Diabetic Foot Referral Form
advertisement
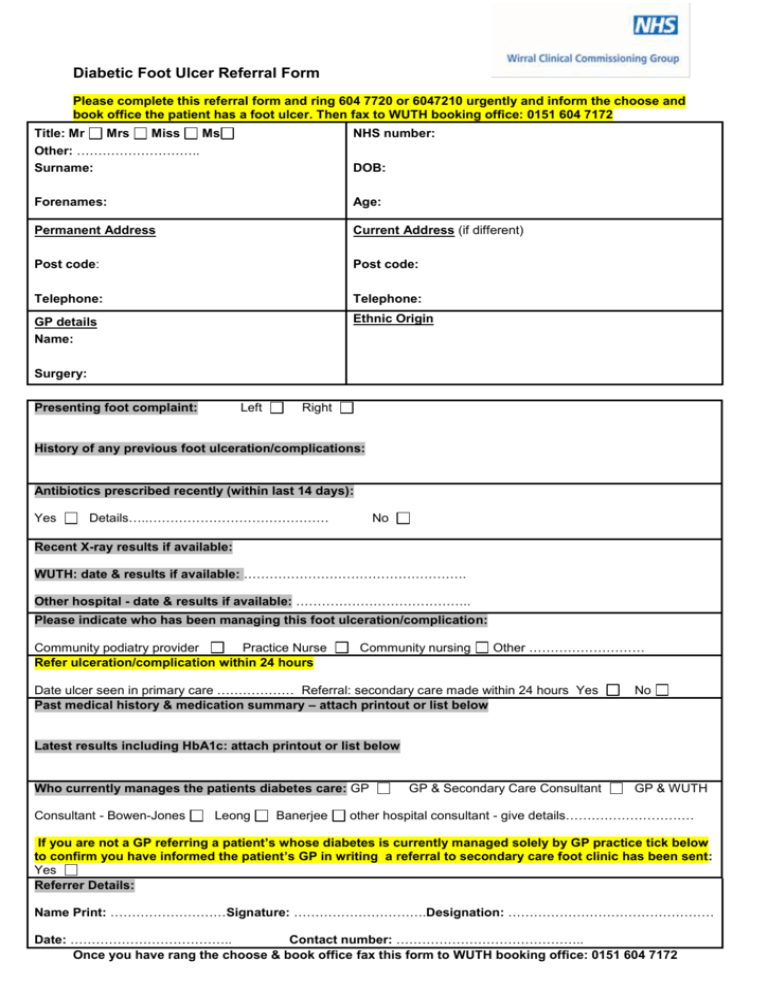
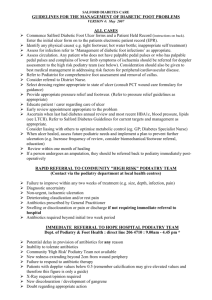
Diabetic Foot Ulcer Referral Form Please complete this referral form and ring 604 7720 or 6047210 urgently and inform the choose and book office the patient has a foot ulcer. Then fax to WUTH booking office: 0151 604 7172 Title: Mr Mrs Miss Ms Other: ……………………….. Surname: NHS number: Forenames: Age: Permanent Address Current Address (if different) Post code: Post code: Telephone: Telephone: GP details Name: Ethnic Origin DOB: Surgery: Presenting foot complaint: Left Right History of any previous foot ulceration/complications: Antibiotics prescribed recently (within last 14 days): Yes Details…..…………………………………… No Recent X-ray results if available: WUTH: date & results if available: ……………………………………………. Other hospital - date & results if available: ………………………………….. Please indicate who has been managing this foot ulceration/complication: Community podiatry provider Practice Nurse Refer ulceration/complication within 24 hours Community nursing Other ……………………… Date ulcer seen in primary care ……………… Referral: secondary care made within 24 hours Yes Past medical history & medication summary – attach printout or list below No Latest results including HbA1c: attach printout or list below Who currently manages the patients diabetes care: GP Consultant - Bowen-Jones Leong Banerjee GP & Secondary Care Consultant GP & WUTH other hospital consultant - give details………………………… If you are not a GP referring a patient’s whose diabetes is currently managed solely by GP practice tick below to confirm you have informed the patient’s GP in writing a referral to secondary care foot clinic has been sent: Yes Referrer Details: Name Print: ………………………Signature: ………………………….Designation: ………………………………………… Date: ……………………………….. Contact number: …………………………………….. Once you have rang the choose & book office fax this form to WUTH booking office: 0151 604 7172 Diabetic Foot Ulcer Referral Form Clinical Guideline Infected diabetic foot ulcers and osteomyelitis for out-patients For all patients: Inform the diabetes team looking after the patient. Check FBC, U&Es, LFTs, ESR, CRP and HbA1c prior to starting treatment. Arrange to check U&E’s, LFTs and CRP at least fortnightly until completion of treatment Obtain swabs for microscopy, culture and sensitivity from the floor of the affected ulcer after debridement. Review therapy when culture results become available NB. In general, superficial swabs from ulcers are not useful for determining if infection is present. Most will be positive due to colonisation of the ulcer and may not demonstrate a genuine infecting organism. For infected ulcers: First line: Oral co-amoxiclav* 625mg every 8 hours for a minimum of 2-4 weeks If PENICILLIN ALLERGY: Oral levofloxacin 500mg every 12 hours** (also see box 1) and oral metronidazole 400mg every 12 hours for a minimum of 2-4 weeks If Meticillin Resistant Staphylococcus aureus (MRSA) has been isolated from the site of infection at any time: Add oral doxycycline*** 100mg every 12 hours to either of the above regimens and Irrigate wound with Prontosan® Wound Irrigation Solution at each dressing change. (NB: the frequency of dressing change is dictated by the dressing type and will not always be daily. There is no need to take the