Formulation and Evaluation of Niosome
advertisement
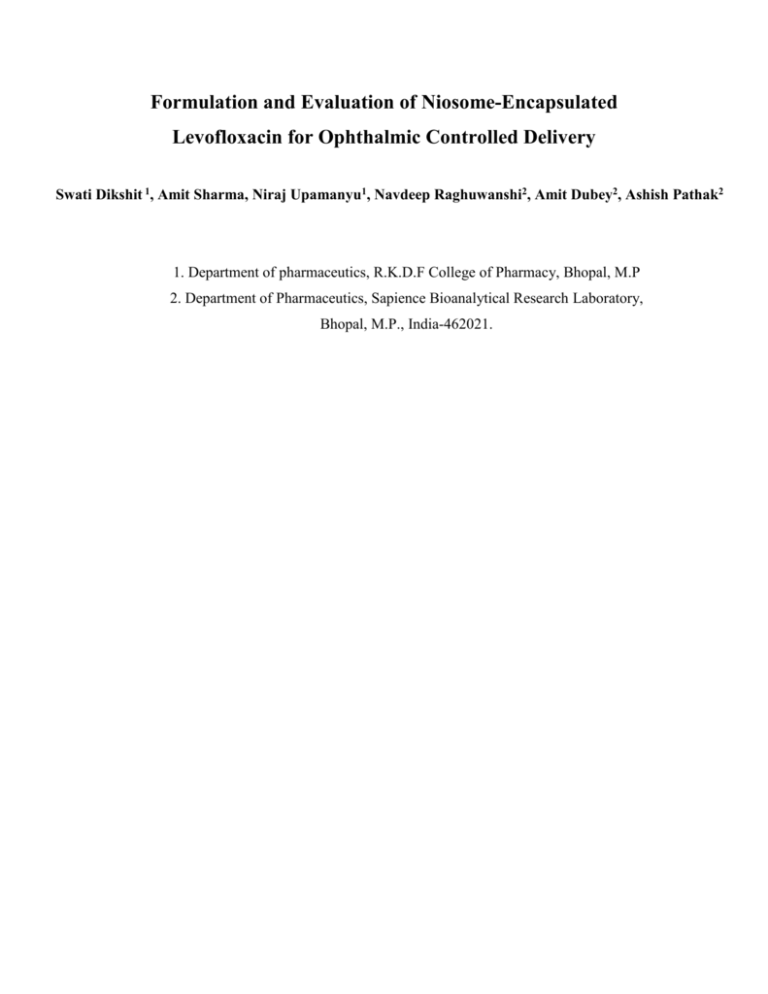
Formulation and Evaluation of Niosome-Encapsulated Levofloxacin for Ophthalmic Controlled Delivery Swati Dikshit 1, Amit Sharma, Niraj Upamanyu1, Navdeep Raghuwanshi2, Amit Dubey2, Ashish Pathak2 1. Department of pharmaceutics, R.K.D.F College of Pharmacy, Bhopal, M.P 2. Department of Pharmaceutics, Sapience Bioanalytical Research Laboratory, Bhopal, M.P., India-462021. Introduction: Drug delivery in ocular therapeutics is a challenging problem and is a subject of interest to scientists working in the multi-disciplinary areas pertaining to the eye, including chemical, biochemical, pharmaceutical, medical, clinical, and toxicological sciences[1] The current treatment of ocular infections requires frequent topical antimicrobial drug administration in microbial keratitis and repeated injection of antimicrobial drugs into the site of infection in endophthalmitis [2] . The therapeutics requires the association of more than one antimicrobial treatment for several weeks, which often leads to poor patient compliance, contributing to low therapy efciency[3]. Vesicular drug delivery systems allows the entrapment of drug molecule into lipid bilayer or surfactant vesicles and thus increase drug concentration at the site of application with sustained drug delivery of medicament, which results in improved bioavailability. Such vesicles (liposome and niosome) acts as carrier for controlled ocular drug delivery by preventing metabolism of drug from enzymes present at the corneal epithelial surface. Vesicle entrapped drug can be easily administered in liquid dosage forms such as eye drops with patient compliance, modulated drug release profile and high drug pay load. Niosomes can encapsulate both tear results in the rapid removal of the drug from eye lipophilic and hydrophilic drugs and protect against acidic and enzymatic effects in vivo. They offer several advantages over liposomes such as higher chemical stability, intrinsic skin penetration enhancing properties and lower costs.[4] Levofloxacin is a antibacterial agent of the fluoroquinolone class that exhibits a broad spectrum of in vitro activity. It has been demonstrated to be effective in the treatment of a wide range of community and hospital-associated infections.[5] This review presents a microbiological perspective of the use of levofloxacin for topical treatment of bacterial external ocular infections, presenting in vitro, pharmacokinetic and clinical trials data. Levofloxacin eye drops were launched in several European countries in 2002. The widespread use of levofloxacin in ophthalmology can be attributed to its appropriate antibacterial spectrum and good corneal penetration. The main indications for treatment are bacterial blepharitis and conjunctivitis, bacterial keratitis, especially when associated with contact lenses and endophthalmitis, where it is provided as an additional therapeutic agent. Furthermore, levofloxacin eye drops are used as prophylaxis to reduce the bacterial conjunctival flora prior to intraocular surgery. In a healthy eye the conjunctival bacterial flora primarily consists of Staphylococcus spp. (mainly S. epidermidis), Corynebacterium spp. and, to a lesser degree, Streptococcus spp. and various Gram-negative rods.[6] The predominant bacterial organisms isolated from patients with acute bacterial conjunctivitis are S. aureus, S. pneumoniae and Haemophilus influenzae, the latter being frequently recovered from children.