a case report illustrating the management of a complex neuropathic
advertisement

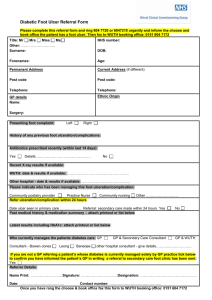
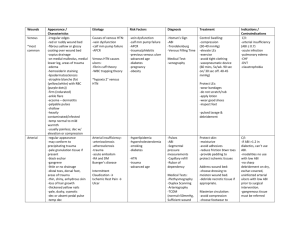
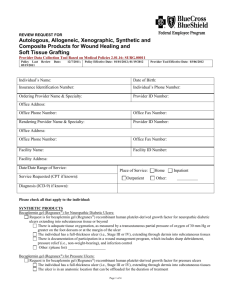
A CASE REPORT ILLUSTRATING THE MANAGEMENT OF A COMPLEX NEUROPATHIC FOOT ULCER Vowden K, D’Arcy A*, Vowden P. Dept. of Vascular Surgery and *Podiatry, Bradford Royal Infirmary, Bradford, UK. The foot without a protective response is always at risk of significant trauma or continuous low grade injury. When ulceration occurs in this situation management can be challenging and may require the use of a number of advanced wound care products used in conjunction with offloading, which in this case involved ambulatory pressure relief. Case study A 42 year old Asian male patient with a 37 year history of chronic foot ulceration secondary to a peripheral neuropathy initially thought, although not confirmed, to be due to leprosy was referred to the combined diabetic and vascular foot clinic in August 2000. The patient reported that he had previously had 24 attempts at skin grafting including amputation of the great toe with transfer of the skin to the ulcerated area on the sole of the foot. The last skin graft was performed in 1984 and following failure of these procedures he was offered below knee amputation but declined this radical form of treatment, preferring to continue with self-treatment, community and plastic surgical dressings and periodic courses of antibiotics. More recently he had required these three monthly. 1 On referral to the combined foot clinic, there were two plantar ulcers, one across the metatarsal heads with a further ulcer towards the heal (Figure 1). Despite intensive conventional management which included offloading with an Aircast® (Aircast Incorporated) boot, debridement and a variety of protective dressings these areas coalesced into a single ulcer measuring 23.6cm2 (Figure 2). Having concluded that this ulcer was unlikely to heal with either further dressings and offloading or another autologous skin graft we elected to treat the ulcer with a bioengineered skin product, Apligraf® (Organogenesis, Canton, MA and Novartis Pharmaceuticals, East Hanover, NJ). Following further wound bed preparation, which on this occasion including the use of Hyaluronic acid, Hyalofill® (ConvaTec Ltd) (Figure 3) we considered the ulcer ready for grafting. The Apligraf was airfreighted from the USA in environmentally stabilised packaging which provides a shelf-life of five days (Figure 4). We placed two of the 7.5cm diameter Apligrafs, fenestrated to allow drainage of exudate, onto the wound (Figure 5). The grafts were held in place by a combination of Mepital® (Mölnlycke), Lyofoam® (Seton) and orthopaedic wool covered with a retention crepe bandage. Initially the patient was managed as an outpatient with complete off-loading, returning to the Aircast® and limited mobilisation after four weeks. Results At the first major dressing change on day 5 there was already an improvement in the wound with evidence of an advancing healing edge (Figure 6). At 4 weeks (Figure 7) there had been a marked reduction in the ulcer size (>50%) and the remainder of the wound appeared healthy with a reduction in hyperkeratinosis and exudate. Rapid healing continued as shown by the images at 6 weeks (Figure 8), 7 weeks (Figure 9) 2 and 8 weeks (Figure 10). The ulcer has now healed (Figure 11) and other than one minor ulcer recurrence six month after healing the ulcer remains healed and the patient has returned to full mobility in custom made footwear. Discussion It would appear that the use of Apligraf has achieved what the patients own skin failed to do, namely the resolution of this chronic foot ulcer. Apligraf® (Organogenesis, Canton, MA and Novartis Pharmaceuticals, East Hanover, NJ) is a living human skin equivalents (HSEs) consisting of a tissue engineered bi-layered skin equivalent having both an epidermis and a dermis [1, 2]. It consists of keratinocytes and fibroblasts derived from neonatal foreskin and bovine collagen. Apligraf has been demonstrated to produces a great number of cytokines and growth factors and is immunologically well tolerated. Although the exact mode of action of HSE’s are not known they appear to act by both filling the wound defect with an extracellular matrix and by producing bio-active chemicals which enhance healing and which are produced by normal skin during the healing process. The value of this product in the management of diabetic neuropathic foot ulceration has recently been published [3-5]. It has been suggested that the neonatal origin of cells used in the production of Apligraf may provide the product with an advantage over other skin products and possibly even over autografts. Certainly in this case where management by conventional grafting techniques had failed repeatedly the healing of this ulcer following a single application of Apligraf has been remarkable. This case illustrates the importance of good wound bed preparation (WBP) before the application of either skin or biosynthetic skin substitutes if effective use of a scares or 3 expensive resources is to be used effectively. The aspects of good wound care as they relate to WBP have recently been discussed in an article published in this journal [6]. 4 References 1. Trent, J.F. and R.S. Kirsner, Tissue engineered skin: Apligraf, a bi-layered living skin equivalent. Int J Clin Pract, 1998. 52(6): p. 408-13. 2. Eaglstein, W.H. and V. Falanga, Tissue engineering and the development of Apligraf a human skin equivalent. Adv Wound Care, 1998. 11(4 Suppl): p. 18. 3. Pham, H.T., B.I. Rosenblum, T.E. Lyons, J.M. Giurini, J.S. Chrzan, G.M. Habershaw, and A. Veves, Evaluation of a human skin equivalent for the treatment of diabetic foot ulcers in a prospective, randomised, clinical trial. Wounds, 1999. 11(4): p. 79-86. 4. Brem, H., J. Balledux, T. Bloom, M.D. Kerstein, and L. Hollier, Healing of diabetic foot ulcers and pressure ulcers with human skin equivalent: a new paradigm in wound healing. Arch Surg, 2000. 135(6): p. 627-34. 5. Veves, A., V. Falanga, D.G. Armstrong, and M.L. Sabolinski, Graftskin, a human skin equivalent, is effective in the management of noninfected neuropathic diabetic foot ulcers: a prospective randomized multicenter clinical trial. Diabetes Care, 2001. 24(2): p. 290-5. 6. Vowden, P. and Vowden, K. (2002). Wound Bed Preparation (WBP). World Wide Wounds. Available: Internet Journal www.worldwidewounds.com, Version: Revision 1. Accessed on: April 2002. 5