Allergic Reaction
advertisement

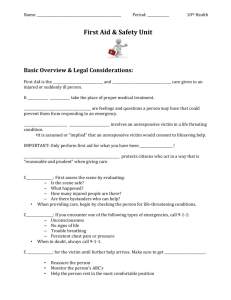
Emergency Medical Guidelines 1 Medical Table of Contents Basic Supplies Needed in a First Aid Kit ..................................3 Medical/Health Emergencies .................................................4 Emergency Procedures...........................................................5 Triage .....................................................................................6 START .....................................................................................7 Allergic Reactions ...................................................................8 Bleeding .................................................................................9 Pressure Points .....................................................................10 Asthma .................................................................................11 Choking.................................................................................12 Heimlich Maneuver ..............................................................13 CPR .......................................................................................14 Child CPR ..............................................................................15 Seizures ................................................................................16 Stabbing/Gunshot Wounds ..................................................17 Diabetes ...............................................................................18 Heat Stroke...........................................................................19 Poisoning ..............................................................................20 Behavior Concerns ...............................................................21 OSHA – Exposure to Blood and/or Body Fluids ....................22 AED (Defibrillator) ................................................................23 2 Basic Supplies Needed in a First-Aid Kit 2”x2” and 4”x4” Sterile Gauze Dressings – Individually Wrapped Sterile Gauze by the roll Sterile self-adhesive pads Adhesive Tape Band-aids (various sizes) Barrier Device (CPR mask) First Aid Spray Cotton balls Q-Tips Cold Packs First Aid Cream Antibiotic Ointment Tweezers 2 – Triangular Bandages/slings Vaseline Petroleum Jelly Alcohol Sharp Scissors Thermometer and Shields Tongue Depressors Gloves Whenever an emergency arises, please call 9-1-1. Once emergency services have been summoned and you find that you don’t need their services, the dispatch center can notify the unit to disregard. It is always better to call and have them on their way and not need them, than to desperately need their services and not have them accessible!!!! 3 MEDICAL/HEALTH EMERGENCIES Have 9-1-1 called immediately for: Anaphylactic Reaction (severe allergic reaction) Head Injury with loss of consciousness Amputation Neck or back injury Bleeding (severe) Heat Stroke Breathing difficulty (persistent) Paralysis of any type Broken Bones Poisoning Burns (chemical, electrical – 3rd degree) Seizure (if not history or trauma-related) Chest Pain (severe) Shock Choking Traumatic injury Drowning Unconsciousness Electrical Shock Wound (deep or extensive) Frostbite Other – when in doubt Never leave an ill or injured individual unattended. Have someone else call 9-1-1 and then attempt to reach parents or guardians. Do not wait for the parent’s permission before you call 9-1-1, if it is truly a medical emergency, call immediately. The parent cannot instruct you to refrain from calling 9-1-1. Religious, ethnic or cultural reasons are not sufficient to remove the responsibility from the division for not providing prompt, appropriate medical aid. When in doubt, call 9-1-1. Err on the side of caution. The school division does not incur liability by calling 9-1-1. However, the school division can incur significant liability by failing to call 9-1-1. Concern over who pays ambulance and emergency room bills is not important in a crisis. Do NOT move an injured individual or allow the person to walk (bring help and supplies to the individual). Other school staff or responsible adults should be enlisted to help clear the area of students who may congregate following an injury or other emergency situation. Henry County Schools policy states that at least 3 staff members from Elementary and 5 from Middle and High Schools be certified in CPR/1 st Aid and Diabetes Education annually. 4 Emergency Procedures For Injury or Illness 1. Remain calm and assess the situation. Be sure the situation is safe for you to approach. The following dangers will require caution: live electrical wires, gas leaks, building damage, fire or smoke, traffic or violence. 