Buckinghamshire Sexual Health Network
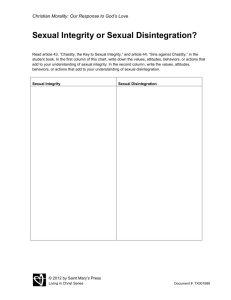
advertisement

NHS BUCKINGHAMSHIRE SEXUAL HEALTH & HIV STRATEGY 2009-2014 (REVIEWED AND UPDATED SEPTEMBER 2011) 1 2 Foreword Good sexual health is a vital aspect of health and well being and it is important that people have the right information, confidence and the means to make the right choices for themselves. Promoting sexual health is about enabling people to develop safe and positive relationships. NHS Buckinghamshire has published this 2009 – 2014 strategy to improve the health of the local population and reduce inequalities. This will be done by commissioning integrated sexual health services of a high quality that meet the sexual health needs of the local population and are equitable, cost effective and engage relevant community groups in their development. Over the last two years, a huge amount of work has gone in to implementing a sexual health programme of work in Buckinghamshire and some of the key achievements are highlighted below: providing additional access to contraceptive services in further and higher education settings setting up a long acting reversible contraception (LARC) training programme for general practitioners to improve access to contraception recommissioning of a termination service including early medical abortion commissioning a new sexual assault referral centre with other NHS organisations across the Thames Valley issuing a tender for a new level two integrated (STI screening and contraception) sexual health service development of a local sexual health website – www.sexualhealthbucks.nhs.uk roll out of the county wide emergency hormonal contraception scheme in community pharmacy improving access to condoms in non statutory youth and community settings achieving prompt access to local genitourinary (GUM) services within 48 hours. It is key, in light of future NHS changes, we continue to work across the NHS, local authorities and with third sector organisations to improve sexual health and make a positive difference to the lives of people in Buckinghamshire. Dr Jane O’Grady Director of Public Health NHS Buckinghamshire 3 Acknowledgements The development of this strategy would not have been possible without the valuable contribution made by all stakeholders in the local sexual health economy, especially those linked into the local Sexual Health Network in particular, Janette Harper, Commissioning Portfolio Lead, Angie Blackmore, Public Health Principal and Jenny Kent, Public Health Practitioner at NHS Buckinghamshire. 4 Contents Foreword ............................................................................................................... 3 Acknowledgements ................................................................................................ 4 Contents ................................................................................................................ 5 Executive Summary ................................................................................................ 6 Glossary ................................................................................................................. 9 Purpose of the Strategy ........................................................................................ 10 Strategic Vision .................................................................................................... 11 Setting the Scene.................................................................................................. 12 Buckinghamshire Sexual Health Network ............................................................. 14 National Sexual Health Policy Targets and Indicators ............................................ 14 Buckinghamshire’s Current Performance Against Key Targets ............................... 15 Sexual Health Profile ............................................................................................ 15 Local Sexual Health Services (2009) .............................................................................. 17 GUM & Sexual Health Services ..................................................................................... 18 Contraceptive Services................................................................................................. 20 Community Pharmacies ............................................................................................... 22 Chlamydia Screening Programme ................................................................................. 23 HIV Services ................................................................................................................ 24 Termination of Pregnancy Services............................................................................... 26 Vasectomy and Sterilisation ......................................................................................... 27 Psychosexual Services and Erectile Dysfunction ............................................................ 28 Sexual Assault & Exploitation ....................................................................................... 29 Sexual Health Promotion ............................................................................................. 30 Patient and Public Engagement ............................................................................ 32 Sexual Health Strategic Aims and Priorities........................................................... 33 Local Health Inequalities .............................................................................................. 33 Strategic Aims ............................................................................................................. 33 Priorities ..................................................................................................................... 34 References & Bibliography ................................................................................... 38 Appendices .......................................................................................................... 39 Appendix 1: Terms of Reference for the Sexual Health Network ................................... 39 Appendix 2: Levels of Sexual Health Service Provision .................................................. 40 Appendix 3: Sexual Health Guidance Documents .......................................................... 42 5 Executive Summary The continued rise of levels of sexually transmitted diseases, terminations and unplanned pregnancy both nationally and locally demonstrate that there is a need for a continued drive to address risky sexual health behaviours through education and access to services. As the number of people living with HIV, and living longer with HIV, continues to grow, the demand for flexible services to meet the needs of people living with this long term condition also rises. Since the publication of The National Strategy for Sexual Health and HIV in 2001 there has been an increased drive and focus on addressing sexual ill health, especially in the prevention of sexual ill health and unplanned pregnancy. Addressing sexual ill health has been shown to be cost effective, both in terms of the prevention of onward transmission and timely treatment of illness to prevent further co morbidities, and in terms of patient outcomes related to quality and control of their life. The key challenges within sexual health locally continue to be: Reducing rates of sexually transmitted infections (STIs), especially chlamydia in young people under 25 Reducing late diagnosis and undiagnosed sexually transmitted infections including HIV, especially in high risk groups Improving access to contraception to reduce unintended pregnancies Reducing the under 18 teenage conceptions leading to an abortion The objectives of the previous sexual health strategy for Buckinghamshire1 continue into this strategy and include: 1 To raise public awareness of sexual health services and the importance of positive sexual and emotional relationships, and risks of unsafe sex. To increase access to sexual health information, treatment, support and advice, especially to young people and other high risk groups. To provide skills and build capacity in individuals and communities, especially young people, to enable them to take greater control over their sexual health by gaining key relationship skills such as: - Negotiating for safer sex - Better communication - Assertiveness, being able to say ‘no’ to sex - Enhancing self-esteem in individuals, groups and communities so that they are able to make informed decisions about their sexual health. Mid-South Buckinghamshire Sexual Health & HIV Prevention Strategy 2006-2009 6 Progress has been made in many of the areas covered in the previous strategy, including: Introduction of level 2 community sexual health services to increase access to STI testing & treatment Increase in the provision of Emergency Hormonal Contraception (EHC, also known as “the morning after pill”) via community pharmacy Introduction of a Chlamydia Screening Programme locally Introduction of a condom distribution scheme for young people Piloting of You’re Welcome standards for developing young people accessible services. The higher rate of under 18 conceptions leading to a termination and late diagnosis of HIV, suggest that more work is still needed to increase awareness, access and education around all aspects of sexual health. The previous strategy was young people focused, whilst this strategy has been developed to consider the needs of all communities within the local population. The strategy has been developed based on national strategies, a refreshed local sexual health needs assessment and local priorities. A multi-disciplinary approach has ensured that all stakeholders have been able to contribute to this strategy, and will continue to be the approach taken to develop local pathways based on national evidence and designed to address local health inequalities. Since the development of this strategy, progress has been made in a number of areas including: The achievement of the GUM 48-hour offered target (offering an appointment within 48 hours of client’s first contact) for the first time in Buckinghamshire Commissioning a pilot service offering contraception alongside the level 2 outreach sexual health clinics The commissioning of a young people’s drop in service in the south of the county The refocusing of the Chlamydia Screening Programme to embed chlamydia screening into core services The retendering of termination services to increase the value achieved from this service and increase local access Commissioning a new sexual assault referral centre (SOLACE) Development of a local specialist training programme (LARC) Development of local primary care training programmes around sexual health Development of a standardised service specification across providers of GUM services Review of specialist contraception services to look at options for future service development Introduction of Chlamydia Screening via local community pharmacies Development of a local sexual health website 7 Work has also begun in the following areas: Joint review of HIV services with the council Review of level 2 sexual health services post the contraception pilot This strategy aims to provide a focus for all local providers and stakeholders to use to work towards quality, integrated, holistic sexual health services that are patient focused and meet the needs of all those living within Buckinghamshire. 