Case Sample: Nursing Home Abuse and Neglect Plaintiff is an 88
advertisement

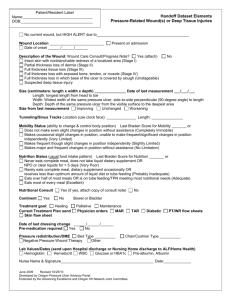
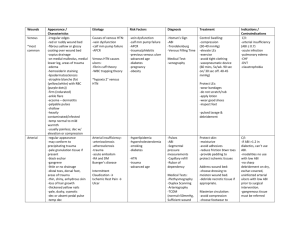
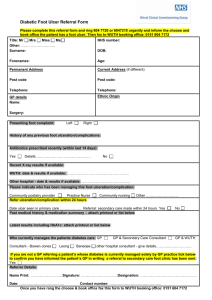
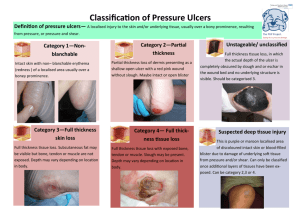
Case Sample: Nursing Home Abuse and Neglect Plaintiff is an 88-year old female and is a resident of various skilled nursing facilities from 2000 till date. She has got multiple medical conditions like diabetes, hypertension, dementia, arthritis, and osteomalacia and has had various surgeries in the past. She has been in and out of hospitals at regular intervals. Most of the information available related to the various bedsores and the care plan provided. Bedsores seem to have formed and healed at various points. Client advised to include information such as time period of stay at various hospitals and nursing homes, wound and ulcer care, bedsore assessments, nutrition, weight loss, contractures DATE PROVIDER 02/17/2000 FL Senior Living Services James Richard, M.D. Rose Mary, R.N. 02/16/2001 FL Senior Living Services James Richard, M.D. Rose Mary, R.N. Gladys Ross, R.N. 08/20/2002 FL Senior Living Services James Richard, M.D. OCCURRENCE/TREATMENT Admission Patient transferred via ambulance from Elder Care Facility and admitted. Prior to placement she had several falls at home and could no longer manage her care needs. BATES 836 882-887 992 Status Assessment Urinary Incontinence reported daily. Psychosocial wellbeing - Patient could establish own goals Nutritional Status Weight loss noted. Patient complained about the taste of many foods. Dietary supplement provided between meals. Pressure Ulcers Patient was in her room most of the times. Patient had Stage 2 decubitus ulcers to her left ankle and right buttock and her participation in scheduled programs had declined. Patient received room visits Care Plan Provision of bed rails Ulcer care Pressure relieving devices for chair and bed and heel pads. 16x18 high density Temper-Med foam recommended Turning/Repositioning patient every 2 hour Nutrition/hydration intervention to manage skin problem Pain management with medication Assessment of skin condition each shift Foot Care Nails/calluses trimmed. Protective foot care Diet Alert Weight increase of 6 lbs noted. Enjoyed sweets and family brought sweets, chocolate, ice cream. Family asked to avoid sweets and bring healthy snacks such as fruits. 112-117 119-136 1500 DATE 2005 PROVIDER FL Senior Living Services James Richard, M.D. Rose Mary, R.N. Gladys Ross, R.N. 09/23/2005 FL Senior Living Services James Richard, M.D. Rose Mary, R.N. Gladys Ross, R.N. 02/01/2007 FL Senior Living Services James Richard, M.D. 05/29/2007 Wound Care, LLC Paul Claude Montenegro, M.D. OCCURRENCE/TREATMENT Monthly Summary Leg pain Score - 6/10 05/29/2005 - Soft, low fat, low residual bland diet. 10/21/2005 – NCS increased protein diet. Pressure Sores On 05/29/2005 rashes noted to both breasts and abdominal folds On 09/23/2005 patient returned from hospital after surgical procedure for gallbladder removal. Patient had acquired Stage IV sacral ulcer. Patient repositioned every 2 hours within bed. Patient admitted to Skilled Nursing Facility after discharge from acute care hospital. Patient non-ambulatory. Total loss of voluntary movement to lower legs. Muscle weakness and rigidity. Had frequent bowel and bladder incontinence. Patient reported daily pain to the back and joints. Skin Evaluation Patient had Pressure Ulcer Stage IV to right side inner buttock. Skin rashes to right side abdomen and various surgical wounds. Skin at Risk Score - Severe Skin Treatment - pressure relieving devices for bed and chair, ulcer care, surgical wound care. Nursing staff are taking all necessary precautions however contractures are the cause of pressure and causing the ulcers Dietary Progress Notes Significant weight loss noted contra indicatory to wound healing. Poor glycemic control would impede wound healing. Ordered HbA1C. Patient did not meet protein needs for healing of Stage IV wound. Wound Consultation Patient seen for evaluation and management for multiple wounds on lower extremities, hip, sacrum, abdomen and elbow. She was a very debilitated. Blood sugars reported to be in good control. Patient deemed to be an unreliable historian and information was obtained from various records. Wound Examination Full thickness ulceration of the left and right trochanter (hip), sacrum. Periwound without erythema, crepitus, edema or induration. Moderate non-odorous serous drainage. Partial thickness ulceration of the abdomen. Foot wound Full thickness ulceration of left medial knee Right lateral foot - Stable eschar Left lateral malleolus - left foot, left 5th toe BATES 447-448 4 355-360, 949 1506 608-610 DATE PROVIDER OCCURRENCE/TREATMENT Deep tissue injury in left heel and left medial foot. Blood blister noted to right heel and right medial foot Treatment Full thickness wound of the bilateral hip - Stage IV Wound was inflammatory. Site cleaned with NSS or wound cleaner, medication applied and covered with gauze. Pressure ulcer of the sacrum - Stage IV Wound was proliferative. Cleaned with NSS, medication applied and covered with gauze. Full thickness ulcer of the left medial knee and right elbow Cleaned and dressed. Foot wounds: Complicated by vascular disease Ointment applied and dressed. General Care Plan Repositioning every 2 hours and off-load pressure on wound, float heels off mattress with pillow positioning, foam wedges. Monitoring of nutritional intake BATES