Diabetic Foot Ulcers
advertisement
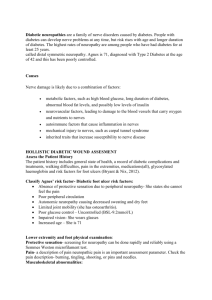
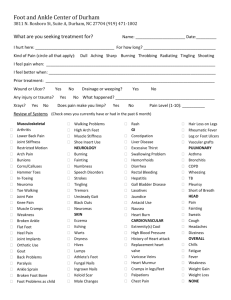
Diabetic Foot Ulcers Etiology Intrinsic factors 1. impaired blood supply 2. neuropathy 3. impaired defences against infection Extrinsic factors 1. trauma 2. Charcot joints 3. thick callous 4. previous foot ulcer 5. improper footwear, 6. unobtainable or low-quality podiatry service Secondary risk factors include 1. poor metabolic control 2. psychological factors 3. tobacco smoking 4. old age 5. low socioeconomic status. Neuropathy Diabetic neuropathy may be the most important Motor neuropathy leads to muscle atrophy, foot deformity (figure), altered biomechanics of walking, and redistribution of foot pressures during standing and walking Abundant callus formation on pressure points, together with thinning of the submetatarsal head fat-pads, additionally increases the force of plantar pressure and ultimately results in foot ulceration Autonomic neuropathy results in loss of sweating, which leaves the skin dry and vulnerable to cracks and fissures, and altered neurogenic regulation of cutaneous blood flow Sensory neuropathy can substantially impair the patient's perception of touch, deep pressure, temperature, and joint position. Leads to loss of protective sensations and altered foot mechanics during ambulation on uneven surfaces DPN affects the sensory neurons, with small-fiber sensory loss resulting initially in loss of pain, light touch, and temperature sensation, followed by loss of vibratory sensation as degeneration of the large myelinated fibers advances. Foot ulcers will develop in about 15% of patients with diabetes, and 25% of those will require amputation Vasculopathy 2-3-fold excess risk of accelerated atherosclerosis characteristically affects vessels between the knee and the ankle Trauma direct trauma, thermal injury mechanical stress that is repetitive (walking barefoot or in improper footwear) or continuously applied (extended unperceived pressure). Susceptibility increased with restricted joint mobility, poor foot care, and foot deformity resulting in bony prominences Classification neuropathic, ischaemic, or neuroischaemic International Working Group on the Diabetic Foot has proposed the PEDIS classification - grades the wound on the basis of five features: 1. perfusion (arterial supply) 2. extent (area) 3. depth 4. infection 5. sensation. Management 1. Perfusion a. reduce the risk of atherosclerotic vascular disease - smoking cessation, diet improvement, and medication prescription when needed to reach target concentrations of total and LDL cholesterol; b. establish the extent of any neuropathy c. establish presence of vascular disease, which includes i. palpating for foot pulses, ii. measuring the ankle-brachial pressure index (ABPI) and toe pressures, iii. colour-flow duplex ultrasonography iv. transcutaneous oxygen measurement, d. Magnetic resonance angiography (MRA) or conventional intra-arterial digital subtraction angiography if planning vascular reconstruction 2. Infection a. Most diabetic foot infections do not produce systemic manifestations, such as fever or leucocytosis, but when these signs are present, they typically suggest that any accompanying infection is severe b. most important pathogens causing diabetic foot infections are aerobic grampositive cocci (GPC), especially S aureus, but also β-haemolytic streptococci (especially group B) and coagulase-negative staphylococci. c. These GPCs often cause monomicrobial infections, but patients with chronic ulcers, or those who have recently received antibiotic treatment, often have a polymicrobial mix of aerobic gram-negative bacilli with GPCs d. old standard test for osteomyelitis is a bone biopsy sample processed for culture and histology 3. Wound dressings a. New treatments for diabetic foot ulcers continue to be introduced, yet few are subjected to controlled or comparative studies of their efficacy. b. Routine debridement of devitalised tissue at follow-up visits is widely recommended, but evidence showing that it accelerates healing is scarce c. Studies show that advancement of >0.7mm per week is 80% sensitive and specific for eventual wound closure d. Recent developments include the use of i. bone-marrow-derived stem cells ii. negative pressure dressings 1. randomized controlled trial (Armstrong, Lancet Nov 2005) shows a higher proportion of healed wounds, faster time to wound closure, a more rapid and robust granulation tissue response, and a potential trend towards reduced risk for a second amputation than control treatment. iii. bioengineered skin equivalents 1. Apligraf – 56% vs 38% wound closure at 12 weeks 2. Dermagraft – 30% vs 18% wound closure at 12 weeks iv. growth-factor therapy 1. PDGF-BB - 15% increased incidence of wound closure at 20 weejs v. Hyperbaric oxygen treatment seems to reduce the risk of major amputation, but not the time to ulcer healing or the rate of minor amputation. vi. Maggot (larval) biotherapy seems to be effective for debridement and acceleration of healing, and perhaps also in reducing antibiotic use and risk of amputation 4. Mechanical load relief a. should be counselled never to walk in the same shoes that could have contributed to a foot ulcer. b. Pressure