[7,8] Material and Method: Levofloxacin was a gift sample from Renbaxy Labs, Devas, M.P, India, Cholesterol, Span 60 were gift sample from Zydus Cadila, Ahmdabad, Gujrat. Methanol, dihydrogen phosphate, disodium hydrogen phosphate were purchased from India Ltd, Mumbai. Preformulation study: [9] The FT-IR spectrum of pure drug was analyzed to check the purity of the drug using Bruker Fourier Transform Spectrophotometer by KBr pellet method. The IR absorption spectra of the pure drug were taken in the range of 400-4000-1 cm. FT-IR Graph reported in figure 1. Preparation of niosomes: [9-10] The composition of the tested niosomal formulae are reported in Table 1. Niosomes containing levofloxacin were prepared by thin film hydration technique. Briey, surfactants, cholesterol and DCP in different molar ratios, were accurately weighed in to along necked quick fit round-bottom fask and dissolved in 10ml chloroform. The organic solvent was slowly evaporated at 60°C under reduced pressure, using a rotary evaporator at 150 rpm such that a thin dry film of the components was formed on the inner wall of the rotating flask. The dried thin lipid film was then hydrated with 10ml of phosphate buffered saline (PBS, pH7.4), containing 10mg levofloxacin, by rotating the flask in a water bath using a rotavapor under normal pressure in order to ensure complete hydration of the film. The niosomal suspension was left to mature overnight at 4°C. For sterility, all the above mentioned steps were done under aseptic conditions. All glassware was sterilized by autoclaving, phosphate buffered saline was passed through a 0.22m membrane filter, and the entire procedure was carried out in a laminar flow hood. Microscopy [10] The vesicle formation by the particular procedure was confirmed by optical microscopy in 400x resolution. The niosome suspension placed over a glass slide and fixed over by drying at room temperature, the dry thin film of niosome suspension observed for the formation of vesicles. Entrapment efficiency The proportion of encapsulated levofloxacin was obtained by ultra-centrifugating 1ml of the niosomal suspension at 15,000rpm for 1h using a cooling centrifuge at 4°C (Remi, Mumbai, India). The niosomes were separated from the supernatant and were washed twice, each time with 1ml phosphate buffered saline, and recentrifuged again for 1h. The amount of entrapped levofloxacin was determined by lysis of the separated vesicles with isopropanol. A 100 µl sample of niosomes was mixed with 1ml of isopropanol, the volume was completed to 10ml with phosphate buffered saline and covered with para film to prevent evaporation. The concentration of the drug was determined spectrophotometrically (Systronic, model UV-1601 PC, Ahmedabad, India) after derivatization with o-phthaldialdehyde reagent by Zhang’s method [11] .Briey, the o- phthaldialdehyde reagent was formulated by adding 2.5g o-phthaldialdehyde, 62.5 ml methanol and 3ml 2-mercaptoethanol to 560 ml sodium borate solution, pH 8. There agent was stored in a brown bottle in dark chamber for atleast 24h before use, as it is light sensitive. This reagent could be used only upto 3days. Levofloxacin solution, ophthaldialdehyde reagent, and isopropanol (to avoid precipitation of the products formed) were mixed in similar proportions and stored for 30 min at room temperature. The ophthaldialdehyde reagent reacted with levofloxacin amino groups and chromophoric products were obtained, whose absorbance was measured at 298 nm. The entrapment efficiency is defined as follows [12]: Total Drug – Diffused Drug Percent of Entrapmet Efficiency = ---------------------------------------- × 100 Total Drug In-vitro drug release study [13] In vitro release pattern of niosomal suspension was carried out in dialysis bag method. 