CHAPTER 44 - Nursing Pharmacology FrontPage
advertisement

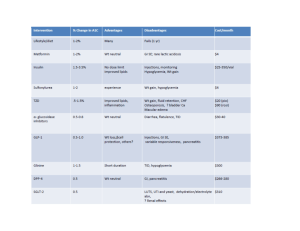
CHAPTER 44 DRUGS FOR DIABETES MELLITUS LEARNING OUTCOME 1 Describe the endocrine and exocrine functions of the pancreas. Concepts 1. The pancreas is both an endocrine and an exocrine gland. It is responsible for the secretion of several enzymes into the duodenum that assist in the chemical digestion of nutrients. This is its exocrine function. The islets of Langerhans are responsible for its endocrine function: the secretion of glucagon and insulin. 2. Insulin is released when the blood-glucose level increases, and glucagon is released when the blood–glucose level decreases. Hormones and drugs can affect blood sugar (hyperglycemic or hypoglycemic effects). (See Figure 44.1 for an illustration of alpha and beta cells. See Figure 44.2 for an illustration of glucose, insulin, and glucagon action in the body.) Figure 44.1 Glucagon and Insulin-secreting Cells in the Islets of Langerhans Figure 44.2 Insulin, Glucagon, and Blood Glucose LEARNING OUTCOME 2 Compare and contrast type 1 and type 2 diabetes mellitus. Concepts 1. Type 1 DM is caused by an absolute lack of insulin secretion due to autoimmune destruction of pancreatic islet cells. If untreated, DM produces long-term damage to arteries, which leads to heart disease, stroke, kidney disease, and blindness. 2. Type 2 DM is insulin resistance; target cells become unresponsive to insulin due to a defect in insulin receptor function caused by a lack of sensitivity of insulin receptors at the target cells (insulin resistance) and a deficiency in insulin secretion. If untreated, the same chronic conditions result as in type 1 DM. LEARNING OUTCOME 3 Compare and contrast types of insulin. Concepts 1. Type 1 DM is treated with dietary restrictions, exercise, and insulin therapy. The many types of insulin preparations vary as to their onset of action, time to peak effect, and duration. (See Table 44.1 for a list of types of insulin.) 2. Almost all insulin used today is human insulin made by recombinant DNA technology. It is more effective, causes fewer allergies, and creates less resistance. It is modified to be more rapid (Humalog) or have a prolonged action (Lantus). Insulin is administered by subcutaneous (SQ), inhaled (Exubera, approved in Adams_IRM Ch 44-1 2006), or intravenous routes. Only regular insulin can be given intravenously. (See Figure 44.3 for an illustration of an insulin pump.) Table 44.1 Insulin Preparations Figure 44.3 An Illustration of an Insulin Pump LEARNING OUTCOME 4 Describe the signs and symptoms of insulin overdose and underdose. Concepts 1. The most serious adverse effect from insulin therapy is hypoglycemia. Hypoglycemia can result from an overdose of insulin, improper timing of insulin dose, or skipping a meal. Signs and symptoms of hypoglycemia include tachycardia, confusion, sweating, drowsiness, convulsions, coma, and even death. 2. Hyperglycemia can result from an underdose of insulin or oral hypoglycemic. Signs and symptoms of hyperglycemia include fasting blood glucose greater than 126 mg/dL, polyuria, polydipsia, polyphagia, glucosuria, weight loss or gain, and fatigue. LEARNING OUTCOME 5 Describe the nurse’s role in the pharmacologic management of diabetes mellitus. Concepts 1. The role of the nurse in the pharmacologic management of diabetes mellitus involves careful monitoring of a client’s condition and providing education as it relates to the prescribed drug treatment. Obtain baseline medical, surgical, and drug history; lifestyle and dietary habits, including use of herbal or alternative therapies; and a detailed description of symptomology and current therapies. 2. Insulin therapy: Be familiar with the onset, peak, and duration of action of the insulin(s) prescribed, as well as any other important aspects of the specific insulin, and convey this information to the client. It is important to understand that not all types of insulin are compatible and may not be mixed together in a single syringe. Clear insulin must be drawn into the syringe first to reduce the possible contamination of the clear insulin by the insulin containing a suspension. Know the signs and symptoms of hypoglycemia and hyperglycemia. 