8 Glossary AIDS ASG BASHH BCC bpas CaSH CSW C-Card CSP DH EHC EMA FPA FRSH GMS GP GUM HIV HPV ISVA LARC LINk LGBT MedFASH MSM NICE PCT PMS SARC SHA SHAW STI ToP TVPS Acquired Immune Deficiency Syndrome AIDS Support Grant British Association for Sexual Health and HIV Buckinghamshire County Council British Pregnancy Advisory Service Contraceptive and Sexual Health Service Commercial Sex Workers Condom Distribution Scheme Chlamydia Screening Programme Department of Health Emergency Hormonal Contraception (also known as the “morning after pill”) Early Medical Abortion Family Planning Association Faculty of Reproductive and Sexual Health General Medical Service contract (for provision of primary care services) General Practice/ General Practitioner Genito-Urinary Medicine (Specialist clinics for the treatment of STIs) Human Immunodeficiency Virus Human Papilloma Virus Independent Sexual Violence Advisor Long Acting Reversible Contraception (e.g. coils and implants) Local area Involvement Network Lesbian, Gay, Bisexual and Transexual people Medical Foundation for AIDS & Sexual Health Men Who Have Sex With Men National Institute for Health and Clinical Excellence Primary Care Trust Primary Medical Services contract (for provision of primary care services) Sexual Assault Referral Centre Strategic Health Authority Sexual Health At Wycombe (GUM clinic) Sexually Transmitted Infection Termination of Pregnancy Thames Valley Positive Support 9 Purpose of the Strategy Sexual ill health costs the NHS more than £700 million a year (HPA, 2004). For individuals this ranges from brief discomfort to pelvic inflammatory disease, infertility, and in some cases, death as a result of HIV / AIDS. Sexual health is a state of physical, emotional, mental, and social well being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence. (WHO, 2002) The purpose of this strategy is to bring together all services within the sexual health economy and align them strategically to produce integrated holistic sexual health services for the population of Buckinghamshire. The strategy will outline NHS Buckinghamshire’s strategic vision for services and look at the progress of sexual health services since 2009. It specifically looks at sexual health service provision and promotion, linking with other local and national strategies where appropriate2. Other areas, such as the HPV vaccine programme, the various cancer screening programmes, fertility, and gynaecological issues, whilst linked to the area, are out of scope for this strategy and are therefore not covered here. This strategy has been developed in consultation with all stakeholders within the sexual health economy of Buckinghamshire to ensure it is a comprehensive strategy that all parties can engage in to deliver the strategic vision for sexual health services within Buckinghamshire. Buckinghamshire Sexual Health Network will use this strategy to guide the development of services locally across the local health and social care economy. 2 E.g. the local Teenage Pregnancy Strategy 2009-2011 (Bucks County Council) and Alcohol Harm Reduction Strategy (2004, Prime Minister’s Strategy Unit). See References and Bibliography section for details. 10 Strategic Vision The strategic vision for sexual health services across Buckinghamshire was developed with key stakeholders in the sexual health economy of Buckinghamshire at a Visioning Event held with the support of the DH National Support Team for Sexual Health. This vision represents an ideal statement that stakeholders should work towards and will be the focus for developments in sexual health services across Buckinghamshire. The Vision for Sexual Health Services in Buckinghamshire: To provide holistic, confidential, integrated sexual health services that work through local partnerships, and that act as a centre of excellence for quality, training and clinical governance issues; To have pathways that provide equitable access to the full range of sexual health services [including abortion] through a central hub and are supported by prevention, outreach and signposting; That services are delivered by the most appropriately trained staff to meet the needs of our local population and in particular those identified as most vulnerable – as informed by local evidence and user involvement; And that sexual health services are transparently commissioned, well marketed and cost-effective. 11 Setting the Scene NHS Buckinghamshire has set itself four strategic objectives that underpin the commissioning plans and direction for the organisation. These are: 1) Improve the health status of our local population and reduce inequalities in health 2) Enhance quality and safety of patient services that we commission 3) Enable local people to have a greater influence on services that NHS Buckinghamshire commissions and increase the ability of people to manage their own care 4) Achieve financial sustainability with headroom to invest These are reflected in the core values and guiding principles that support the development of this strategy and its implementation: Equality – especially for vulnerable groups who are more likely to experience poor sexual health, targeting services where needed to ensure equitable access to sexual health services and reduce sexual health inequalities. Collaborative Working – partnership working with key stakeholders is vital to ensure that services are integrated and target where they are needed most, without duplication and with clear pathways between services. User Involvement – information from consultations, service user feedback and the development of a range of different ways to enable public and user involvement in service development to ensure that services meet local needs. Choice – to support the public to engage in their own sexual health and wellbeing access to services and information must be available through a range of different media and settings across the county. Quality – all services and information need to meet with national standards (including standards around respect and confidentiality), and be evidence based to ensure that services meet the needs of the local population and maximise the use of available resources appropriately. 12 The National Strategy for Sexual Health and HIV (2001) provides the strategic direction for improving sexual health in England. It includes five key aims which are reflected in local commissioning priorities: Reduce transmission of HIV and STI’s Reduce prevalence of undiagnosed HIV and STI’s Reduce unintended pregnancy rates Improve health and social care for people living with HIV Reduce stigma associated with HIV and STI’s. Overall, the direction of the National Strategy is working towards achieving: Better prevention Better services Better commissioning Much of the available guidance supports the need for all health services, including sexual health and HIV services, to engage in keeping people healthy (prevention of poor sexual health), rather than just treating illness. Levels of HIV and STIs continue to rise across the UK, with numbers of new diagnoses up 63% since 1998. The cost of providing sexual health services, including contraception and abortion services is now in excess of £0.25 billion each year nationally. Advances in treatment mean people with HIV are able to live healthier lives for longer, but this also increases the costs of treatment and care for HIV, which is now estimated to cost around £0.5 billion a year in the UK. In the National Sexual Health and HIV Strategy3, the DH also estimates that the socioeconomic costs of HIV are increasing by up to £3 billion each year. Research published by the fpa in 20054 indicated that the NHS in England could save almost £1 billion over 15 years by investing in contraception services and speeding up access to abortion by just ten days. The effective prevention of HIV and STIs and investment in contraception services is essential to reduce transmission and limit costs. NHS Buckinghamshire commissioned a refresh of the Sexual Health Needs Assessment for Buckinghamshire in 2009 to support the development of this strategy. This sexual health population profile has been refreshed in 2011 to provide an updated picture of the local population needs to ensure that services continue to develop to meet local needs. 