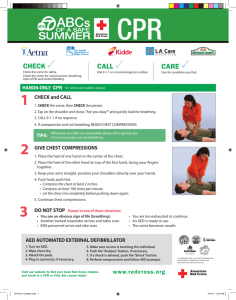
Pediatric life support
advertisement
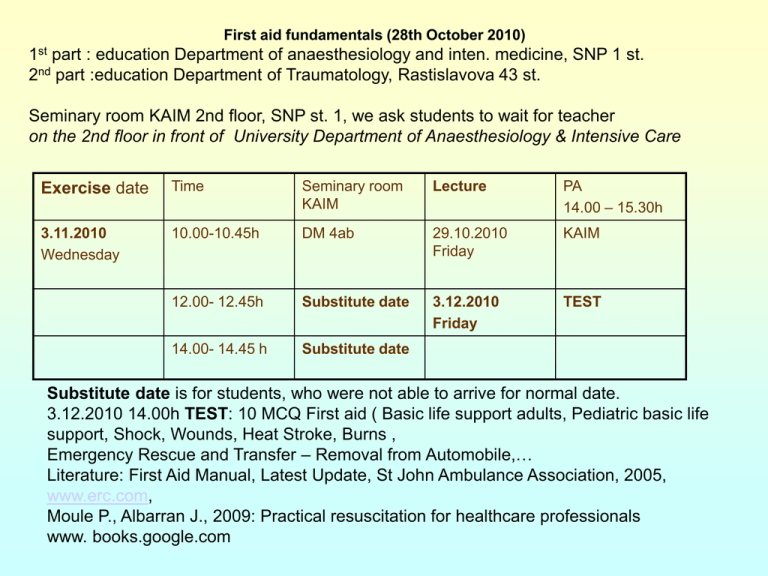
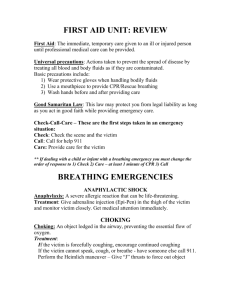
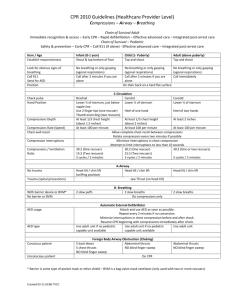
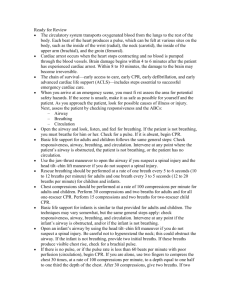
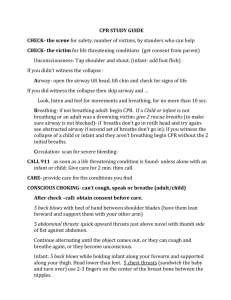
First aid fundamentals (28th October 2010) 1st 2nd part : education Department of anaesthesiology and inten. medicine, SNP 1 st. part :education Department of Traumatology, Rastislavova 43 st. Seminary room KAIM 2nd floor, SNP st. 1, we ask students to wait for teacher on the 2nd floor in front of University Department of Anaesthesiology & Intensive Care Exercise date Time Seminary room KAIM Lecture PA 14.00 – 15.30h 3.11.2010 Wednesday 10.00-10.45h DM 4ab 29.10.2010 Friday KAIM 12.00- 12.45h Substitute date 3.12.2010 Friday TEST 14.00- 14.45 h Substitute date Substitute date is for students, who were not able to arrive for normal date. 3.12.2010 14.00h TEST: 10 MCQ First aid ( Basic life support adults, Pediatric basic life support, Shock, Wounds, Heat Stroke, Burns , Emergency Rescue and Transfer – Removal from Automobile,… Literature: First Aid Manual, Latest Update, St John Ambulance Association, 2005, www.erc.com, Moule P., Albarran J., 2009: Practical resuscitation for healthcare professionals www. books.google.com Paediatric basic life support Monika Grochová MD, PhD Klinika anestéziológie a intenzívnej medicíny LF UPJŠ a UNLP Košice • www.erc.edu www.resus.org.uk • Resuscitation (2005, 2010) 67 Supplement • Resuscitation (2005, 2010) 67 Basic life support A B C irway – airways opening reathing – arteficial ventilation irculation – recovery of circulation CBA adults Paediatric basic life support • simplification based on the knowledge that many children receive no resuscitation at all because rescuers fear doing harm Age: - An infant is a child under 1 year of age - a child is between 1 year and puberty 25 kg, 8. years CPR IN CHILDREN • Adult CPR techniques can be used on children • Compressions 1/3 of the depth of the chest 30 3 0 BASIC LIFE SUPPORT (BLS) Approach safely Check response Shout for help Open airway Campbell head tilt and chin lift, BASIC LIFE SUPPORT (BLS) Approach safely Check response Shout for help Open airway Check breathing Look, listen and feel for NORMAL breathing Breathing • Take a breath and cover the mouth and nasal apertures of the infant with your mouth, making sure you have a good seal • Blow steadily into the infant’s mouth and nose over 1—1.5 s, sufficient to make the chest visibly rise • Take another breath and repeat this sequence five times Breathing No effective breathing: - the airway may be obstructed • Open the child’s mouth and remove any visible