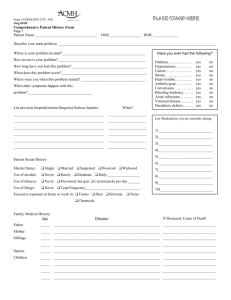
COMPREHENSIVE PATIENT HISTORY FORM
advertisement

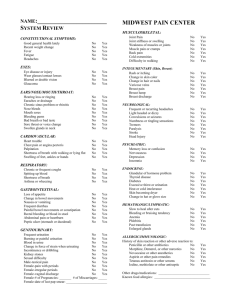
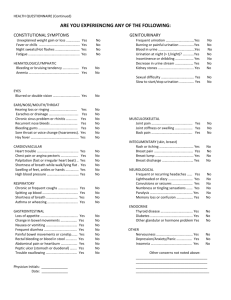
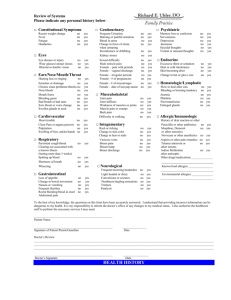
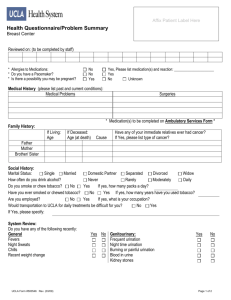
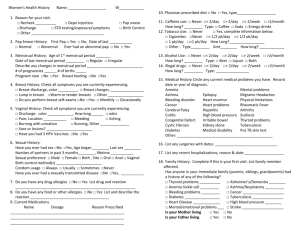
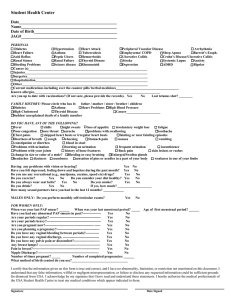
COMPREHENSIVE PATIENT HISTORY FORM Patient Name: _________________________________________ Date: ___________________ Describe your main problem __________________________________________________________________ Have you ever had the following? Where is your problem located? ___________________________________ Diabetes……………….. yes no How severe is your problem? _____________________________________ Hypertension…………... yes no How long have you had this problem? ______________________________ Cancer……………….… yes no Stroke………………….. yes no When does this problem occur? ___________________________________ Heart trouble…………... yes no Where were you when this problem started? _________________________ Arthritis/gout…………... yes no Convulsions……………. yes no What other things happen with this problem? ________________________ Bleeding tendency………yes no _____________________________________________________________ Acute infections…………yes no Venereal disease…………yes no Hereditary defects……….yes no List previous hospitalizations/Surgeries/Serious injures When List medications you are currently _____________________________________________ ____________ taking: _____________________________________________ ____________ 1) ______________________ _____________________________________________ ____________ 2) ______________________ _____________________________________________ ____________ 3) ______________________ _____________________________________________ ____________ 4) ______________________ _____________________________________________ ____________ 5) ______________________ 6) ______________________ Patient Social History Marital Status: ___Single___Married___Separated___Divorced___Widowed Use of alcohol: ___Never___Rarely___Moderate___Daily Use of tobacco: ___Never___Previously but quit___Current packs/day_____ Use of Drugs: ___Never___Type/Frequency__________________________ 7) ______________________ 8) ______________________ 9) ______________________ 10) ______________________ Excessive exposure at home or work to:___Fumes___Dust___Solvents ___Noise Family Medical History Age Diseases If Deceased, Cause of Death Father ____________ Mother ___________ Siblings___________ ____________ Spouse ____________ Children___________ ____________ _______________________________________ _______________________________________ _______________________________________ _______________________________________ _______________________________________ _______________________________________ _______________________________________ ________________________ ________________________ ________________________ ________________________ ________________________ ________________________ ________________________ ____________ _______________________________________ ________________________ PLEASE ANSWER ALL QUESTIONS Are you currently experiencing any of the following? CONSTITUTIONAL Good general health lately……………….. Recent weight gain………………………. Fever……………………………………… Fatigue……………………………………. Headaches………………………………… No No No No No Yes Yes Yes Yes Yes EYES Eye disease or injury……………………….. No Wear glasses/contact lenses…………………No