3 The National Strategy for Sexual Health and HIV, DH, 2001 4 The Economics of Sexual Health, 2005, FPA 13 Buckinghamshire Sexual Health Network The Buckinghamshire Sexual Health Network5 has been established as a forum to bring together the key stakeholders in the local sexual health economy to address local needs and drive forward national and local agendas around sexual health6. The Buckinghamshire Sexual Health Network7: Aims to facilitate equitable, co-ordinated and integrated sexual health services for the local population Has responsibility for developing and reviewing the progress of projects in relation to the local sexual health priorities and plans Is chaired by Public Health, NHS Buckinghamshire and meets quarterly. Comprises of all local sexual health service providers, local community and voluntary sector organisations, and statutory services (such as local authority and health), with membership reviewed annually Invites other agencies and stakeholders to the group to ensure that links are developed and maintained with related areas/ specialities Establishes sub-groups from within the Network to work on key projects. National Sexual Health Policy Targets and Indicators Since the development of the National Strategy for Sexual Health (2001), and the review of the National Sexual Health Strategy by MedFASH8, there have been a number of national and regional targets and indicators developed to improve the performance of sexual health services. The table overleaf outlines Buckinghamshire’s performance against these targets for 2008-09, 2009-10 and 2010-11. With the current redesign of health and social care services under the coalition government, these indicators are currently under review and are likely to change from 2012-13. Once the new targets and indicators have been decided upon services will be assessed and developed where necessary to meet the new targets. 5 Previously called the Buckinghamshire a Sexual Health & HIV Strategy Group This is in line with recommendations in the national sexual health strategy to support providers to work together to deliver equitable, holistic care and focus on sexual health promotion to reduce STIs, HIV and unintended pregnancies. 7 Please see appendix for details of the Terms of Reference 8 Progress and Priorities – working together for high quality sexual health, 2008, MEDFASH 6 14 Buckinghamshire’s Current Performance Against Key Targets Bucks Performance9 National Targets 2008-09 2009-10 2010-11 Increase the proportion of patients offered a GUM appointment within 48 hours of them first contacting the service to 98%10 Increase the proportion of patients seen within GUM services within 48 hours to 85%. 17% under 15 to 24 year olds to be screened for Chlamydia in 2008/09 increasing to 25% and 35% in subsequent years. Total Offered 92.3% Total Offered 98.1% Total Offered 99.9% Total Seen 76.9% Total Seen Total Seen 83.9% 82% 15 to 24 year olds screened 8.3% 15 to 24 year olds screened 10.4% 15 to 24 year olds screened 10.3% Teenage pregnancy - reduce the under 18 conception rate by 50% by 2010. (Note that the local target is to reduce rates by 45% due to the lower than national average rates of teenage pregnancy in Bucks). Conception in under 18 year olds for 2007 = 236 (nos) Conception in under 18 year olds for 2008 = 240 (nos) Conception in under 18 year olds for 2009 = 234 (nos) Rate is 23.9 Data is always 16 months in arrears to per 1000 account for conceptions that go on to live female births. population aged 15-17 years old11 Rate is 24.4 per 1000 female population aged 15-17 years old Over 99% in local hospital maternity units Rate is 24.2 per 1000 female population aged 15-17 years old Over 99% in local hospital maternity units An increase in the proportion of pregnant women accepting an antenatal HIV test. Over 99% in local hospital maternity units Sexual Health Profile Sexual Health in Buckinghamshire: a review (2009) provides a refreshed sexual health needs assessment for Buckinghamshire, with the population information being further update by Sexual Health in Buckinghamshire PCT: Population Profile and Service Activity, 20111213, with details of the national and local picture of sexual health. 9 Data taken from Sexual Health Needs Assessment 2009, the Sexual Health Population Profile, 2011 and the latest available ONS and HPA data. 10 Note there is a 2% tolerance with this target 11 1998 baseline: 223 conceptions/Rate of 24.8 per 1000 female population aged 15-17 years 12 This can be found on the www.sexualhealthbucks.nhs.uk website. 15 Buckinghamshire Sexual Health Profile The number of people living with HIV in Buckinghamshire more than doubled (from 119 in 2002 to 338 in 2009) over the last 7 years of available data Although the numbers of new diagnoses of HIV are decreasing, up to 40% of all these cases are diagnosed late in the disease progression, meaning the risks of complications and the health burden are higher for these individuals Chlamydia remains the most commonly diagnosed STI New cases of gonorrhoea and syphilis are small, with cases of gonorrhoea decreasing from 2001 Buckinghamshire has a significantly lower teenage pregnancy rate for under 18s (24.2 per 1,000 females aged 15 – 17) compared to the England rate of 38.2 A higher percentage (61%) of under 18 conceptions end in termination compared to 51% and 50% in the South East and England respectively Termination and repeat termination rates in Bucks are in line with regional and national averages A number of sexual health inequalities exist across Buckinghamshire, including: - Lack of outreach services to engage with MSM (men who have sex with men) who are a high risk group for sexual ill health and discrimination - Lack of out-reach services to minority ethnic groups, especially around HIV infection - Young people locally feel under pressure to have sex, and almost a quarter report not knowing where to go for sexual health information and advice - No local sexual health promotion programmes in place for Commercial Sex Workers - Limited or no sexual health promotion programmes for vulnerable groups, including LGBT community, people with learning disabilities, substance mis-users and offenders. 13 Both documents where commissioned by Public Health and provided in conjunction with Solutions for Public Health. 16 Local Sexual Health Services (2009) The map below demonstrates the current arrangement of services (as of 2009) and areas of deprivation. This demonstrates the need to review access to services to ensure equitable access across Buckinghamshire and to ensure that services are targeted to the areas of need. Details of local services and plans to develop these are outlined below. Sexual Health Services and IMD 2007 score in NHS Buckinghamshire, 2009 17 GUM & Sexual Health Services In Buckinghamshire access to sexual health testing and treatment services is available from a range of providers: Specialist GUM level 314 services are provided in Aylesbury at the Brookside clinic and High Wycombe at the SHAW clinic. These clinics are now both provided by Buckinghamshire Healthcare NHS Trust15 Level 2 sexual health testing and treatment services are provided by The Practice and the Kestrel service at a variety of locations across the county Residents in the south of the county also often cross into East Berkshire to access GUM at The Garden Clinic, Slough which offer holistic walk-in clinics providing STI testing and contraception including LARC, and specialist clinics for LARC, HIV, and Sexual Dysfunction. In 2006 the Department of Health introduced a national target to improve access to GUM16 to reverse the recent trend of a rising spread of sexually transmitted diseases across the country: By March 2008, all patients who made contact with a GUM service to be offered an appointment within 48-hours of making initial contact Regionally a target of 85% of patients contacting GUM services being seen within 48 hours was introduced at the same time. Level 2 services where introduced in 2006 to support achievement of these targets locally by increasing capacity and providing community provision for sexual health testing and treatment. These are provided in a range of community settings across the county including GP surgeries, community hospitals, colleges & universities and drop-in centres. Both levels of service will be developed in line with DH Best Practice Guidance about reaching and maintaining the 48-hour access target17, with key priority given to: The improved use of resources to enable clinics to be run in the evenings, early mornings and at weekends Ensuring choice of access by offering a choice of both walk-in and appointment Promoting informed choice to balance the public health risks of delayed attendance with patient choice (through encouragement of patients to attend as soon as possible) Making use of outreach facilities to reduce barriers such as travelling time to attending services, especially in specific high risk communities The appropriate delivery of services across a sexual health network to ensure the needs of all sectors of the community are met. 14 Details of the different levels of service as defined by MedFASH & BASHH can be found in the appendices. 15 Since 2010/11. 16 National Support Team for Sexual Health, DH, (2006), 10 High Impact Changes for Genitourinary Medicine 48-Hour Access, London, DH 17 National Support Team for Sexual Health, DH, (2008), Genitourinary Medicine 48-hour Access: Getting to target and staying there, London, DH. 18 Key Service Issues & Priorities (as of 2009): - GUM & Level 2 Sexual Health Services To review service design to ensure that capacity is in place and efficiently utilised to enable sustaining of the 48-hour offered target (achieved for the first time in 09/10) Review the patient pathway for access to GUM/STI services to ensure there is clear alignment between providers to ensure patients are seen by the most appropriate service Develop outreach services to engage with vulnerable groups and support access to services across the county to meet the needs of the local population and address health inequalities Investigate the feasibility of developing out of hours clinics for GUM, including later evening clinics and weekend access within county Standardise service specifications across both GUM clinics to ensure equitable access to services To re-engage GUM with the prison health provider to ensure that services are available to this population To engage with patients and the local population to ensure that the GUM and STI services are patient focused Review services simultaneously with family planning/contraception service to ensure a coherent approach to contraception and sexual health services for all patients Investigate options for the provision of integrated sexual health and contraception services in line with national and local drivers To develop targeted services, clinics and campaigns (including outreach) to key high risk groups, such as Men who have Sex with Men (MSM) and Commercial Sex Workers (CSW). 