2. Notify building response team. 3. A responsible adult should stay at the scene and give help until the person(s) designated to handle emergencies arrives. This person(s) will take charge of the emergency and render first aid as needed. 4. Do NOT give medications unless there has been prior approval by the student’s guardian and doctor according to School BD policy. 5. Do NOT move a severely injured or ill student unless absolutely necessary for immediate safety. If moving is necessary, follow guidelines in NECK AND BACK section. 6. The responsible school authority or a designated employee should notify the parent/legal guardian of the emergency as soon as possible. 7. A responsible individual should remain with the injured student on the scene and at the hospital until a family member arrives. Post Crisis Intervention Following Serious Injury or Death Discuss with Building Response Team Determine level of intervention for staff and students. Counseling rooms (preferably Media Center) for students and/or staff. Escort affected students, siblings and close friends and other affected individuals to meet with Crisis Team staff members. Assess stress level of staff. Recommend counseling as needed. Follow-up with students and staff who receive counseling. Designate staff person(s) to attend funeral. 5 Triage Triage means “to sort” and “to do the most good for the most people.” Triage Categories GREEN – “Walking Wounded” Minor injuries that can wait for longer periods of time. Injuries include: minor lacerations, contusions (bruising), sprains and superficial burns. YELLOW – Seriously Injured Injuries may include: Penetrating abdominal wounds, severe eye injury, fractures, burns (other than face, neck or perineum), and open thoracic (chest) wounds. RED – Critically Wounded or LifeThreatening Examples may include: Airway obstruction or heart failure, external hemorrhage, shock, sucking chest wound and burns of the face and neck. BLACK – Deceased Injuries may include: Severe head injury, burns over 85% of the body, multi-system trauma and signs of impending death. 6 START Start is the mnemonic when performing a triage assessment in reference to a mass casualty incident. *Simple *Triage *And *Rapid *Transport START Triage Respirations Under 30/minute Over 30/minute NO Perfusion Immediate Cap refill >2 sec, Position Airway NO Dead or Expectant Control Bleeding YES Cap refill < 2 sec, Mental Status Immediate Immediate Failure to follow simple commands Can follow simple commands Delayed Immediate 7 Allergic Reaction Children may experience a delayed allergic reaction up to 2 hours following food ingestion, bee sting, etc. Does the student have any symptoms of a severe allergic reaction which may include flushed face, dizziness, seizures, confusion, weakness, paleness, hives over body, blueness around mouth or eyes, difficulty breathing, drooling or difficulty swallowing, or loss of consciousness? Symptoms of a mild allergic reaction: Red, watery eyes Itchy, sneezing, runny nose Hives or rash on one area Check student’s airway Look, listen and feel for breathing. Check breathing status NO Adult(s) supervising student during normal activities should be aware of the student’s exposure & should watch for any delayed symptoms of a severe allergic reaction for up to 2 hours. YES Is student having difficulty breathing or clearing throat? YES If student is so uncomfortable that he/she is unable to participate in school activities, contact responsible school authority and parent or legal guardian. NO Administer standing order for Benadryl (according to physician’s orders) If student begins to have difficulty breathing …. Refer to student’s plan. Administer standing order for Epinephrine (according to child’s age and weight). CALL 9-1-1, Contact responsible school authority and parent or guardian. 8 Bleeding The human body circulates 5-7 gallons of blood every minute. Oxygenated blood keeps the organs supplied with oxygen which is imperative to sustaining life. Is bleeding bright red and spurting? Is injured part amputated or severed? NO YES Bleeding is dark red and flowing steady or oozing. CALL 9-1-1 Expose wound. Apply direct pressure over wound with a pad or cloth. Have victim lie on his back if able. Raise injured area above level of the heart. Apply a firm dressing. Check circulation and reassess every 10 minutes. Keep applying more bandages and hold pressure. Expose wound. Cover wound with clean bandage. Do not remove old dressing. Continue to re-enforce and add more gauze if bleeding through existing dressing. Seek medical attention if necessary. Is patient pale and less coherent? YES NO Continue as above. Raise legs at least 6-12.” Continue to monitor while waiting for EMS personnel. If unable to stop bleeding, consider using a constrictive wrap or apply pressure on a pressure point (brachial, femoral or radial arteries). Cover student with a blanket. 