Blurred or double vision…………………….No Glaucoma……………………………………No Yes Yes Yes Yes ENT Hearing loss………………………………….No Ringing in the ears…………………………...No Earaches or drainage…………………………No Sinus problems……………………………….No Nose bleeds…………………………………..No Mouth sores………………………………….No Bleeding gums……………………………….No Bad breath or bad taste………………………No Sore throat or voice change…………………..No Swollen glands in neck……………………….No Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes CARDIOVASCULAR Heart trouble………………………………….No Chest pain……………………………………..No Sudden heart beat changes……………………No Swelling of feet, ankles or hands………….….No Yes Yes Yes Yes RESPIRATORY Frequent coughing…………………………….No Spitting up blood……………………………...No Shortness of breath……………………………No Asthma or wheezing…………………………..No Yes Yes Yes Yes GASTROINTESTINAL Loss of appetite……………………………….No Change in bowel movements…………………No Nausea or vomiting…………………………...No Frequent diarrhea……………………………..No Painful bowel movements or constipation……No Blood in stool…………………………………No Stomach pain…………………………………No Yes Yes Yes Yes Yes Yes Yes GENITOURINARY Frequent urination…………………………….No Yes Burning or painful urination…………………..No Yes Blood in urine…………………………………No Yes Change of force of strain when urinating……..No Yes Incontinence or dribbling……………………..No Yes Kidney stones…………………………………No Yes Sexual difficulty………………………………No Yes Male – testicle pain…………………………….No Yes Female – pain with periods…………………….No Yes Female – irregular periods…………………….No Yes Female – vaginal discharge……………………No Yes Female - # of pregnancies ____# of miscarriages ____ Female – date of last pap smear____________________ Female – findings of last pap smear ___Normal ___Abn. MUSCULOSKELETAL Joint pain……..………….. No Joint stiffness or swelling… No Weakness of muscles or joints…….No Muscle pain or cramps…….………No Back pain………………………….No Cold extremities…………………...No Difficulty in walking………………No Yes Yes Yes Yes Yes Yes Yes SKIN Rash or itching……………………..No Change in skin color………………..No Change in hair or nails…………...…No Varicose veins………………………No Breast pain………………………….No Breast lump…………………………No Breast discharge…………………….No Yes Yes Yes Yes Yes Yes Yes NEUROLOGICAL Frequent or recurring headaches ……No Light headed or dizzy….………….…No Convulsions or seizures……………...No Numbness or tingling sensations ……No Tremors………………………...........No Paralysis……………………………..No Stroke………………………………..No Head injury…………………………..No Yes Yes Yes Yes Yes Yes Yes Yes PSYCHIATRIC Memory loss or confusion……..……No Nervousness………………………...No Depression…………………………..No Sleep problems……………………...No Yes Yes Yes Yes ENDOCRINE Glandular or hormone problem……..No Thyroid disease……………………..No Diabetes…………………………….No Excessive thirst or urination………..No Heat or cold intolerance…………….No Dry skin……………………………..No Change in hat or glove size………....No Yes Yes Yes Yes Yes Yes Yes HEMATOLOGIC/LYMPHATIC Slow to heal after cuts…………….No Easily bruise or bleed……………...No Anemia………………………….…No Phlebitis……………………………No Past transfusion……………………No Enlarged glands……………………No Yes Yes Yes Yes Yes Yes ALLERGIC/IMMUNOLOGIC History of skin reaction or other adverse reactions to: Penicillin or other antibiotics………No Morphine, Demerol, other narcotics No Novocaine or other anesthetics…….No Tetanus antitoxin or other serums…No Iodine, merthiolate, other antiseptic No Known food allergies: _________________ Yes Yes Yes Yes Yes PATIENT: Sign here ______________________________ PHYSICIAN: Sign here ____________________________