1.5 mg equivalent of 0.3 % of niosomal suspension was taken in dialysis bag (Hi media) and the bag was placed in a beaker containing 250 ml simulated tear fluid (pH7.4 phosphate buffer). The beaker was placed over magnetic stirrer and the temperature was maintained at 37º ± 1ºC. 5 ml samples were withdrawn periodically and were replaced by fresh buffer. The sink condition was maintained throughout the experiment. The withdrawn samples were analyzed for drug content using U.V. spectrophotometer at 294 nm keeping phosphate buffer pH 7.4 as blank. Ocular irritance test [14] The potential ocular irritation and/ or damaging effects of the niosomes under test were evaluated by observing them for any redness, inflammation (or) increased tear production. Formulation was tested on six rabbits by dispensing niosomes in the cul-desac of the left eye. Results and Discussion: Entrapment Efficiency %EE: The entrapment efficiencies of optimized niosomal formulations are reported in Table 2. In order to attain high levofloxacin encapsulation efficiency, several factors, including the type of surfactant, presence of PEO and the ratio of cholesterol added were evaluated and optimized. Due to entrapment efficiency we know that Span 20 is the better entrapped. So that span 20 was optimized for other tests. Characterization of Levofloxacin Niosomes Photomicroscopy and Transmission Electron Microscopy The formation of niosomal vesicles as well as their morphological aspects were evaluated by using photo and transmission electron microscopy. Various niosomal formulations were examined under optical microscope and photo-graphed at a magnication of ×40, by means of a fitted camera. Levofloxacin niosomal samples were also examined by transmission electron microscope at 70kV, after being negatively stained. A saturated ammonium molybdate aqueous solution was used as the staining agent. The images are shown in figure 3 & 4 respectively. In Vitro Release of Nimesulide from Niosomes niosomes prepared by lipid film hydration method. The comparative release data indicates that, NF1 is the better release in compare to NF2 and NF3. It is observed that the release was systemic and sustained action. All the data is shown in table no.3. Ocular Irritancy Test of Niosomes It was observed that over the study period (48 h) none of the tested formulae showed any signs of redness, inflammation or increased tear production. Thus it could concluded that the non ionic surfactants namely Span 20 [NF1], Span 60 [NF2], and Span 80 [NF3], used in the niosomal formulations as well as the other excipients were non-irritant to the eye. CONCLUSION The main objective of this study was to design suitable niosome-encapsulated drug delivery for ocular drug delivery on levofloxacin, to study the in vitro behaviour of the prepared system and ocular irritancy test in Albino rabbit eye. Finding of all this investigation conclusively demonstrate prolongation of drug release at a constant and controlled rate, after encapsulation of levofloxacin. This study suggests that niosomal formulation can provide consistent and prolonged release of levofloxacin