9 Pressure Points Pressure points are places where an artery can be pressed against an underlying bone to prevent the blood from flowing past. Use a pressure point to reduce severe bleeding only as a last resort and then with extreme care. Is patient bleeding from legs and feet? Lay the victim down and bend the injured leg at the knee. Press down firmly in the center of the groin, one thumb on top of the other, against the rim of the pelvis. Do not press forcefully for longer than 6 minutes. Is the patient bleeding from arms and hands? Hold the victim’s arm at right angles to the body. The brachial artery runs along the inner side of the upper arm. To control bleeding from the lower arm, put one hand under the upper arm and press your fingers against the bone. Have someone to immediately call 9-1-1. 10 ASTHMA Students with a history of breathing difficulties including asthma should be known to appropriate staff. A care plan should be developed. Henry Co. policy allows a student to possess and use an asthma inhaler at school if orders are on file in the office. A student with asthma/wheezing may have breathing difficulties which may include: Did breathing difficulty develop rapidly? Are the lips, tongue or nail beds turning blue? Uncomfortable coughing Wheezing – a high-pitched sound during exhale. Rapid breathing Flaring (widening) of the nostrils. Feeling of tightness of the chest. Not able to speak in a full sentence. Increased use of accessory muscles to breathe. NO Refer to Student’s Emergency Plan YES YES Does student have doctor and parent approved medication? (administer medication) NO Remain Calm. Encourage student to sit quietly, breathe slowly and deeply in through the nose and out through the mouth. CALL 9-1-1. Has an inhaler already been used? Are symptoms getting worse? YES CALL 9-1-1. NO Administer medication as ordered Contact responsible school authority and parent. 11 CHOKING . Choking is defined as the inability to breathe. Causes may be from food, inhaling toxic fumes, drowning or strangulation. Physical Findings: Victim conscious and making attempts to breathe Complete or near-complete inability to speak Grasping of neck, usually with both hands, palms toward neck. Rapid onset of cyanosis (blueness of lips and fingertips), cessation of breathing efforts, and loss of consciousness. Is victim unable to cough, speak or breathe? YES CALL 9-1-1 NO Continue to monitor. If breathing becomes more difficult or ceases. Do Heimlich Maneuver (see following page) Make sure someone calls parent/guardian. 12 HEIMLICH MANEUVER Action 1. Stand behind the person and wrap your arms around his/her waist. Rationale 1. Rescuer’s arms should be just above the belt line. The victim’s head, arms, and upper torso are allowed to lean forward. 2. Make a fist with one hand and grasp the fist with your other hand. Place the thumb side of your fist against the victim’s abdomen slightly above the navel and below the rib cage. 2. This action cannot be done on obese or pregnant victims. For these victims, the rescuer must do chest thrusts. 3. Press your fist into the victim’s abdomen with a quick upward thrust. 3. This action produces a sudden sharp rise in intra-thoracic pressure which will eject the bolus or object that is occluded. If patient goes unresponsive, begin CPR. (See CPR). 13 CPR (CardioPulmonary Resuscitation) CPR is a combination of breaths and chest compressions given to a victim who is in cardiac arrest. (Cardiac arrest is when the heart is not beating). When administering CPR, it is important for it to be performed according to the American Heart Association standards. The 3 major steps are: C-A-B C ompression Adult CPR A irway B reathing Compression If the victim is still not breathing normally, coughing or moving, begin chest compressions. Push down on the chest 11/2 to 2 inches 30 times right between the nipples. Pump at the rate of 100/minute, faster than once per second. Airway Tilt the head back and listen for breathing. If not breathing normally, pinch nose and cover the mouth with yours and blow until you see the chest rise. Give 2 breaths. Each breath should take 1 second. Breathing CONTINUE WITH 2 BREATHS AND 30 PUMPS UNTIL HELP ARRIVES NOTE: This ratio is the same for one-person & two-person CPR. In two-person CPR the person pumping the chest stops while the other gives mouth-to-mouth breathing. 