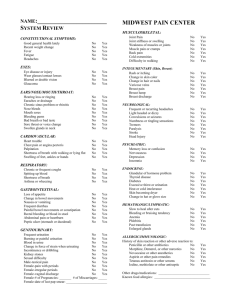
Health Questionnaire/Problem Summary
advertisement
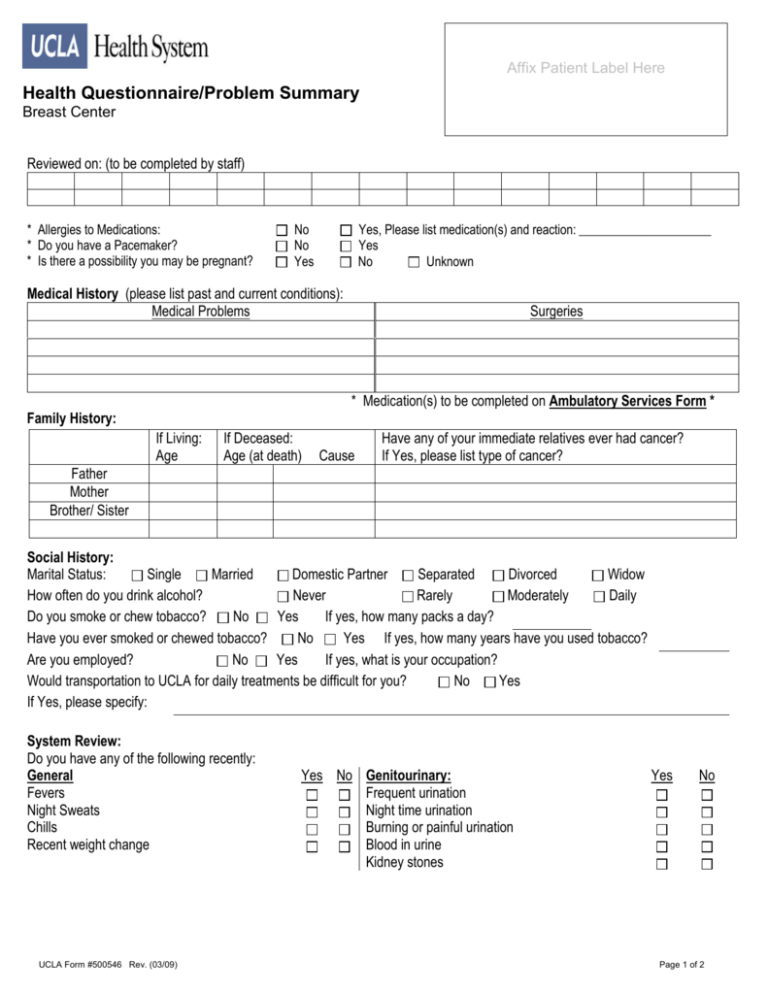
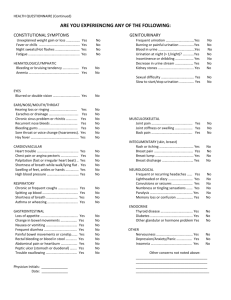
Affix Patient Label Here Health Questionnaire/Problem Summary Breast Center Reviewed on: (to be completed by staff) * Allergies to Medications: * Do you have a Pacemaker? * Is there a possibility you may be pregnant? No No Yes Yes, Please list medication(s) and reaction: _____________________ Yes No Unknown Medical History (please list past and current conditions): Medical Problems Surgeries * Medication(s) to be completed on Ambulatory Services Form * Family History: If Living: Age If Deceased: Age (at death) Cause Have any of your immediate relatives ever had cancer? If Yes, please list type of cancer? Father Mother Brother/ Sister Social History: Marital Status: Single Married Domestic Partner Separated Divorced Widow How often do you drink alcohol? Never Rarely Moderately Daily No Yes If yes, how many packs a day? Do you smoke or chew tobacco? Have you ever smoked or chewed tobacco? No Yes If yes, how many years have you used tobacco? Are you employed? No Yes If yes, what is your occupation? Would transportation to UCLA for daily treatments be difficult for you? No Yes If Yes, please specify: System Review: Do you have any of the following recently: General Fevers Night Sweats Chills Recent weight change UCLA Form #500546 Rev. (03/09) Yes No Genitourinary: Frequent urination Night time urination Burning or painful urination Blood in urine Kidney stones Yes No Page 1 of 2 Yes No Yes Skin: Hives Eczema Rash Musculoskeletal: Joint Pain Joint Swelling Injuries or Joint Fractures Eyes, Ears, Nose & Throat: Eye Disease or injury Do you wear glasses Change in vision Change in hearing Nose Bleeds Psychiatric: Depression Anxiety Hallucinations Paranoia Neurological: Fainting spells Convulsions Headaches Respiratory: Shortness of breath Cough Wheezing Hematologic: Anemia Have you had difficulty w/excessive bleeding Have you had abnormal bruising or bleeding Swollen glands Cardiovascular: Chest Pain Shortness of breath while walking or lying Down. Difficulty walking two blocks Swelling of hands, feet or ankles Heart Murmur Endocrine: Excessive thirst Intolerance to heat/cold Gastrointestinal: Peptic ulcer (stomach or duodenal) Black stool Recent change in bowel habits Frequent diarrhea Heartburn or indigestion Immunology/Allergy: Itchy eyes Allergies to animal or plants Runny Nose Gynecological (female Patients only): Date of first day of last period Age periods first started Number of pregnancies? Number of children: Number of miscarriages: Have you ever taken hormone replacement medications? If yes, what type? Have you ever taken Birth Control Pills? If yes, how long? Have you ever breastfed? Date of last Mammogram: List any other test: Age at first live birth? Date of last PAP smear: Breast History: Do you have any lumps in your breasts? Do you have breast pain? Do you have discharge? Please list any other symptoms: UCLA Form #500546 Rev. (03/09) Right Right Right Left Left Left How Long? How Long? How Long? Page 2 of 2 No