20,000-30,000 new cases/year primarily among newborn and elderly Causes of Prosthetic Valve Endocarditis Pathogenesis Blood is driven from a high pressure area through a cardiac defect into a low pressure sink. A platelet-fibrin aggregate forms in the low pressure sink. During bacteremia, avirulent/virulent organisms adhere to the platelet-fibrin aggregate forming a vegetation. Clinical presentations Subacute bacterial endocarditis – Duration of more than six weeks Symptoms may begin insidiously and last for months Fever, sweats, weakness, myalgias, arthralgias, malaise, anorexia, and fatigability are common Subacute bacterial endocarditis, continued May be caused by avirulent bacteria, such as streptococci which are part of the indigenous flora Cutaneous manifestations – Petechiae-conjunctivae, oropharynx, skin – Osler’s nodes—tender, purplish subcutaneous nodules in the pulp of the fingers – Janeway lesions-nodular, nonpainful erythematous or hemorrhagic areas on the palms or soles. Subacute bacterial endocarditis, continued Musculoskeletal features—myalgias, arthralgias, arthritis 40-50% Ocular findings—Roth spots—oval white areas surrounded by a zone of hemorrhage 3-5% Splenomegaly—15-30% with infarcts in 40% and abscesses in 5% of patients with SBE Subacute bacterial endocarditis, continued Renal manifestations – Hematuria in 50% – Embolic renal infarction—flank pain – Membranoproliferative glomerulonephritis Embolic phenomenon (cerebral or systemic) 25-50% Mycotic aneurysms 2-10% Subacute bacterial endocarditis, continued Neurological complications 30-40% due either to emboli or mycotic aneurysms Cardiac findings – Murmur present in 90% of patients – Heart failure-usually due to involvement of aortic or mitral valves – New conduction abnormalities due to involvement of the membranous septum in the area of the AV node Acute bacterial endocarditis Organisms are more invasive (s. aureus, s pneumoniae, gram negative bacilli) Onset is abrupt, with rigors and temperatures over 102° F (duration less than six weeks) Cutaneous manifestations, petechiae may be prominent, especially when caused by s. aureus Emboli are common Metastatic infections-cause organ-specific symptoms Echocardiography 60% of vegetations can be detected using transthoracic echocardiography 87-94% of vegetations can be detected with transesophageal echocardiography Transesophageal echocardiography is indicated as the initial method for difficult to image patients, possible prosthetic valve infections, in patients with intermediate to high clinical suspicion or in patients for a high risk of complications