dressing down just to irrigate the wound). For sloughy wounds, a gauze swab can be soaked with in Prontosan® Wound Irrigation Solution and placed on the wound for 10-15 minutes prior to dressing. Re-screen the wound for MRSA carriage 7 days after completion of treatment. Response should be reviewed in 72-96 hours and if ongoing concern discuss with Consultant Microbiologist. If osteomyelitis is suspected (non-healing chronic ulcer or deep ulcer where the bone can be probed): Use oral levofloxacin 500mg every 12 hours** (also see box 1) and oral clindamycin**** 300mg every 6 hours (if intolerant to 300mg of clindamycin, reduce dose to 150mg every 6 hours) for a minimum of 8 weeks. If the patient has swabs positive for MRSA, the microbiology laboratory should be contacted to determine clindamycin sensitivity. This is suitable only for patients who can be clinically treated as an outpatient. If large areas are involved or severe infection the patient should be given intravenous antibiotics – discuss with Consultant Microbiologist. Arrange X-rays of the affected area and if required MRI scan. If possible, try to obtain bone biopsies for microscopy, culture and sensitivity. Diabetic Foot Ulcer Referral Form Notes: * Cholestatic jaundice can occur either during or shortly after the use of co-amoxiclav (CSM warning). Patients should be counselled to stop co-amoxiclav and contact their GP immediately if they get any signs/symptoms of jaundice. ** Patients prescribed levofloxacin who have renal impairment will require dose reduction. If creatinine clearance (CrCl) is 20-50 ml/min use 500mg od; if CrCl 10-19ml/min use stat dose of 500mg followed by 250mg od; if CrCl <10ml/min or on renal replacement therapy use stat dose of 500mg followed by 125mg od. *** Photosensitivity is a known side effect of doxycycline – patients must avoid exposure of skin to direct sunlight or sun lamps. Patients should also be counselled to swallow doxycycline capsules whole with plenty of fluid during meals while sitting or standing **** If the patient develops diarrhoea (>48 hours) or has abdominal pain associated with the diarrhoea, ask the patient to contact the GP/Diabetic Nurse Specialist (DNS) and stop clindamycin. A stool sample should be submitted for Clostridium difficile toxin (CDT) testing and contact the microbiologists for advice on further antibiotic therapy. Box 1: Additional management of patients known to have previously had (at any time) or currently have MRSA colonisation who are prescribed levofloxacin: Ensure the patient is also prescribed daily Octenisan® skin washes (or equivalent) for the duration of the levofloxacin therapy. Please take into account previous microbiological results and if in doubt contact the Microbiologists (Dr John Cunniffe, Dr Kavya Mohandas and Dr Paul Shears) or the Microbiology Pharmacist (Christine Sluman). Microbiology Consultants: Microbiology Pharmacist: Microbiology results/enquiries: Ext 4429 or 4512 Ext 2877, Bleep 2459 Ext 4521 References: Watkins PJ. ABC of diabetes: The diabetic foot. British Medical Journal 2003;326:977-979 Dilemmas when managing cellulitis. Drug and Therapeutics Bulletin 2003; 41:43-46 Lew DP, Waldvogel FA. Osteomyelitis. The Lancet 2004;364:369-379 Managing foot ulcers in patients with diabetes. Drug and Therapeutics Bulletin 2002;40:12-14