19 Contraceptive Services18 Specialist Services The specialist contraceptive services in Buckinghamshire are provided by Buckinghamshire Healthcare NHS Trust since the merger of the PCT provider arm in 2010. The CASH service (Contraception and Sexual Health Service) provides clinics from the Brookside centre in Aylesbury, High Wycombe and a weekly clinic in Chalfont St Peter which include: Weekend and evening clinics All forms of contraception including LARC Dedicated young people’s clinics Appointment and walk-in services Emergency contraception including emergency coil fits Advice, guidance and treatment for complex cases. There is an urgent need to review the current service design and role of the CASH service to ensure that the service is robust and fit for purpose as a specialist level 3 provider of contraception across the county, including the provision of training for other non-specialist providers of contraception. The current clinic arrangement is based on historic set-up, which has at times resulted in huge pressures on the service and does not make best use of available resources, occasionally resulting in some temporary clinic closure. GP Services All of the Buckinghamshire GP practices provide basic contraceptive services under the current GMS and PMS contracts, which includes: Advice about the full range of contraceptive methods available Advice about sexual health promotion and STIs Testing for specific STIs in symptomatic patients and referrals as necessary for specialist sexual health services Prescribing of contraceptives Provision of LARC methods where specialist training has been undertaken in line with NICE guidance. There is concern that sexual health service provision within General Practice is variable and often dependent on the training and skills of GPs and Nurses within the practice. Approximately 75% of women go to their GP for contraception; therefore it is essential that NHS Buckinghamshire patients are able to access high quality equitable services across the whole county. There have also been issues accessing training to support LARC provision in General Practice. Brook Brook (young people’s sexual health charity) currently provides a weekly clinic on a Monday afternoon in Buckingham for those under 25 who wish to seek advice about all aspects of sexual health. They are able to provide condoms, emergency hormonal contraception and oral contraception for this group; with the only LARC method they are able to provide being contraceptive hormonal injections. This service is only 18 Previously known as Family Planning Service 20 available in the north of the county so does not promote equitable access across Buckinghamshire. With a higher number of teenage conceptions leading to a termination rate in Buckinghamshire and the very slow fall in teenage rates, it suggests that young people are not accessing effective contraception and may be engaging in more risky behaviour. In 2010 an outreach clinic was opened in Burnham to begin to address this issue. Access to Contraception Programme The DH has provided £26.8 million nationally over three years for local health services to ensure contraception is available in the right places at the right time. This included a focus on access to LARC methods (Long-Acting Reversible Contraception19), as NICE highlighted that if 7% of women switched from the contraceptive pill to LARC methods, the NHS could save around £100 million through reducing unintended pregnancies by 73,000 per annum. Key Service Issues & Priorities: Contraceptive Services There is a need to address access to contraception to ensure equity across the county and support patient choice. Services need to be reviewed to consider the need to address a patient’s sexual health and contraception needs holistically, including building links between services and looking to develop integrated services where possible. A programme of work to increase access to contraception in line with the DH programme needs to be developed and implemented. A pilot has been commissioned to provide contraception with the sexual health clinics in outreach settings. This will need to be reviewed and if successful additional resources made available to sustain this work. There is a need to engage with patients and the public to understand their needs and why there appears to be poor engagement in contraceptive services as demonstrated by the high termination rates. The CASH service needs to be redesigned to enable it to focus on providing a specialist level 3 contraception service. Local training programmes (especially around LARC) need to be established through the level 3 CASH provider to enable quality contraceptive and sexual health services to be provided through primary care (General Practice and Community Services). Need to look into young people’s outreach services to increase engagement of young people in sexual health and enable access to contraception. 19 particularly the Intra-Uterine Device (the coil), the Intra-Uterine System (the Mirena coil) and sub-dermal implants as long-acting contraceptive injections (Depo-Provera) are also LARC methods, but these are not included in the government drive to increase LARC uptake as their success depends on the patient attend 3 monthly for another injection, and so is more liable to failure through non-effective use. 21 Community Pharmacies Emergency Contraception Scheme Community Pharmacies within Buckinghamshire play a key part in promoting access to contraception for young people within Buckinghamshire. Currently 38 community pharmacies throughout Buckinghamshire participate in NHS Buckinghamshire’s Emergency Hormonal Contraception Scheme (EHC). This is a locally enhanced service which provides free EHC to young women aged under 19 years in the county. The service aims to make EHC more accessible to young women and contributes towards reducing Buckinghamshire’s teenage conception rate and increasing referrals to contraceptive services. Other possibilities There is potential to expand the Chlamydia Screening Programme to be offered at community pharmacies, especially whenever a patient accesses EHC, and this needs to be further investigated. Community pharmacies offer anonymous open access, which can be valuable in accessing young people and other vulnerable groups. Options to enhance the role of community pharmacies in sexual health promotion should be further explored via the new Healthy Living Pharmacy initiative. In July 2011 Chlamydia screening for all 15 – 24 year olds is being rolled out to pharmacies signed up to the EHC scheme. Testing and treatment is also available in three central pharmacies in High Wycombe, Aylesbury and Chesham from October 2010. This increases the choice in sites for treatment for young people and is based on their views captured during a series of focus groups in 2009. Key Service Issues & Priorities: Community Pharmacies Uptake of the EHC scheme should be monitored to identify areas of high usage for intervention. The scheme should also be promoted within the wider context of sexual health to ensure that young people are aware of its availability, but do not become reliant on the scheme as a method of contraception. Need to ensure that the issue of repeat users of the EHC scheme are encouraged to link in with sexual health services to promote safer behaviour and contraception. Further investigation is needed into the role of community pharmacies in the Chlamydia Screening Programme. There are opportunities to link CSP with the EHC scheme, as well as opportunities for opportunistic screening, treatment and promotion of the programme. Need to ensure that Community Pharmacies signpost patients of all ages to sexual health services to promote safe sex and access screening as appropriate. The role of community pharmacies in the promotion of the whole sexual health agenda should be reviewed and enhanced where possible. 22 Chlamydia Screening Programme The Chlamydia Screening Programme was introduced by the DH in 2003 in an attempt to reduce the dramatic rise in chlamydia in young people nationally, providing free testing and treatment if needed to all under 25. It has been commissioned in Buckinghamshire since 2007. The Chlamydia Screening Office (CSO) in Buckinghamshire is provided by Buckinghamshire Healthcare NHS Trust. The CSO provides: Training and support to sites participating in the Chlamydia Screening Programme Coordination and management of test results Treatment for those testing positive Partner notification Promotion and marketing of the programme through a range of media, including their own local website (http://morethanahug.com/). Chlamydia Screening is available through a number of sites, including non statutory services and postal kits via the website. Since 2007 there has been a year on year increase from the national target to screen 15% of the target population, to 35% in 2010-11, which NHS Buckinghamshire is yet to be able to achieve. In 2012/13 there will be national changes to the chlamydia indicator. The uptake of chlamydia screening through core services (general practice, community pharmacy, contraception, termination) has been poor across primary care. NHS Buckinghamshire is currently looking at a number of options to pilot in 2010-11 to establish their success at integrating chlamydia screening into general practice. National reports also question the value for money currently being achieved by this programme, which needs to be addressed at all levels (nationally as well as locally). Key Service Issues & Priorities: Chlamydia Screening Programme (CSP) There is a need to review current CSP and work with all providers to look at ways to increase uptake of the screening programme to meet the national targets Focus on building chlamydia screening into core services in line with national strategic direction, including implementing and reviewing a number of pilots around various areas of primary care, including general practice and community pharmacy Review the resources dedicated to CSP in light of the national target and local progress