relief on ulcers, commonly referred to as off-loading, should always be a part of the treatment plan. c. The most compelling evidence that off-loading accelerates ulcer healing comes from studies using a total contact cast for healing non-infected neuropathic ulcers. d. Neuropathic ulcers that have resisted healing for many months or years typically heal in about 6 weeks in a total contact cast. e. Pressure between the foot and ground at a plantar prominence can exceed 1000 kPa, whereas pressure between a correctly applied total contact cast and a potential ulcer site is less than 100 kPa f. Total contact casts are successful when properly applied and changed at least weekly, partly because patients cannot remove them easily. g. Crutches, bedrest, wheelchairs, and assistive ambulatory devices are probably not effective for off-loading without direct intervention at the foot, because of poor patient compliance. 5. Surgery a. Prevention i. Percutaneous lengthening of the Achilles tendon (ulcers due to limited ankle dorsiflexion) temporarily reduces pressure under the metatarsal heads, but carries an additional risk of secondary heel ulcers resulting from an altered gait. ii. Percutaneous tenotomy of the toe extensors reduces toe deformity and can hasten ulcer healing and prevent recurrence. iii. metatarsal osteotomy and resection of prominent metatarsal heads, either prophylactically or at the time of ulceration but this procedure poses a risk of secondary ulceration or other complications. b. Reconstruction Diabetic Foot Reconstruction Traditional views were pessimistic: Karp NS; Microvascular free-flap salvage of the diabetic foot: a 5-year experience. Plast Reconstr Surg. 1994 Nov 21 microvascular free flaps to the diabetic foot in 19 patients over a 65-month period. Twenty of the flaps survived. The operations required a long, costly hospitalization with frequent recipient- and donor-site complications. All patients eventually ambulated on their flaps. Five patients(20%) came to proximal amputation from 6 to 37 months after surgery. Only one amputation was for flap breakdown. Increasing literature on the reliability of flap coverage in diabetic foot ulcers Multistaged multidisciplinary approach In the presence of nonpalpable foot pulses – revascularisation, if possible performed first initial debridement where deep cultures taken and bone sent for pathologic evaluation serial debridement until wound clean Bone was debrided until normal bleeding bone was reached (Paprika sign). wounds observed until all signs of infection had resolved and soft-tissue regeneration was present Attinger C; Relative roles of aggressive wound care versus revascularization in salvage of the threatened lower extremity in the renal failure diabetic patient. Plast Reconstr Surg. 2002 Apr overall 43 percent complication rate. mean follow-up of over 3 years, 79 percent of wounds healed, 89 percent of all limbs were salvaged, and 49%of patients survived Blume, P, Attinger, C; Single-Stage Surgical Treatment of Noninfected Diabetic Foot Ulcers. PRS Feb 2002 single-stage approach consisted of total excision of the ulcer with broad exposure, correction of the underlying osseous deformity, and immediate primary closure using a local random flap selection – well perfused non infected diabetic foot Attinger, C; The Role of Intrinsic Muscle Flaps of the Foot for Bone Coverage in Foot and Ankle Defects in Diabetic and Nondiabetic Patients. PRS Sep 2002 Five different pedicled muscle flaps were used: o workhorse flap (abductor digiti minimi) is particularly useful for lateral ankle and calcaneal defects. o abductor hallucis flap is useful for medial midfoot, heel, and ankle defects. o flexor digitorum brevis flap is useful for plantar heel defects. o extensor digitorum brevis flap is useful for anterior ankle defects. 26% complication rate complete pedicled muscle flap failure rate 3% Ozkan O. Reliability of free-flap coverage in diabetic foot ulcers. Microsurgery. 2005 ultimate limb salvage rate was 83% should be considered a useful reconstructive option for serious defects in wellselected cases During the follow-up period of 8 months to 2 years, no ulcer recurrence was noted Rainer; Microsurgical management of the diabetic foot. J Reconstr Microsurg. 2003 Nov 10 microvascular free muscle flaps in nine patients over a mean follow-up period of 44 months. one flap loss, and nine flaps were transferred successfully. Seven of eight patients whose flaps survived had complications related to the free-flap recipient site. These seven patients underwent 20 secondary surgical procedures due to arterial and venous thrombosis, partial necrosis of the skin grafts, minor local infections, and gangrene or necrosis of the remaining toes. In three patients, progressive ischemic necrosis of the remaining toes, with total survival of the flap, was attributed to a microvascular steal phenomenon. However, all eight patients whose flaps survived subsequently ambulated on their flaps. Summary Well selected patients Adequate debridement Free flap success high Perioperative complications high Prolonged hospital stay Free flaps can be done successfully in diabetic patients and will lead to limb salvage and ambulation in the intermediate term