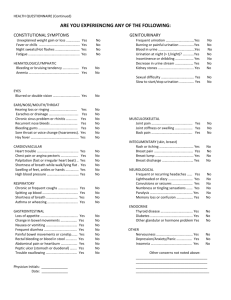
Health History pt.2
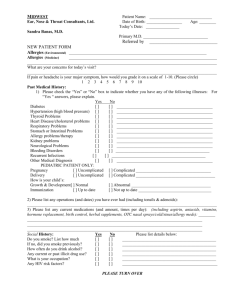
advertisement
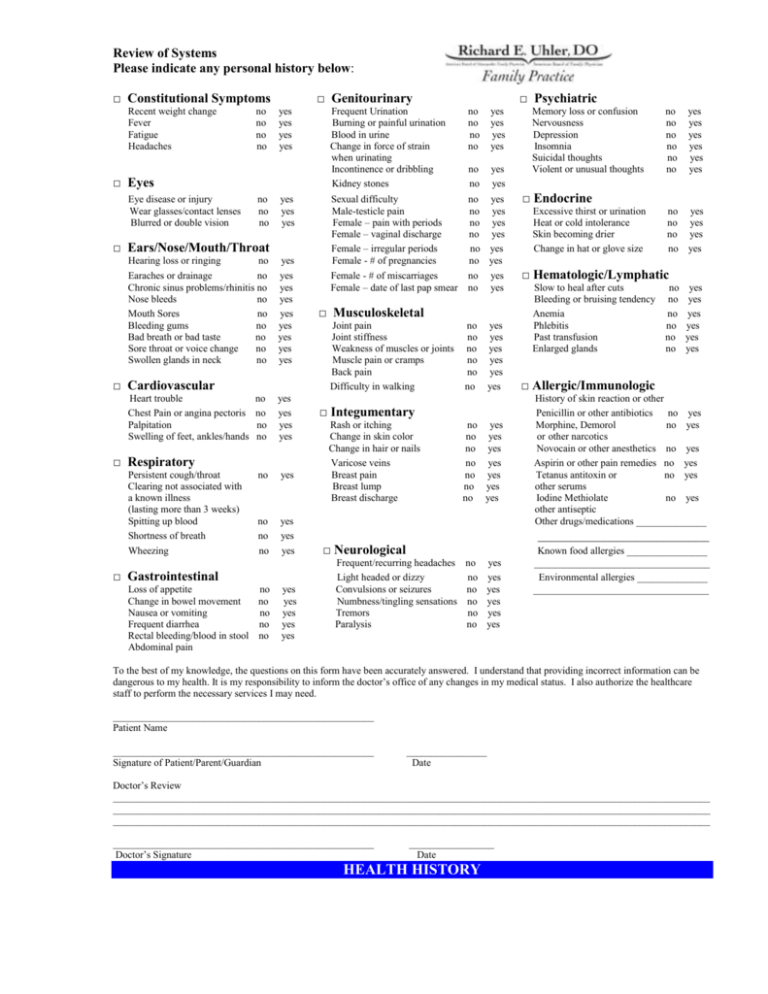
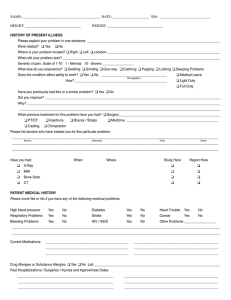
Review of Systems Please indicate any personal history below: □ Constitutional Symptoms Recent weight change Fever Fatigue Headaches no no no no □ Genitourinary yes yes yes yes □ Eyes Eye disease or injury Wear glasses/contact lenses Blurred or double vision no no no yes yes yes □ Ears/Nose/Mouth/Throat Hearing loss or ringing no yes Earaches or drainage no yes Chronic sinus problems/rhinitis no yes Nose bleeds no yes Mouth Sores no yes Bleeding gums no yes Bad breath or bad taste no yes Sore throat or voice change no yes Swollen glands in neck no yes □ Cardiovascular Heart trouble Chest Pain or angina pectoris Palpitation Swelling of feet, ankles/hands no no no no yes yes yes yes no yes no no no yes yes yes □ Respiratory Persistent cough/throat Clearing not associated with a known illness (lasting more than 3 weeks) Spitting up blood Shortness of breath Wheezing □ Gastrointestinal Loss of appetite no Change in bowel movement no Nausea or vomiting no Frequent diarrhea no Rectal bleeding/blood in stool no Abdominal pain yes yes yes yes yes Frequent Urination Burning or painful urination Blood in urine Change in force of strain when urinating Incontinence or dribbling Kidney stones □ Psychiatric no no no no yes yes yes yes no no yes yes Sexual difficulty no yes Male-testicle pain no yes Female – pain with periods no yes Female – vaginal discharge no yes Female – irregular periods no yes Female - # of pregnancies no yes Female - # of miscarriages no yes Female – date of last pap smear no yes □ Musculoskeletal Joint pain Joint stiffness Weakness of muscles or joints Muscle pain or cramps Back pain Difficulty in walking no no no no no no yes yes yes yes yes yes □ Integumentary Rash or itching Change in skin color Change in hair or nails Varicose veins Breast pain Breast lump Breast discharge no yes no yes no yes no yes no yes no yes no yes Memory loss or confusion Nervousness Depression Insomnia Suicidal thoughts Violent or unusual thoughts no no no no no no yes yes yes yes yes yes □ Endocrine Excessive thirst or urination Heat or cold intolerance Skin becoming drier Change in hat or glove size no yes no yes no yes no yes □ Hematologic/Lymphatic Slow to heal after cuts no Bleeding or bruising tendency no Anemia no Phlebitis no Past transfusion no Enlarged glands no yes yes yes yes yes yes □ Allergic/Immunologic History of skin reaction or other Penicillin or other antibiotics no yes Morphine, Demorol no yes or other narcotics Novocain or other anesthetics no yes Aspirin or other pain remedies no yes Tetanus antitoxin or no yes other serums Iodine Methiolate no yes other antiseptic Other drugs/medications ______________ __________________________ □ Neurological Frequent/recurring headaches Light headed or dizzy Convulsions or seizures Numbness/tingling sensations Tremors Paralysis no no no no no no yes yes yes yes yes yes Known food allergies ________________ ___________________________________ Environmental allergies ______________ ___________________________________ To the best of my knowledge, the questions on this form have been accurately answered. I understand that providing incorrect information can be dangerous to my health. It is my responsibility to inform the doctor’s office of any changes in my medical status. I also authorize the healthcare staff to perform the necessary services I may need. ____________________________________________________ Patient Name ____________________________________________________ Signature of Patient/Parent/Guardian ________________ Date Doctor’s Review _______________________________________________________________________________________________________________________ _______________________________________________________________________________________________________________________ _______________________________________________________________________________________________________________________ ____________________________________________________ Doctor’s Signature _________________ Date HEALTH HISTORY