towards this Review current CSP initiatives to establish their success and decide whether to re-launch or decommission these initiatives Ensure good links with external partners/organisations, such as schools and colleges, to maximise on opportunities for chlamydia screening Investigate options for the provision of a sexual health GP clinical champion to support engagement in sexual health programmes including CSP. 23 HIV Services Health Outpatient care for people with HIV is provided by Buckinghamshire Healthcare NHS Trust at the SHAW and Brookside clinics. Patients are also able to access HIV outpatient care from out of area clinics, dependent on patient choice, an option taken up by a number of patients. Patients requiring in-patient care for illnesses secondary to their HIV, including those needing a blood transfusion, are provided for at High Wycombe General Hospital, although complex in-patient care is provided by the Infectious Diseases Unit in Oxford. Social Care Buckinghamshire County Council (BCC) provides HIV support via one full-time senior specialist social worker, who is currently supported by a part-time support worker. This is funded via the ASG (AIDS Support Grant), which is made to councils from the Department of Health as a contribution to the costs of social care for people living with HIV in each area. Voluntary Sector The ASG is also used to commission voluntary sector support provision for people affected and living with HIV. This is provided by The Crescent Support Group and TVPS (Thames Valley Positive Support). Following the removal of the ring-fencing of the ASG in 2010, BCC reviewed the funding made available to support people living with HIV and the contract with TVPS and the part-time support worker were ceased. Voluntary sector support provides: An outreach worker who links with the local GUM services Training for local social care services A drop-in centre in Aylesbury & High Wycombe Some outreach work to engage with high risk communities Support with social needs, such as housing, employment, immigration & benefits Peer support Health and wellbeing promotion. HPA Data from 2007 shows Buckinghamshire to have a prevalence rate of 0.8320, the 3rd lowest prevalence across South Central SHA. However, in 2007 46% of those newly diagnosed with HIV, were diagnosed late21. This was the second highest rate of late diagnosis across the SHA, and is well above the national average (31%). This suggests that stronger outreach programmes are needed to engage with relevant populations about their risk and how HIV can be managed, to encourage more people to come forward for testing. The use of technological developments, such as rapid testing, also needs to be considered to address the high rates of late diagnosis. HIV prevalence per 1,000 population aged 15 – 59 by local authority Late diagnosis is classed as having a CD4 cell count less than 200 cells per mm3 within 30 days of diagnosis, and is well beneath the CD4 cell count where medication should be initiated to prevent development of the disease and associated co-morbidities. 20 21 24 Key Service Issues & Priorities: HIV Services There is a need to understand why local HIV services may not be the services of choice when people choose to access services out of area, to enable local providers to develop services to meet local needs Following the removal of the ring-fence for the ASG and the planned changes to the health service, BCC and NHS Buckinghamshire need to work together to review current provision and plan a coordinated way forward to support people living with HIV The high late diagnosis rate in Buckinghamshire suggests the need for more pro-active engagement with high risk groups, as well as more awareness of the risks of acquiring HIV and the need for testing There is a need for a multi-agency review to ensure that the services available to support people living with HIV continue to meet their needs and are complimentary to each other, including supporting people’s primary care needs An HIV needs assessment and county wide review of all services that provide all levels of support and care to people living with HIV is recommended to support appropriate review of resource and investment. This review would also ensure that local services meet nationally recommended standards and are able to cope with the increasing number of people living with HIV in the county Clear referral pathways between all services need to be established and communicated Access to psychological support for children and adults affected and infected with HIV needs to be reviewed to ensure appropriate support is available Investment in resources and services will need to keep pace with the increasing numbers of HIV-infected persons requiring care, especially as people live longer with the illness. 25 Termination of Pregnancy Services Termination of pregnancy (ToP) services for unwanted pregnancies are provided by bpas (British Pregnancy Advisory Service)22 for all patients except those with significant co-morbidities23, and since 2010 have been commissioned in conjunction with NHS Milton Keynes and NHS Oxfordshire following a competitive tender process to ensure value for money is being achieved from the contract24. As part of this retender, Early Medical Services (EMA) have been developed within each PCT to increase local access to services to support patients to access ToP services under 10 weeks’ gestation. bpas offer a range of services from a number of venues across the country. Locally the following services are available: Consultation and Counselling is available in Aylesbury, High Wycombe, Milton Keynes and Oxford (from late 2010) Telephone Counselling is also available (from 2010) Procedures are available in London, Luton, Leamington Spa, and from 2010 High Wycombe, and Milton Keynes, with services being developed in Oxford – venue is dependent on the procedure being undertaken and patient choice 24 hour support and booking line Self referral is available Provision of contraception post procedure, including LARC methods Sign-posting to other services if patients decided to continue with the pregnancy Chlamydia Screening as part of the national programme. Key Service Issues & Priorities: Termination Services The termination of pregnancy service needs to be retendered during 09/10 to ensure that the desired quality, access to local services and value for money is achieved NHS Buckinghamshire will work with regional NHS providers of ToP services to ensure smooth pathways and patient choice are embedded and patients with complex co-morbidities are able to access ToP services rapidly where required Maximise the uptake of contraception post termination procedure to reduce the rate of repeat procedures The quality of all terminations needs to be closely monitored to ensure that services meet the needs of local patients, who may be reluctant to verbalise issues with the service due to the sensitive nature of it Ensure the uptake of chlamydia screening by people attending for terminations is maximised. 22 Termination of pregnancy services for medical reasons are completed at the local acute hospitals through the Obstetrics and Gynaecology services. 23 For patients with significant co-morbidities arrangements are in place with a number of NHS providers dependent on the patient’s needs, gestation and patient choice. bpas have a dedicated team to refer on these patients rapidly where required. 24 Termination of pregnancy services were previously jointly commissioned from bpas by NHS Milton Keynes and NHS Buckinghamshire for a number of years. 26 Vasectomy and Sterilisation Vasectomy services within Buckinghamshire are provided by two GP practices that have historically provided the service based on an enhanced service to their GMS contract. There is limited choice for patients, and there is often a long wait for a procedure (currently 4-6 months). There is a mix of approaches used across services, with the scapel-less technique the current best practice. Access to vasectomy services is via GP referral after full consideration of all other contraceptive methods and considerations for the risks and implications for the procedure. Female sterilisations are provided via gynaecological departments at general hospitals. These procedures are rare though, as with the availability and reliability of LARC methods, an invasive non-reversible procedure is rarely felt to be necessary. Reversal of both vasectomy and sterilisation are not funded on the NHS unless in extremely exceptional circumstances. Key Service Issues & Priorities: Vasectomy and Sterilisation Services Urgent work is needed to deal with the large waiting lists and ensuring that vasectomy is the most appropriate contraceptive procedure given the low success rates of reversal (which is not NHS funded) Vasectomy services need to be reviewed to ensure that the services provided meet best-practice standards around access and technique NHS Buckinghamshire needs to continue to ensure that all clinicians promote LARC methods over vasectomy and sterilisation methods, ensure that it is clear to the patient the low success rate of reversing the procedure and the lack of NHS funding available to undertake this. 27 Psychosexual Services and Erectile Dysfunction Relate provide psychosexual counselling services across Buckinghamshire to which patients can be referred or self-refer if they have identified that they would benefit from this type of support. There has been some concern about the appropriateness of some of the referrals received by the service, suggesting that there may need to be education about the function of psychosexual counselling. Relate charges people for each session they attend, based on their ability to pay. NHS Buckinghamshire provides a grant to the service to support those who are less able or not able to pay to ensure that they can still receive the service. There are no specific erectile dysfunction clinics available within Buckinghamshire. Currently patients requiring this service have to be referred out of area, although access to these clinics is not always easy for out of area patients as these clinics are often primary care based. A local GP has provided an erectile dysfunction clinic via pharmaceutical funding, but due to changes in the pharmaceutical funding rules this clinic has not been able to continue on a regular basis. Anecdotal evidence from local GPs is that referrals for patients with erectile dysfunction are made to urology due to a lack of a viable alternative, but the coding of urology appointments does not allow for the amount of activity this accounts for to be unpicked. Within secondary care there is dedicated erectile dysfunction support (specialist nurses) within the urology oncology department, but access to this resource is limited to patients within this speciality. Key Service Issues & Priorities: Psychosexual and Erectile Dysfunction Services Need to review provision of psychosexual counselling to ensure that local provision meets local needs A clear referral criteria and patient pathway needs to be established to ensure that all referrals to psychosexual and erectile dysfunction services are appropriate and that patients can access the most appropriate service for their needs Need to look into options for the provision of erectile dysfunction clinics in primary care reflecting national and local priorities and best practice. 