3. Oral hypoglycemic therapy: Assessment of the client with type 2 diabetes includes a physical examination, health history, psychosocial history, and lifestyle history. Provide clients with information about the importance of keeping blood-glucose levels within a normal range. Blood-glucose levels should be monitored daily; urinary ketones should be monitored if the blood-glucose level is over 300 mg/dL. Also monitor intake and output, and review lab studies for liver-function abnormalities. Monitor the client for signs and symptoms of illness or infection. Administer oral hypoglycemics as directed by the prescriber. Ch 44-2 Adams_IRM LEARNING OUTCOME 6 Identify drug classes used to treat type 2 diabetes mellitus. Concepts Type 2 DM is controlled through lifestyle changes and oral hypoglycemic drugs. All oral hypoglycemics have the common action of lowering blood-glucose levels. Many have the potential to cause hypoglycemia. Oral hypoglycemics are not effective for type 1 DM. People with type 2 diabetes mellitus should have a preprandial blood sugar below 110 mg/dL. The six primary groups of oral antidiabetic drugs are classified by their chemical structures and their mechanisms of action. These include sulfonylureas, biguanides, meglitinides, thiazolidinediones (or glitazones), alpha-glucosidase inhibitors, and incretin therapies. (The oral hypoglycemics are shown in Table 44.2.) 1. Sulfonylureas: The first oral hypoglycemics available, sulfonylureas are divided into first- and secondgeneration categories. The sulfonylureas act by stimulating the release of insulin from pancreatic islet cells and by increasing the sensitivity of insulin receptors on target cells. The most common adverse effect of sulfonylureas is hypoglycemia, which is usually caused by taking too much medication or not eating enough food. 2. Biguanides: Metformin (Glucophage), the only drug in this class, acts by decreasing the hepatic production of glucose (gluconeogenesis) and reducing insulin resistance. It does not promote insulin release from the pancreas. Most side effects are minor and GI-related, such as anorexia, nausea, and diarrhea. A new extended-release formulations of metformin ((Fortamet, Glucophage XR, and Glumetza) approved in 2005, allow for once-daily dosing. 3. Alpha-glucosidase inhibitors: The alpha-glucosidase inhibitors such as acarbose (Precose) act by blocking enzymes in the small intestine that are responsible for breaking down complex carbohydrates into monosaccharides. Because carbohydrates must be in the monosaccharide form to be absorbed, digestion of glucose is delayed. These agents are usually well tolerated and have minimal side effects. The most common side effects are GI-related, such as abdominal cramping, diarrhea, and flatulence. 4. Thiazolidinediones: The thiazolidinediones, or glitazones, reduce blood glucose by decreasing insulin resistance and inhibiting hepatic gluconeogenesis. Optimal lowering of blood glucose may take 3 to 4 months of therapy. The most common adverse effects are fluid retention, headache, and weight gain. Hypoglycemia does not occur with drugs in this class. 5. Meglitinides: The meglitinides are a newer class of oral hypoglycemics that act by stimulating the release of insulin from pancreatic islet cells in a manner similar to that of the sulfonylureas. Both agents in this class have short durations of action of 2 to 4 hours. Their efficacy is equal to that of the sulfonylureas, and they are well tolerated. Hypoglycemia is the most common adverse effect. 6. Newer agents: These agents act by affecting the incretin–glucose control mechanism. Incretins are hormones secreted by the intestine following a meal when the blood-glucose level is elevated. Two new drugs with unique mechanisms entered the market in 2005. Exenatide (Byetta) is an injectable drug that belongs to a class of drugs called incretin mimetics. These drugs mimic the effects of incretins, which are hormones produced and released into the blood by the intestine in response to food. Sitaglipton inhibits DPP-4, thereby reducing the destruction of incretins. Levels of incretin hormones increase, thus decreasing blood-glucose levels in patients with type 2 diabetes. The drug is given once daily by the oral route. Pramlintide (Symlin) is a new injectable drug for type 1 and type 2 DM that resembles human amylin, a hormone produced by the pancreas after meals that helps the body to regulate blood glucose. In 2009, an old drug with a new use was approved to treat type 2 diabetes—bromocriptine (Parlodel) marketed