obstruction. • Ensure that there is adequate head tilt and chin lift, try the jaw thrust method • Make up to five attempts to achieve effective breaths; if still unsuccessful, move on to chest compressions Breathing, circulation • look for signs of a circulation any movement, coughing normal breathing=circulation is present (not agonal gasps, which are infrequent, irregular breaths) Basic life support • Chest compressions – – – – – – – – – To 1. year 2 fingers (2 thumbs circular) Over 1. yer one hand/two hands Low part of sternum Thumb over processus xiphoideus Compression by 1/3 of antero-posterior distance AED Children > 1 year Smaller size of pads for children to 8 years 50 – 75 J (4 J/kg) Chest compression Chest compressions • to depress the sternum by approximately one third of the depth of the chest • and repeat at a rate of about 100 min−1 Chest compressions : breaths 30:2 AED IN CHILDREN • Age > 8 years • use adult AED • Age 1-8 years • use paediatric pads / settings if available (otherwise use adult mode) • Age < 1 year • use only if manufacturer instructions indicate it is safe AED DEFIBRILLATION ATTACH PADS TO CASUALTY’S BARE CHEST ANALYSING RHYTHM - DO NOT TOUCH VICTIM SHOCK INDICATED • Stand clear • Deliver shock SHOCK DELIVERED FOLLOW AED INSTRUCTIONS 30 2 Recovery position Approach safely Approach safely Check response Check response Shout for help Shout for help Open airway Open airway Check breathing Check breathing Call 112 Call 112 5 rescue breaths Attach AED 30 chest cmpressions Follow voice prompts Anatomical diferencies of airwais by children Postresuscitation care • Aproppriate tissue perfusion • Cooling – if unconsiousness after CPR – 32 – 34°C of body core 12 – 24 hours – Warming 0,25 – 0,5°C / hour – AE- infection, koagulopathy, glykémia, ións, circulation – Avoid hyperthermia - antipyretics ETICS and CPR • Start – not start • Parents´presens during CPR • Decision to stp CPR- team leader, not parents CPR of newborn Newborn resuscitation • Lungs distension- ambu- bag with face mask, in term newborn f: 30-60/min if bradycardia persists - increase oxygen concentration • Mecónium – desuflation by weak newborns • Compressions- breathing ratio 3:1 90 compressionsií and 30 breaths • Adrenalín, if despite art. Vent.with O2 bradycardia <60/min dose 0,01-0,03 mg/kg i.v., into ETT 5-7 x more • Check HR every 30 sekúnd, STOP if HR > 60/min • Circulation support evective only by lungs distension • Temperature of body core maintenance Foreign body airway obstruction – Combination of methods needed – 5 hits back blows – 5 chest compressions (till 1year) / abdominal thrusts over 1 year – Horisontal rib´s position – abdominal organs damage risk ANY QUESTIONS?