28 Sexual Assault & Exploitation Sexual assault and exploitation are often hidden crimes, the effects of which can be devastating and have life-long health implications. Appropriate support enables the impact to be minimised and prevent further harm to both the individual and society. There is national work around sexual violence and exploitation, especially violence against women and girls. In response to government recommendations, Buckinghamshire County Council is undertaking work to co-ordinate the local response to sexual violence, and is looking to establish a sexual violence forum. Nationally, the government has the expectation that each police area will have at least one Sexual Assault Referral Centre (SARC) and that all victims will have access to an Independent Sexual Violence Advisor (ISVA) by 2010. SARCs provide a ‘one stop’ location where complainants of rape or sexual assault/abuse can receive: Appropriate medical care Emotional support and counselling Referral for follow-up by other agencies (e.g. GUM or ToP services) Support for historic as well as acute incidents Collation of forensic evidence for use at a later stage should the complainant not want to pursue criminal proceedings at the time. Buckinghamshire County Council support work around sexual violence and exploitation. A number of services are available locally to support people who have experienced or been affected by sexual abuse or exploitation25, including: Aylesbury & Wycombe Rape Crisis Victim Support Aylesbury & Wycombe Women’s Aid R-U-Safe? A Thames Valley wide SARC was opened in April 2011 with sites in Slough and Bletchley. Key Service Issues & Priorities: Sexual Abuse and Exploitation NHS Buckinghamshire will need to work with the Thames Valley wide project to implement a SARC locally, including ensuring that the necessary resources are available to support this. Clear links into and out of the SARC service must be in place once the SARC service is operational. There is a lack of support services available for male victims of sexual violence, therefore services should be looked to be developed to account for this. Clear care pathways and protocols must be established to support these patients who present reporting sexual violence, including the use of early evidence kits where appropriate. 25 There are also a number of national organisations that people can access including Stop it Now!, Lucy Faithfull Foundation, NSPCC, Survivors UK and Mankind UK. 29 Sexual Health Promotion Sexual Health Promotion is fundamental to achieving good sexual health for all people within Buckinghamshire. Through awareness of all the issues associated with sexual health and knowledge of where to access relevant services, the population of Buckinghamshire will be able to enjoy relationships that are safe, healthy, and consensual and free from discrimination, illness and disease. The Sexual Health Network have an annual communication plan to link in with national and coordinated local campaigns around specific aspects of sexual health. There are specific schemes to promote sexual health, run and delivered through various collaborations: C-Card – This scheme provides access to free condoms (and lubrication) from a range of non statutory settings, and is mainly26 aimed at young people under the age of 25. Sites are trained in demonstrating best practice use of condoms and how to discuss issues around sex and relationships with young people. The scheme is coordinated by Brookside Contraceptive and Sexual Health (CaSH) clinic, who also provide some of the Sex Matters training required to become a C-Card site. The scheme has been in place since November 2008 and currently has over 25 sites signed up to the scheme. It is intended that the number of sites will continue to increase and the opportunity to link with the CSP will be maximised. Sexual Health Bucks Website – During 2009 NHS Buckinghamshire launched the Sexual Health Bucks website to promote all local services and information around sexual health (www.sexualhealthbucks.nhs.uk). The website was developed from the Sexual Health Marketing sub-group of the Sexual Health Network, and will be reviewed and updated in 2011. Sex Matters Training – Sex Matters training is commissioned to support all professionals working with young people to be able to talk about sex and relationships, including sign-posting them to appropriate services for further advice or treatment, if needed, and at the higher level demonstrating and advising on condom use and pregnancy testing. Healthy Schools – Healthy Schools was a government initiative to promote a whole child/whole school approach to health, to reduce health inequalities, improve health and social inclusion and raise pupil achievement. Whilst this programme has been discontinued, the Sexual Health Network continue to link in with the schools service at BCC to support the health and wellbeing agenda, including the Health Zone programme commissioned by BCC. Healthy FE – Healthy FE (Further Education) is an extension of the principles of the Healthy Schools programme for the further education setting. This programme is a newer programme and therefore has only recently been initiated. Again, NHS Buckinghamshire and the local providers of sexual health services are working closely with partners in education and the local authority to support its implementation. 26 The C-Card scheme is also used to provide free condoms to those living with HIV via the voluntary sector services to help prevent onward transmission of the virus. 30 Key Service Issues & Priorities: Sexual Health Promotion C-Card scheme: there needs to be an increase in the number of sites registered with the scheme, and wider promotion of the scheme should be undertaken to ensure that it is being optimally used. Clear links with CSP should also be maximised. The website review needs to build on initial engagement with patients and the public to ensure that it remains a valuable local resource. Healthy Schools/FE: The Sexual Health Network will continue to look to support this work and increase the awareness and education around sexual health delivered via these avenues. Providers will be encouraged to link with this programme to help ensure the standards of sexual health education that is delivered. Outreach: There is a gap in targeted outreach to high risk groups. Work should be undertaken to identify resources to support this and the best model to achieve this across Buckinghamshire. 31 Patient and Public Engagement Patient and Public Engagement is key to developing services that fully meet the needs of the local population. This is especially so with sexual health services, where poorly designed services that do not meet local people’s needs can lead to poor engagement with services and then potentially to sexual ill health or unintended conception. Patient and Public Engagement work to date includes: Collection of patient feedback by all service providers, which is used to develop services to meet patient needs Focus groups held by the Public Health department within NHS Buckinghamshire to look at engagement in chlamydia screening Engagement with young people around the accessibility and usefulness of the sexual health website and incorporation of ideas for improvement into the final version Completion of a piece of work by a specialist registrar within the C&SH service looking at making sexual health services more young people friendly within Bucks, and the implementation of You’re Welcome standards Dedication of Sexual Health Network meeting to review how patient feedback is collected and used across the local sexual health economy, including guest speaker from Brook on how they engaged young men in local services. Since 2010 this work has developed further including: Public Consultation via patient groups, the LINk and Overview and Scrutiny Committee at BCC on the draft Sexual Health Strategy A piece of consultative work commissioned by Public Health to understand the views of local women on contraception Snapshot views of young people’s understanding of chlamydia captured via a local radio broadcast and vox pox with students in a Further Education setting Online anonymous engagement with the public to understand local views is currently being developed. The Sexual Health Network will continue to monitor the progress of patient and public engagement in sexual health services, and work to come up with innovative ways to engage with people from all backgrounds to ensure fair representation is made. 32 Sexual Health Strategic Aims and Priorities Local Health Inequalities The Sexual Health Needs Assessment and Sexual Health Population Profile update for 2011 continue to highlight the main groups who experience sexual health inequalities and are at high risk of sexual ill health: Young people, especially those in areas of deprivation within Buckinghamshire Lesbian, Gay, Bisexual and transgender (LGBT) community, especially men who have sex with men Commercial sex workers Minority ethnic groups. Other identified groups that are also more likely to experience sexual health inequalities include: Homeless people People with learning, physical and sensory disabilities Offenders People with drug and alcohol abuse issues People living with HIV Asylum seekers and recent migrants. Strategic Aims In order to ensure that NHS Buckinghamshire provides the best possible services for the local population the following issues need to be addressed: The current service provision across the county is not equitable and there are differences in the availability of access to services Reducing late diagnosis and undiagnosed sexually transmitted infections including HIV Improving access to contraceptive services to reduce unintended pregnancies Reduce the number of teenage conceptions leading to an abortion, as these are higher than the national average and suggest that both contraception and risky sexual behaviour needs to be addressed NHS Buckinghamshire needs to work with all providers to understand and address barriers preventing achievement of national and regional targets. It is widely acknowledged that whilst much work has been undertaken to improve the sexual health of the local population, mainly in recent years, much more is needed to really coordinate services and address the inequalities that exist within the county. All stakeholders are committed to continuing to work with NHS Buckinghamshire to develop services to meet the needs of the local population and achieve world class sexual health services for the people of Buckinghamshire. 