as Cycloset, whose exact mechanism of action is still unclear. Adams_IRM Ch 44-3 Table 44.2 Oral Hypoglycemics LEARNING OUTCOME 7 For each of the drug classes listed in Drugs at a Glance, know representative drug examples, and explain the mechanisms of drug action, primary actions, and important adverse effects. Concepts 1. Insulins: Prototype drug: regular insulin. Mechanism of action: to promote the entry of glucose into cells. Primary use: This is a short-acting insulin, with an onset of 30 to 60 minutes, a peak effect at 2 to 3 hours, and a duration of 5 to 7 hours. It is used to quickly decrease blood glucose; also used in the emergency management of ketoacidosis. Adverse effects: hypoglycemia. 2. Oral hypoglycemics: Prototype drug: glipizide (Glucotrol, Glucotrol XL). Mechanism of action: to stimulate the pancreas to secrete more insulin. It also increases the sensitivity of insulin receptors at target tissues. Primary use: for treatment of type 2 diabetes. Adverse effects: hypoglycemia, rashes, and photosensitivity. Some clients experience mild, GI-related effects such as nausea, vomiting, or loss of appetite. Prototype Drug regular insulin glipizide (Glucotrol, Glucotrol XL) ANIMATIONS AND VIDEOS Mechanism in Action: glipizide (Glucotrol) LEARNING OUTCOME 8 Use the nursing process to care for patients receiving drug therapy for diabetes mellitus. Concepts 1. Clients receiving insulin therapy—Assessment: Obtain a complete health history, including allergies, drug history, and possible drug interactions. Obtain a history of current symptoms, duration and severity, and other related signs or symptoms (e.g., paresthesias of hands or feet). Assess feet and lower extremities for possible ulcerations. Obtain a dietary history including caloric intake if on an ADA diet, number of meals and snacks per day. Assess fluid intake and type of fluids consumed. Obtain baseline vital signs, height, and weight. Evaluate appropriate laboratory findings (e.g., CBC, electrolytes, glucose, A1C level, lipid profile, osmolality, hepatic and renal function studies). Assess subcutaneous areas for potential insulin injection sites. Assess client’s knowledge of insulin and ability to self-administer insulin. 2. Clients receiving insulin therapy—Nursing diagnoses: Imbalanced Nutrition, Less than Body Requirements (Type I diabetes, related to lack of insulin availability for normal metabolism); Imbalanced Nutrition, More Than Body Requirements (Type II diabetes, related to insulin resistance and intake more than body needs); Deficient Knowledge (drug therapy); Ineffective Therapeutic Regimen Management related to deficient knowledge or altered compliance with prescribed treatment Altered Compliance, Ch 44-4 Adams_IRM Noncompliance related to complexity of treatment plan, deficient knowledge; Risk for Deficient Fluid Volume related to polyuria from hyperglycemia; Risk for Injury related to adverse drug effects, lack of sensation in extremities from neuropathies; Risk for Infection related to hyperglycemia, impaired circulation to extremities, neuropathies. 3. Clients receiving insulin therapy—Planning: The client will experience therapeutic effects (e.g., blood sugar within normal limits). The client will be free from or experience minimal adverse effects. Verbalize an understanding of the drug’s use, adverse effects and required precautions. Demonstrate proper selfadministration of the medication (e.g., dose, timing, when to notify provider). 4. Clients receiving insulin therapy—Implementation: Administer insulin correctly and per schedule ordered (e.g., routine dosing with or without sliding-scale coverage), planning insulin administration and peak times around meal times. Ensure dietary needs are met based on need to lose, gain, or maintain current weight and glucose levels. Hold insulin dose if blood sugar is less than 70 mg/dL and report to the health care provider. Continue to monitor periodic lab work: CBC, electrolytes, glucose, A1C level, lipid profile, osmolality, hepatic and renal function studies. Assess for symptoms of hypoglycemia, especially around time of insulin peak activity. Monitor blood-glucose levels more frequently during periods of illness or stress. Encourage increased physical activity but monitor blood–glucose levels before and after exercise and begin any new or increased exercise routine gradually. Rotate insulin administration