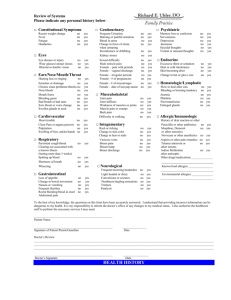
Patient History
advertisement

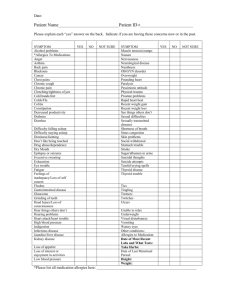
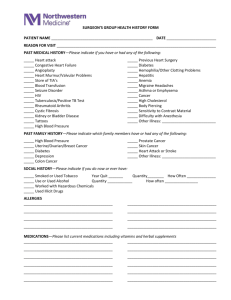
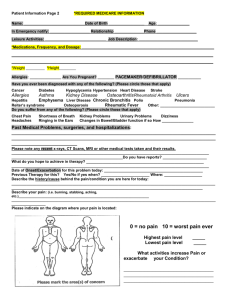
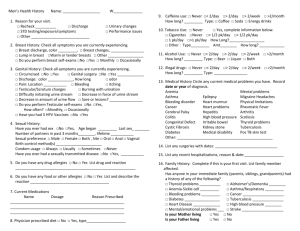
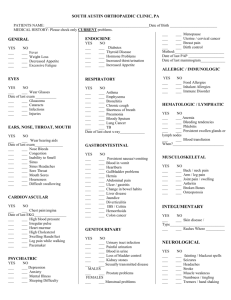
Name: ___________________________________________ Date:_____________________ SS#: ____________________________ Height: _______________________________ Weight: _______________________________ History of Present Illness Please explain your problem in one sentence:________________________________________________________________________ Where is your problem located? Severity of pain. Scale of 1-10 1 - Minimal 10 - Severe _________________ Does the condition affect ability to work? Yes No ___________________________________ Medical Leave Full Duty Did you improve?_ _____________________________________________________________________________________________ _ ___________________________________________________________________________________________________________ Work related? Yes No Right Left Location_____________________________________________________________ When did your problem start?_____________________________________________________________________________________ What else do you experience? Swelling Grinding Give way Catching Popping Locking Sleeping Problems Occupation Light Duty How? _________________________________________________ Have you previously had this or a similar problem? Yes No Why?________________________________________________________________________________________________________ What previous treatment for this problem have you had? Surgery_______________________________________________________ PT/OT Injections Casting Chiropractor Braces / Straps Medicine_ _________________________________________________ Please list doctors who have treated you for this particular problem: _______________________________________________________________________________________________________________ (Name) (Specialty) (City) (Date) _______________________________________________________________________________________________________________ _______________________________________________________________________________________________________________ Have you had: X-Ray Bone Scan When Where Study Here MRI CT Report Here Patient Medical History Please circle Yes or No if you have any of the following medical problems. High blood pressure Yes No Diabetes Yes No Heart Trouble Yes Bleeding Problems Yes No HIV / AIDS Yes No Other Problems _________________ Respiratory Problems Yes No Stroke Yes No Cancer Yes No No ________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________ Current Medications: _____________________________________________ ______________________________________________ _____________________________________________ ______________________________________________ _____________________________________________ ______________________________________________ Drug Allergies or Substance Allergies Yes No List:____________________________________________________________________ Past Hospitalizations / Surgeries / Injuries and Approximate Dates _ ___________________________________________________ ___________________________________________________ _ ___________________________________________________ ___________________________________________________ _ ___________________________________________________ ___________________________________________________ Family History: Have any of your relatives (e.g.. - Mother, Father, Brother, Sister, Grandparent) ever had: 1. Heart Disease 2. High Blood Pressure 3. Diabetes 4. Stroke 5. Cancer (Location) 6. Thyroid Disease 7. Other Disease Yes ____ ____ ____ ____ ____ ____ ____ No ____ ____ ____ ____ ____ ____ ____ Relationship ____________________________ ____________________________ ____________________________ ____________________________ ____________________________ ____________________________ ____________________________ Social History: Marital Status: Single Married Separated Divorced Widowed Alcohol Use: Never Rarely Moderate Daily How much? _______ Occupation: Tobacco Use: Drug Use: Never Never Quit/ When ___________ __________________ Current smoker / packs per day __________ Type & Frequency ________________________________ Other: ___________________________________________ Review of Systems (ROS) Please circle Yes or No if you have any of the following problems. Constitutional Good General Health Recent Weight Change Night sweats, fevers Fatigue Yes Yes Yes Yes No No No No Ears/Nose/Mouth/Throat Hearing loss or ringing Sinus Problems Nose Bleeds Sore throat/voice change Yes Yes Yes Yes No No No No Eyes Wear glasses/contacts Blurred/double vision Eye disease or injury Glaucoma Yes Yes Yes Yes No No No No Cardiovascular Chest pain Palpitations Heart Trouble Swelling hands / feet Yes Yes Yes Yes No No No No Respiratory Shortness of breath Cough Wheezing / Asthma Coughing up blood Yes Yes Yes Yes No No No No Gastrointestinal Nausea / vomiting Abdominal pain Rectal Bleeding Bowel problems Yes Yes Yes Yes No No No No Musculoskeletal Muscle pain or cramps Stiffness/swelling joints Joint pain Trouble walking Yes Yes Yes Yes No No No No Neurological Frequent Headaches Paralysis or tremors Convulsions/seizures Numbness/tingling Yes Yes Yes Yes No No No No Integumentary (Skin / Breast) Change in hair or nails Yes Rashes or itching Yes Breast lump Yes Breast pain or discharge Yes No No No No Endocrine Excessive thirst/urination Thyroid disease Hormone Problem Yes Yes Yes No No No Hematologic / Lymphatic Bruise easily Slow to heal Enlarged Glands No No No No Genitourinary - Female Only Blood in urine Yes Kidney Stones Yes Sexual problems Yes Menstrual problems Yes Genitourinary - Male Only Blood in urine Yes Kidney Stones Yes Sexual problems Yes Testicle pain Yes Yes Yes Yes Allergic / Immunologic No Food Allergies No Aspirin Allergies No Antibiotic Allergies No No No No Yes No Yes No Yes No Psychiatric Insomnia Yes No Confusion/memory loss Yes No Depression Yes No Patient Statement: To the best of my knowledge, the above information is accurate and complete. Signed: _________________________________________ Date: _________________ Physician Statement: I have reviewed the questionnaire with the patient. Signed: _________________________________________ Date: _________________