33 Priorities Priorities for each year covered in this strategy, and the progress against these to date are outlined below. Year 1 Priorities (2009/10): A new sexual health strategy and comprehensive sexual health needs assessment has been produced, following engagement with all local stakeholders, to provide a strategic view and direction of travel for the development of local sexual health services and sexual health promotion across Buckinghamshire. GUM access has improved, with national targets for 48-hour access being achieved and maintained. Sexual Health Network redeveloped with refreshed membership, terms of reference and coordinated delivery plans across local stakeholders. Local termination of pregnancy services reviewed and retendered to achieve maximum value for money and enhance local provision, especially around contraception post procedure. Supported implementation of the Healthy Schools programme, with sexual health being a core part of this programme. Sexual health website launched, and marketing and communication plans developed support sexual health promotion, with appropriate new resource materials produced and disseminated. Focus groups held with young people to inform the commissioning of the local chlamydia screening programme Vasectomy services reviewed to address waiting list issues and ensure best practice techniques being used. Workforce reviewed in specialist services to resolve service delivery issues. Year 2 Priorities (2010/11): Updated the sexual health profile Issued a service specification for a new level two integrated sexual health service Integration and development of GUM services with service specifications reviewed and implemented across both clinics to standardise services. Review of HIV services provided under the ASG to ensure minimal reduction of service provision post ring-fence removal. Local provision of termination services developed and operational. 34 Thames Valley wide SARC commissioned and operational with sites in Slough and Bletchley. Specialist contraception service reviewed and agreement from the Overview and Scrutiny Committee to concentrate resources at Aylesbury and High Wycombe hubs. Training programmes developed and delivered to support primary care delivery of sexual health services, including specialist LARC training programmes. Programme of pilots and training in place to support DH Access to Contraception programme, including: - Outreach pilot including contraception as part of the level 2 clinics - Further Education and Higher Education mobile clinics extended to include contraception on a pilot basis - Brook service piloted in Burnham - Local GPs funded to train/re-train in LARC fitting. Audit of women’s views on contraception commissioned and delivered, capturing the views with nearly 800 women across a wide range of Buckinghamshire residents via online surveys, user questionnaire and focus groups. New clinical lead in place to develop contraception services and training across Buckinghamshire. Work programme developed to embed chlamydia screening into core services including: - Increasing uptake of CSP in contraception services - Developing CSP as part of the C-Card scheme - Employing a GP clinical champion to support the implementation of CSP in general practice - Developing local EHC schemes in community pharmacy to include CSP - Developing test and treatment pilots for CSP in 3 community pharmacies. - Taking part in a SHA wide social marketing project to increase Chlamydia screening with the over 21 age group Christmas campaign delivered via sixth forms, Further Education and Higher Education, youth and community settings and via public transport on safer sex and advertising the local website and postal test kits for Chlamydia. Year 3 (2011/12): All remaining services will be reviewed in light of the sexual health needs assessment and local strategy, and then re-designed/ re-commissioned to meets the demand and needs of the local population and/ or identify incongruence’s between capacity and demand. Development of High Wycombe specialist contraception hub with concentration of resources on High Wycombe and Aylesbury, and communication plans once detailed operation plans in place. 35 Review local access to erectile dysfunction services. Review access of young men to services across Buckinghamshire. Review and refresh sexual health website. Develop a joint strategic plan for HIV between NHS Buckinghamshire and Buckinghamshire County Council to ensure that future plans and service developments around HIV service provision are complimentary and best value for money is achieved. Year 4 onwards (2012 onwards): NHS Buckinghamshire will work in conjunction with Bucks County Council to develop appropriate action plans on sexual health in particular, targeting young people in line with the NHS changes and transfer of public health over to local authority Develop outreach services to engage high-risk groups. Review implications of health service structural changes to ensure sexual health services are not negatively impacted on by any changes and any opportunities to build on partnership working are identified. Look at feasibility of introducing a centralised booking service for all sexual health services to enable patients to easily access the most appropriate service for their needs. Expand engagement work to ensure that services truly reflect the local population, not just those who are most articulate. On-going review and development of services in line with national policy developments and available resources. Evaluate impact of projects undertaken in years 1 – 3 to establish success in improving the sexual health of the local population and to ensure the strategy remains fit for purpose. Ensuring all services have progressed to meet the national You’re Welcome standards to provide services that meet the needs of young people. To support all of the above priorities, NHS Buckinghamshire will look at the following: Workforce development issues Access Patient pathways Strategy and engagement work Developing robust contracts and performance monitoring with all providers Promoting partnership working across the local sexual health economy 36 NHS Buckinghamshire and the local Sexual Health Network will continue the progress made towards the achievement of good sexual health for all residents of Buckinghamshire. 37 References & Bibliography There have been a number of strategies and supporting guidance around many aspects of sexual health in recent years. These all shape the development of sexual health services nationally and locally. Appendix 3 lists a number of the wide variety of guidance and reports available to support the development of sexual health and HIV services. The key documents used in this strategy are: - - - The National Strategy for Sexual Health and HIV, DH, 2001 The National Strategy for Sexual Health and HIV. Implementation action plan, DH, 2002 Effective Commissioning of Sexual Health and HIV Services. A Sexual Health and HIV Commissioning Toolkit for Primary Care Trusts and Local Authorities, DH, 2003 Standards for the management of sexually transmitted infections (STIs), MedFASH & BASHH, 2010 Progress and priorities – working together for high quality sexual health. Review of the National Strategy for Sexual Health and HIV, MedFASH, 2008 Moving forward: Progress and priorities – working together for high-quality sexual health. Government response to the Independent Advisory Group’s review of the National Strategy for Sexual Health and HIV, DH, 2009 Sexual health – worth thinking about. A paper to inform national strategic planning for sexual health and HIV in 2011 and beyond, MedFASH, 2010 The Time is Now Achieving World Class Contraceptive and Abortion Services, Independent Advisory Group on Sexual Health and HIV, 2009 Clinical Guideline 30:Long Acting Reversible Contraception, NICE, 2005 The Time is Now Achieving World Class Contraceptive and Abortion Services, Independent Advisory Group on Sexual Health and HIV, 2009 Long Acting Reversible Contraception- Clinical Guideline, NICE, 2005 Framework for Better Living with HIV in England, Sigma Research, 2009 Recommended Standards for NHS HIV services, MedFASH, 2003 Standards for HIV Clinical Care, BHIVA, 2007 Buckinghamshire Joint Strategic Needs Assessment, http://www.buckinghamshire.nhs.uk/?page_id=667 Sexual Health in Buckinghamshire - a review, Supporting Public Health and NHS Buckinghamshire, 2009. Sexual Violence and Abuse Report for Buckinghamshire, 2009, Buckinghamshire County Council. Alcohol Harm Reductions Strategy, 2004, Prime Minister’s Strategy Unit Teenage Pregnancy Strategy 2009-11, Buckinghamshire County Council 38 Appendices Appendix 1: Terms of Reference for the Sexual Health Network Developing a strategic, collaborative and co-ordinated approach to the implementation of national sexual health and related strategies and programmes working across key sexual health provider services, county and district councils, NHS Trusts and the community and voluntary sector. Identifying local priorities across Buckinghamshire. Ensuring resources are targeted to those most at risk of poor sexual health. Developing a Buckinghamshire Sexual Health Strategy with associated delivery plans. Providing advice and a co-ordinated approach by working jointly with health commissioners. Acting as a key reference point to any local clinical networks and in an advisory capacity for implementation of NICE guidance and MEDFASH standards. Support the development of early intervention and health promotion opportunities within services. Act as the umbrella group for a number of task orientated subgroups (named below) and ad hoc core working groups as necessary. - Communications and Marketing Working Group - led by Public Health, NHS Buckinghamshire - Further Education Programme Working Group - led by Public Health, NHS Buckinghamshire - Local Chlamydia Steering Group - led by CASH Service, Buckinghamshire Healthcare NHS Trust To work in close liaison with the Buckinghamshire County Council HIV Steering Group and Teenage Pregnancy Reference Group. 