14 CHILD CPR CPR for children is similar to CPR for adults. The compression to ventilation ratio is 30:2. There are, however, 3 differences. 1) If you are alone with the child, give two minutes of CPR before calling 911. 2) Use the heel of one hand for chest compressions . (Prevents compressing too deep). 3) Press the sternum approximately one-third to one-half the depth of the chest height. Continue CPR until Emergency Responders arrive and take over care of the patient. 15 SEIZURES Students with a history of seizures should be known to appropriate school personnel. An emergency care plan should be on file containing a description of the onset, type, duration and after effects of the seizures. Seizures may be any of the following: Episodes of staring with loss of eye contact Staring involving twitching of the arm and leg muscles Generalized jerking movements of the arms and legs Unusual behavior for that person (running, belligerence, making strange sounds, etc.) Refer to student’s emergency care plan. Observe details of the seizure for parent/legal guardian, emergency personnel or physician. Note: If student seems off balance, place him/her on the floor (on a mat) for observation and safety. DO NOT restrain movements. Move surrounding objects to avoid injury. DO NOT place anything between teeth or give anything by mouth. Keep airway clear by placing student on his/her side. A pillow should not be used. Seizures are often followed by sleep. The student may also be confused. This may last from 15 minutes to an hour or more. After the sleeping period, the student should be encouraged to participate in all normal class activities. NO Duration Kind of movement or behavior. Body parts involved. Loss of consciousness, etc. Is student having a seizure longer than 5 minutes? Is student having a seizure following one another at short intervals? Is student without a known history of seizures having a seizure? Is student having any breathing difficulties after the seizure? YES Contact responsible school authority and parent or legal guardian. CALL 9-1-1. 16 STABBING AND GUNSHOT INJURIES Call 9-1-1 for EMS and police. Intervene only if the situation is safe for you to approach. Refer to your school’s policy for addressing violent incidents. Wear disposable gloves when exposed to blood or other body fluids. Check student’s airway. Look, listen and feel for breathing. If student stops breathing, start CPR. See section on CPR. Is the student: Losing consciousness? Having difficulty breathing? Bleeding uncontrollably? YES NO 1. 2. 3. 4. 5. + Lay student down in a position of comfort if he/she is not already doing so. Elevate feet/legs 8-10 inches unless painful. Press injured area firmly with a clean bandage to stop bleeding. Elevate injured part gently, if possible to decrease bleeding. Keep body temperature normal. Cover with a blanket if available. Provide emotional support. Keep calm and try to calm patient. Contact parent/guardian and school authorities. 17 DIABETES A student with diabetes should be known to all appropriate staff. An Individualized Health Care should be available. Staff in a position to administer approved medications should be trained annually. A student with diabetes may have the following symptoms: Irritability and feeling upset Personality changes Sweating and feeling “shaky.” Loss of consciousness Confusion or strange behavior. Rapid, deep breathing. Refer to student’s Individualized Health Care Plan. Is the student: - Unconscious or losing consciousness? Having a seizure? Unable to speak? Having rapid, deep breathing? NO Is a blood sugar monitor available? YES Give student “quick acting sugar” such as fruit juice, regular soda, sugar, hard candy, cake icing gel or instant glucose. Allow student to check blood sugar. Continue to watch the student in a quiet place. The student should begin to improve in approx. 10 minutes. Is blood sugar less than 70 or “LOW” or is blood sugar “HIGH” according to IHP. Allow student to recheck sugar. LOW YES HIGH Contact parent/guardian and appropriate school authority. Continue to watch student. Is the student improving? NO CALL 9-1-1. Administer Glucagon if ordered and available. Turn patient on side in case of vomiting. 