sites weekly. Change insulin pump subcutaneous catheters every 2 to 3 days to prevent infections at the site of insertion. Ensure proper storage of insulin to maintain maximum potency. Instruct patient and/or family in proper self-administration of drug. Check urine for ketones if blood glucose is over 300 mg/dL. 5. Clients receiving insulin therapy—Evaluation: The client will experience blood sugar within normal limits) and be free from or experience minimal adverse effects. Verbalizes an understanding of the drug’s use, adverse effects, and required precautions. Demonstrates proper self-administration of the medication (e.g., dose, timing, when to notify provider). 6. Clients receiving oral hypoglycemic therapy—Assessment: Obtain a complete health history including allergies, drug history, and possible drug interactions. Obtain a history of current symptoms, duration and severity, and other related signs or symptoms (e.g., paresthesias of hands or feet). Assess feet and lower extremities for possible ulcerations. Obtain a dietary history including caloric intake, number of meals and snacks per day. Assess fluid intake and type of fluids consumed. Obtain baseline vital signs, height, and weight. Evaluate appropriate laboratory findings (e.g., CBC, electrolytes, glucose, A1C level, lipid profile, hepatic and renal function studies). Assess for pain location and level. Assess client’s knowledge of drug. Assess client’s ability to conduct blood- glucose testing. Assess for and report promptly any adverse effects appropriate to type of oral agent signs of hypoglycemia and hyperglycemia. 7. Clients receiving oral hypoglycemic therapy—Nursing diagnoses: Imbalanced Nutrition, More than Body Requirements (Type II diabetes, related to insulin resistance and intake more than body needs); Deficient Knowledge (drug therapy); Ineffective Therapeutic Regimen Management related to deficient knowledge or altered compliance with prescribed treatment; Altered Compliance, Noncompliance related to complexity of treatment plan, deficient knowledge; Risk for Injury related to adverse drug effects, lack of sensation in extremities from neuropathies; Risk for Infection related to hyperglycemia, impaired circulation to extremities, neuropathies. 8. Clients receiving oral hypoglycemic therapy—Planning: The client will experience therapeutic effects (e.g., blood sugar within normal limits) and will be free from or experience minimal adverse effects. Verbalize an understanding of the drug’s use, adverse effects, and required precautions. Demonstrate proper self-administration of the medication (e.g., dose, timing, when to notify provider). 9. Clients receiving oral hypoglycemic therapy—Implementation: Ensure dietary needs are met based on Adams_IRM Ch 44-5 need to lose, gain, or maintain current weight and glucose levels. Consult with dietician as needed. Limit or eliminate alcohol use. Check with health care provider before giving oral hypoglycemic if blood sugar is less than 70 mg/dL and monitor periodic lab work: CBC, electrolytes, glucose, A1C level, lipid profile, hepatic and renal function studies. Assess for symptoms of hypoglycemia. If symptoms of hypoglycemia are noted, provide a quick- acting carbohydrate source (e.g., juice or other simple sugar), and then check capillary glucose level. Monitor blood-glucose levels more frequently during periods of illness or stress. Encourage increased activity but monitor blood-glucose levels before and after exercise and begin any new or increased exercise routine gradually. Monitor for signs of lactic acidosis if the client is receiving biguanide. Monitor for hypoglycemia up to 48 hours after exercise. Monitor for hypersensitivity and allergic reactions. Assess for pregnancy. Monitor for edema, BP, and lung sounds in patients taking thiazolidiones. Monitor for hypoglycemia more frequently in patients on concurrent beta-blocker therapy. Instruct patient and/or family in proper self-administration of drug. 10. Clients receiving oral hypoglycemic therapy—Evaluation: The client will experience therapeutic effects (e.g., blood sugar within normal limits) and will be free from or experience minimal adverse effects. Verbalize an understanding of the drug’s use, adverse effects, and required precautions. Demonstrates proper self-administration of the medication (e.g., dose, timing, when to notify provider). Ch 44-6 Adams_IRM