39 Appendix 2: Levels of Sexual Health Service Provision The following lists comprise elements of STI management that are appropriate at various levels of service provision, as defined in the National Strategy for Sexual Health and HIV, (DH, 2001). There should be clear links between services providing the different levels of service, with services at each level providing the services outlined at the lower levels in addition to the level specific services. Level 1 Sexual history-taking and risk assessment - Including assessment of need for emergency contraception and HIV post-exposure prophylaxis following sexual exposure (PEPSE) Signposting to appropriate sexual health services Chlamydia screening - Opportunistic screening for genital chlamydia in asymptomatic males and females under the age of 25 STI screening for women and heterosexual men dependent on clinical presentation HIV testing - Including appropriate pre-test discussion and giving results Point of care HIV testing - Rapid result HIV testing using a validated test (with confirmation of positive results or referral for confirmation) Screening and vaccination for hepatitis B - Appropriate screening and vaccination for hepatitis B in at-risk groups Sexual health promotion - Provision of verbal and written sexual health promotion information Condom distribution Psychosexual problems - Assessment and referral for psychosexual problems Level 2 Incorporates Level 1 plus: STI testing and treatment of symptomatic but uncomplicated infections in men (except MSM)* and women excluding: - Men with dysuria and/or genital discharge** Symptoms at extra-genital sites, eg rectal or pharyngeal Pregnant women Genital ulceration other than uncomplicated genital herpes 40 Level 3 Incorporates Levels 1 and 2 plus: STI testing and treatment of MSM* STI testing and treatment of men with dysuria and genital discharge** Testing and treatment of STIs at extra-genital sites STIs with complications, with or without symptoms STIs in pregnant women Recurrent conditions - Recurrent or recalcitrant STIs and related conditions Management of syphilis and blood borne viruses - Including the management of syphilis at all stages of infection Tropical STIs Specialist HIV treatment and care Provision and follow up of HIV post exposure prophylaxis (PEP)*** both sexual and occupational STI service co-ordination across a network including: - Clinical leadership of STI management - Co-ordination of clinical governance - Co-ordination of STI training - Co-ordination of partner notification * The testing and management of men who have sex with men (MSM) has been defined as an element of care at Level 3 as the majority of infections in this group are in the rectum and/or pharynx rather than the urethra, with rapid access to microbiology being needed to undertake these tests. ** The appropriate management of men with dysuria and/or urethral discharge requires immediate microscopy, usually only available at specialist GUM (Level 3) services so the testing and treatment of such men has been defined as an element of care at Level 3. *** PEP ‘starter packs’ are often available in other settings such as Accident and Emergency or Occupational Health, but referral to a specialist GUM (Level 3) service is required for ongoing management and provision of antiretroviral drugs. 41 Appendix 3: Sexual Health Guidance Documents National Guidance for Sexual Health Services Commissioning: Choosing Health: Making healthy choices easier, DH, 2004 NHS Next Stage Review, DH, 2008 NHS Operating Framework, DH (refreshed annually) World Class Commissioning, DH Wanless Reports Our health, our care, our say: a new direction for community services, DH, 2006 These all provide frameworks that enable the prioritisation of sexual health at a local level. Within all these policy mechanisms, the focus is on quality of service, high standards in commissioning and good local decision-making to produce services that meet local need. These documents also promote keeping people healthy instead of just treating illness Sexual Health Commissioning Specific: Effective Commissioning of Sexual Health and HIV Services. A Sexual Health and HIV Commissioning Toolkit for Primary Care Trusts and Local Authorities, DH, 2003 Five steps to better sexual health & supporting people with HIV, THT, 2008 The NHS Trusts and PCTs (Sexually Transmitted Diseases) Directions, 2000 Recommended standards for sexual health services, MedFASH, 2005 Integrating the National Strategy for Sexual Health and HIV with Primary Medical Care Contracting, DH, 2005 Health Economics of Sexual Health: A Guide for Commissioning and Planning, DH, 2005 The Economics of Sexual Health, 2005, FPA National Sexual Health Strategy: Progress and priorities – working together for high quality sexual health. Review of the National Strategy for Sexual Health and HIV, MedFASH, 2008 Moving forward: Progress and priorities – working together for high-quality sexual health. Government response to the Independent Advisory Group’s review of the National Strategy for Sexual Health and HIV, DH, 2009 Sexual health – worth thinking about. A paper to inform national strategic planning for sexual health and HIV in 2011 and beyond, MedFASH, 2010 The national strategy for sexual health and HIV, DH, 2001 The national strategy for sexual health and HIV. Implementation action plan, DH, 2002 42 HIV: Recommended Standards for NHS HIV services, MedFASH, 2003 Standards for HIV Clinical Care, BHIVA, 2007 The African HIV Prevention Handbook, NAHIP, 2009 The Knowledge, The Will and The Power: Planning Prevention Framework, NAHIP, 2008 HIV and AIDS in African Communities: A Framework for Better Prevention and Care, DH/NAT/AHPN, 2005 ‘Don’t Forget the Children’. Guidance for the HIV testing of children with HIVpositive parents, BHIVA/ BASHH/ CHIVA, 2009 Children in need and blood borne viruses: HIV and hepatitis, DH, 2004 HIV Testing in Termination of Pregnancy Services: Conference Paper, BHIVA, 2009 Framework for Better Living with HIV in England, Sigma Research, 2009 Building on progress. Enhancing the response to HIV in England, Independent Advisory Group on Sexual Health and HIV, 2009 HIV in the United Kingdom: 2008 Report, HPA, 2008 Commissioning HIV Prevention Activities in England, NAT, 2007 The AIDS Support Grant: Making a difference?, NAT, 2009 Contraception: The Time is Now Achieving World Class Contraceptive and Abortion Services, Independent Advisory Group on Sexual Health and HIV, 2009 Long Acting Reversible Contraception- Clinical Guideline, NICE, 2005 STI: Genitourinary Medicine 48-hour Access: Getting to target and staying there, DH, 2008 Standards for the management of sexually transmitted infections (STIs), MedFASH & BASHH, 2010 Termination of Pregnancy: Standard Service Specification Template, DH, 2009 The Time is Now Achieving World Class Contraceptive and Abortion Services, Independent Advisory Group on Sexual Health and HIV, 2009 Teenage Pregnancy: National Teenage Pregnancy Strategy, Department of Health and Department for Children, Schools and Families, 1999 Teenage Pregnancy Strategy: beyond 2010, Department for Health and Department for Children, Schools and Families, 2010. Teenage Pregnancy and Sexual Health Marketing Strategy, Department of Health and Department for Children, Schools and Families, 2009. 43 Workforce: Primary Care Service Framework: Management of Sexual Health in Primary Care, NHS Primary Care Contracting, 2007 Sexual health competences: an integrated career and competence framework for sexual and reproductive health nursing across the UK, RCN, Revised 2009 Quality Standards for sexual health training: Striving for excellence in sexual health training, DH, 2005 The Manual for Sexual Health Advisers, Society of Sexual Health Advisers (SSHA), 2004 HPA: Sexually Transmitted Infections and Young People in the United Kingdom: 2008 Report Sexually Transmitted Infections and Men who have Sex with Men in the UK: 2008 Report Sexually Transmitted Infections in Black African and Black Caribbean Communities in the UK: 2008 report New guidelines for HIV testing and areas where wider HIV testing policies should be considered, HPA, 2008 HIV in the United Kingdom: 2008 report Other: Under 16s: consent and confidentiality in sexual health services, FPA, 2009 Evaluation of One-Stop Shop Models of Sexual Health Provision, UCL, 2007 One to one interventions to reduce the transmission of sexually transmitted infections (STIs) including HIV, and to reduce the rate of under 18 conceptions, especially among vulnerable and at risk groups, NICE, 2007 You’re Welcome quality criteria. Making health services young people friendly, DH, 2007 Independence, well-being and choice: our vision for the future of social care for adults, DH, 2005 Local Government and Public Involvement in Health Act, 2007 44