from different niosomal formulations. It will lead to sustained action of the entrapped drug that reduce the side effects associated with frequent administration of the drug. Acknowledgement: The authors are thanks to Principal, R.K.D.F College of Pharmacy, Bhopal for providing facilities to carry out this work. Authors are also thanks to Diretor, Sapience Bioanalytical Reserch Laboratory and also thanks to Renbaxy Ltd., Devas for providing gift sample of levofloxacin, PEO and Ranchem Levoratory for providing Span 20, 60, 80. References: 1. Kaur IP, Garg A, Singla AK, Aggarwal D. Vesicular systems in ocular delivery: an overview. Int. J. Pharm. 2004;269:1–14. 2. Frucht-Pery J, Mechoulam H, Siganos CS, Ever-Hadani P, Shapiro M, Domb A. Iontophoresis–gentamicin delivery into the rabbit cornea, using a hydrogel delivery probe. Exp. Eye Res. 2004;78:745–749. 3. Blanco-Prieto MJ, Lecaroz C, Renedo MJ, Kunkova J, Gamazo C. In vitro evaluation of gentamicin released from microparticles. Int. J. Pharm. 2002;42: 203–206. 4. Prabhu P, Koland M, Vijaynarayan K, Harish NM, Ganesh D, Charyulu RN, Satynarayana D. Preparation And Evaluation Of Niosomes Of Brimonidine Tartrate As Ocular Drug Delivery System. J. of Pharmaceutical research and health care. 2002; 2(4):293-301. 5. Croom KF, Goa KL, Drugs, Levofloxacin: a review of its use in the treatment of bacterial infections in the United States. 2003;63(24):2769–2802. 6. Boltze HJ, et al., Klin Monatsbl Augenhlkd, 1990;9:498–9. 7. Seal DV, et al., Br J Ophthalmol, 1982;66:357–60. 8. Gigliotti F, et al., J Pediatr, 1981;98:531–6. 9. Blazek-Walsh AI, Rhodes DG. SEM imaging predicts quality of niosomes from maltodextrin-based proniosomes. Pharm. Res. 2001; 18: 656-661. 10. Carter KC, Dolan TF, Baillie AJ, MacColgan C. Visceral leishmaniasis: drug carrier system characteristics and the ability to clear parasites from the liver, spleen and bone marrow in Leishmania donovani infected BALB/c mice. J.Pharm. Pharmcol. 1989; 41(2): 87-91. 11. Zhang X, Wyss UP, Pichora D, Goosen MFA. Biodegradable controlled antibiotic release devices for osteomyelitis: optimization of release properties. J.Pharm. Pharmacol. 1994;46:718–24. 12. Guinedi AS, Mortada ND, Mansour S and Hathout RM. Int. J. Pharm. 2005;306:71-82. 13. Sankar V, Chandrasekaran AK. and Durga S, Formulation and evaluation of acyclofenac gels for ocular drug delivery,. Acta Pharmaceutica Sciencia, 2006; 48:5-10. 14. Tanwar Y. S., Patel D. and Sisodia S. S., In vitro and in vivo evaluation of ocular inserts of ofloxacin. DARU, 2007;15:139-145. Tables: Table I. Formulae Composition (Molar Ratio) Formula Composition Span 20 Span 60 Span 80 Cholesterol Dicetayl Phosphate F1 1 1 0.1 F2 1.5 1 0.1 F3 2 1 0.1 F4 1 1 0.1 F5 1.5 1 0.1 F6 2 1 0.1 F7 1 1 0.1 F8 1.5 1 0.1 F9 2 1 0.1 Table 2: Optimized of niosomal formulations Formulation Surfactant Drug:surfactant: Cholesterol Entrapment Efficiency %EE NF3 Span20 1:2:1 68.4 NF6 Span60 1:2:1 59.32 NF9 Span80 1:2:1 58.27 Table 3: Comparative In vitro dissolution profile of different formulations Time (hour) % of drug release NF3 NF6 NF9 0 0.00 0.00 0.00 1 13.36 12.05 09.48 2 19.75 18.68 13.06 3 26.67 24.34 23.80 4 35.21 28.72 28.13 5 42.13 38.40 36.12 6 49.36 47.63 44.23 8 54.36 51.54 48.35 10 62.36 61.38 59.58 12 76.57 73.08 71.56 Figure: Figure 1: FTIR of graph of Levofloxacin Figure 2. Drug release profile of levofloxacin Niosomes: Figure 3: Microscopic Image of levofloxacin Niosomes Fig 4. TEM of Levofloxacin Niosome