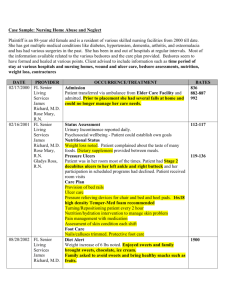
wound types
advertisement

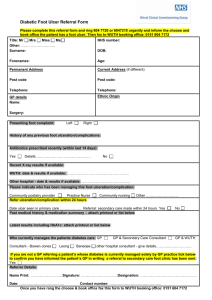
Wounds Venous *most common Arterial Appearance / Characteristics -irregular edges -red or ruddy wound bed -fibrous yellow or glossy coating over wound bed -copius drainage -on medial malleolus, medial lower leg, areas of trauma -edema -hemosiderin staining -lipodermatosclerosis -atrophie blanche (fat (yellow/white) with RBC (purple dots)) -firm (indurated) -ankle flare -eczema – dermatitis -palpable pulses -shallow -heavily contaminated/infected -temp normal to mild warmth -usually painless; dec w/ elevation or compression -regular appearance -may conform to precipitating trauma -pale granulation tissue if present -black eschar -gangrene -little or no drainage -distal toes, dorsal foot, areas of trauma -thin, shiny, anhydrous skin -loss of hair growth -thickened yellow nails -pale, dusky, cyanotic -dec or absent pedal pulse -temp dec Etiology Risk Factors Diagnosis Treatment Causes of venous HTN: -vein dysfunction -calf mm pump failure -APCR -vein dysfunction -calf mm pump failure -APCR -trauma/phlebitis -previous venous ulcer -advanced age -diabetes -pregnancy -obesity -Homan’s Sign -ABI -Trendelenburg -Venous Filling Time Control Swelling: -compression (30-40 mmHg) -elevate LEs -exercise -avoid tight clothing -vasopneumatic device (60 mins, 5x/wk. 90 sec on/ 30 sec off. 40-45 mmHg) Venous HTN causes ulcers: -fibrin cuff theory -WBC trapping theory Medical Test: -venography *hypoxia 2° venous HTN Indications / Contraindications C/I: -arterial insufficiency (ABI ≤ 0.7) -acute infection -pulmonary edema -CHF -DVT -claustrophobia Protect LEs: -wear bandages -do not scratch/rub -apply lotion -wear good shoes -inspect feet -pulsed lavage & debridement Arterial insufficiency: -arteriosclerosis -atherosclerosis -trauma -acute embolism -RA and DM Buerger’s disease Intermittent Claudication → Ischemic Rest Pain → Ulcer -hyperlipidemia -hypercholesterolemia -smoking -diabetes -HTN -trauma -advanced age -Pulses -ABI -Segmental pressure measurements -Capillary refill -Rubor of dependency Medical Tests: -Plethysmography -Duplex Scanning -Arteriography -TCOM (normal=50mmHg, Sufficient wound Protect skin: -moisturize -avoid adhesives -reduce friction btwn toes -provide padding to protect ischemic tissues Address wound bed: -choose dressing to moisten wound bed. -debride necrotic tissue if appropriate. Maximize circulation: -avoid compression -choose footwear to C/I: -if ABI >1.2 in diabetics, can’t use ABI. -modalities no use with low ABI -no sharp debridement on dry, eschar-covered, uninfected arterial ulcers with low ABI prior to surgical intervention. -gangrenous tissue must be referred -severe pain; inc w/ elevation -intermittent claudication healing in chronic ischemic ulcers ≥35mmHg, Unlikely to heal<30 accommodate for bandages & dec stress to wound. -AD to off-load -dependent leg position -aerobic exercise -flexibility (gastrocs) Pressure *2nd most common Stage 1: non-blanchable erythema, superficial but dermis affected, no open area Stage 2: partial thickness involving epidermis and/or portions of dermis, superficial ulcer, looks like abrasion or blister, normal surrounding skin Stage 3: full thickness involving epidermis and dermis, damage or necrosis of subcutaneous tissue, may extend down to but not through underlying fascia, a deep crater with or without undermining, ulcer bed may be fat, slough, necrosis, or granulation tissue Stage 4: full thickness with extensive destruction, tissue necrosis, or damage to muscle, bone, or support structures (tendon, joint capsule, etc), often tunneling or undermining, visible or palpable bone (ulcers with Soft tissue injury caused by unrelieved pressure over bony prominence and resulting in damage to underlying tissue Ischemia occurs when external pressure exceed capillary pressure (12-32 mmHg is enough to occlude capillaries) -limited mobility -PVD -hip fx -diabetic neuropathy -Angioplasty → Stent → Bypass → Amputation 1. Pressure reduction 2. Cleansing 3. Dressings 4. Debridement 5. Nutrition 6. Modalities 7. Surgical treatment Pressure, shear, moisture, friction Medical: Surgical V-Y advancement flap (bring muscle, dermis, epidermis, and vascularization along to cover affected area). Anytime wound reaches bone, need to have a flap. Underlying soft tissue is more susceptible to pressure than skin therefore deeper tissues are larger than the superficial Pressure relief: -active (air) or reactive (foam) mattresses -roho cushion (air) -jay cushion (gel) Isch-disch Sacrum most common, then heels visible bone have osteomyelitis) Unstageable: ulcer covered with eschar or slough and true base cannot be seen Diabetic Deep tissue injury: wound begins in subdermal tissue, initially purple/blue, leads to denuding of epidermis and eschar formation, epidermis not broken through and is covering necrotic tissue Neuropathic with intact circulation: beneath 1st and 2nd metatarsal heads, great toe, dorsal toes, plaque of callus, autolytic wound (skin break-down) Ischemic with (neuroischemic) or without neuropathy: occurs in same places (margins of foot and heel), absence of foot pulse, frequent sepsis, pink, painful, pulseless, cold foot, microangiopathy Critically ischemic with neuropathy: ABI <.3 Grades: 0 = intact skin 1 = superficial 2 = deep 3 = deep & infected 4 = partial foot gangrene 5 = full foot gangrene Neuropathic: Painless trauma, excessive planar pressures during walking, mechanical pressure or shear stress, foot deformities (hammer toes), charcot foot, env around foot (tight shoes) Increased prevalence of medial calcific stenosis (calcification of tunica media and basement membrane) Microvascular disease Sustained hyperglycemia (decreases all 3 phases of wound healing, dec collagen synthesis, angiogenesis, fibroblast proliferation, reduce tensile strength of wounds, impairs ability to fight infection) Nylon filaments at 10-g bending forceif unable to perceive, loss of protective sensation and inc risk of ulceration -debridement -wound care -off-loading: DonJoy walking boot (cam walker) Reduce WB stresses (plantar ulcers) -crutches or walker (PWB) -gait training (dec step length to reduce forefoot pressure) -walking casts (dec pressure, dec edema, protect from re-injury) Total contact cast: minimize risk of secondary infection Stretch Achilles tendon or heel cord release C/I for walking cast: infected ulcers (Caution: mod-severe edema, fragile atrophic skin, deep ulceration) C/I for total contact cast: grades 3-5, fluctuating edema, active infection, ABI <0.45