18 HEAT STROKE/HEAT EXHAUSTION Heat Emergencies are caused by spending too much time in the heat. Heat emergencies can be life-threatening situations. Strenuous activity in the heat may cause heat-related illness. Symptoms include: Is student unconscious or losing consciousness? Red, hot, dry skin Weakness and fatigue. Cool, clammy hands Vomiting Loss of consciousness. Remove student from the heat to a cooler place. Have student lie down. NO YES 1. Quickly remove student from heat to a cooler place. 2. Put student on his/her side to protect the airway. 3. Look, listen and feel for breathing. 4. If student stops breathing, start CPR. See “CPR.” Cool rapidly by completely wetting clothing with room temperature water. Do NOT use ice water. Does student have hot, dry, red skin? Is student vomiting? Is student confused? YES CALL 9-1-1. NO Give clear fluids such as water, 7-Up or Gatorade frequently in small amounts if student is fully awake and alert. Contact parent/guardian and school authority. Contact responsible parent/guardian and school authority. 19 POISONING AND OVERDOSE Poisons can be swallowed, inhaled, absorbed through the skin or eyes or injected. Call Poison Control when you suspect poisoning from: Medicines Insect bites and stings Snake bites Plants Chemicals/cleaners Possible warning signs of poisoning include: Pills, berries or unknown substance in student’s mouth Burns around mouth or on skin Strange odor on breath Sweating Nausea or vomiting Dizziness or fainting Seizures or convulsions. Do NOT induce vomiting or give anything UNLESS instructed to by Poison Control. With some poisons, vomiting can cause greater damage. Do NOT follow the antidote label on the container, it may be incorrect. Drugs/alcohol Food poisoning Inhalants OR if you are not sure. Wear disposable gloves. Check student’s mouth Remove any remaining substances from mouth. If possible, find out: Age and weight of student What the student swallowed What type of “poison” it was How much and when it was taken. CALL POISON CONTROL 1-800-222-1222 Follow their advice! CALL 9-1-1. If student becomes unconscious, place on his/her side. Check airway. Look, listen and feel for breathing If student stops breathing, begin CPR. See “CPR” section. Contact parent/guardian and school authority. Send sample of the vomited material and ingested material with its container (if available) to the hospital with the student. 20 BEHAVIORAL EMERGENCIES Students with a history of behavioral problems, emotional problems or other special needs should be known to school staff. Behavioral or psychological emergencies may present in different forms such as depression, anxiety, phobias, suicidal thoughts, and violent behavior. Intervene only if the scene is safe. Does the student have visible injuries? YES NO Treat injuries. Call 9-1-1 if warranted. - - YES Call the Police. Does student’s behavior present an immediate risk of physical harm to anyone? Does the student have a weapon? NO The cause of the behavior may be due to numerous reasons including: - Fever - Diabetes - Poisoning/overdose - Alcohol or drug use - Head injury. The student needs to be evaluated by a health care provider to determine the cause of his actions. Suicidal and violent behavior should be taken seriously. If the student has threatened to harm himself or others, follow your protocol for suicide. Contact school authority and parent/guardian. 21 EXPOSURE TO BLOOD AND/OR BODY FLUIDS Wash affected area with copious amounts of soap and water. If eyes, nose or mouth are affected, rinse with copious amounts of water. If skin is broken, contact responsible school authority and parent/legal guardian. URGE immediate medical care. Parents/legal guardian of the student(s) should be notified that their child may have been exposed to blood and/or body fluids from another student. Individual confidentiality must be maintained when sharing this information. Check student(s) immunization record(s) to determine last tetanus injection and dates of 3 Hepatitis B injections. 22 AUTOMATED EXTERNAL DEFIBRILLATOR (AED) For Children Over 1 Year of Age and Adults CPR and AED’s are to be used when a person is unresponsive or when breathing or heart beat stops. All schools in Henry County have an AED. 1. Tap or gently shake the shoulder. Shout, “Are you Okay?” If victim is unresponsive, shout for help and send someone to CALL 9-1-1 and get the school’s AED. 2. Follow primary steps for CPR. 3. If available, set up the AED according to instructions. a. Connect Electrodes. b. Apply Pads c. Press “Analyze” button. Follow prompts. Depending on how the AED analyzes the heart rhythm, you may be advised to deliver several shocks, no shocks, or shocks followed by CPR. 23