Many
advertisement
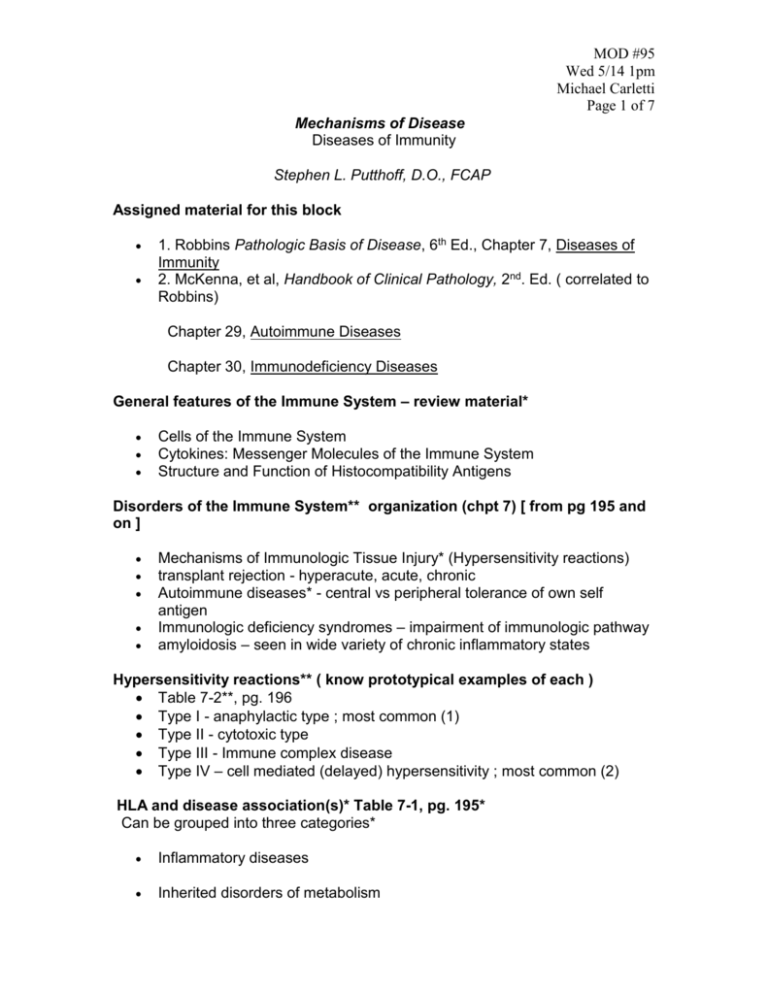
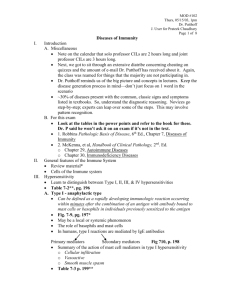
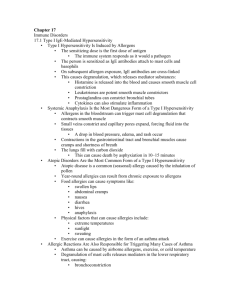
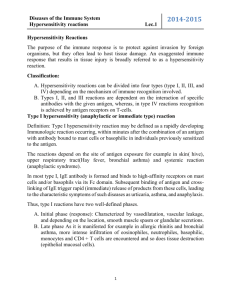
MOD #95 Wed 5/14 1pm Michael Carletti Page 1 of 7 Mechanisms of Disease Diseases of Immunity Stephen L. Putthoff, D.O., FCAP Assigned material for this block 1. Robbins Pathologic Basis of Disease, 6th Ed., Chapter 7, Diseases of Immunity 2. McKenna, et al, Handbook of Clinical Pathology, 2nd. Ed. ( correlated to Robbins) Chapter 29, Autoimmune Diseases Chapter 30, Immunodeficiency Diseases General features of the Immune System – review material* Cells of the Immune System Cytokines: Messenger Molecules of the Immune System Structure and Function of Histocompatibility Antigens Disorders of the Immune System** organization (chpt 7) [ from pg 195 and on ] Mechanisms of Immunologic Tissue Injury* (Hypersensitivity reactions) transplant rejection - hyperacute, acute, chronic Autoimmune diseases* - central vs peripheral tolerance of own self antigen Immunologic deficiency syndromes – impairment of immunologic pathway amyloidosis – seen in wide variety of chronic inflammatory states Hypersensitivity reactions** ( know prototypical examples of each ) Table 7-2**, pg. 196 Type I - anaphylactic type ; most common (1) Type II - cytotoxic type Type III - Immune complex disease Type IV – cell mediated (delayed) hypersensitivity ; most common (2) HLA and disease association(s)* Table 7-1, pg. 195* Can be grouped into three categories* Inflammatory diseases Inherited disorders of metabolism Wed 5/14 1pm Page 2 of 7 Autoimmune diseases (criteria must be met, best examples systemic lupus erythematosus and autoimmune hemolytic anemia Role of HLA class II molecules HLA B27 is correlated to ankylosing spondylitis involves lower lumbar spine where there is chronic inflammatory reactions can progress to other musculoskeletal structures Type I hypersensitivity (anaphylactic type) Can be defined as a rapidly developing immunologic reaction occurring within minutes after the combination of an antigen with antibody bound to mast cells or basophils in individuals previously sensitized to the antigen Fig. 7-9, pg. 197* of bronchial epithelium (airway) – fixation of IgG antibodies to mast cells, the antibody is really IgE and is fixed by the Fc portion to the mast cell; when other antigens attach to the Fab portion they degranulate the mast cell May be a local or systemic phenomenon – systemic is more important due to fear of shock due to lack of profusion of vital organs and increased vascular permability after a reaction to an antigen to which you have been exposed to previously The role of basophils (circulating in white blood cells) and mast cells ( found in tissue and is fixed version of basophils) In humans, type I reactions are mediated by IgE antibodies – Fig 7.10 pg 198 Primary (histamine and proteases) and secondary (leukotrienes and prostaglandins) mediators – to treat allergies they give antihistamines Summary of the action of mast cell mediators in type I hypersensitivity – Table 7-3 pg 199 Cellular infiltration Vasoactive Smooth muscle spasm Two major reactions in this degranulation is tissue edema due to vascular dilatation and loss of fluid into interstitial space; with this you hear wheezing with a stethoscope Wed 5/14 1pm Page 3 of 7 Type II hypersensitivity (cytotoxic type) [ damage is done on site] Mediated by antibodies directed toward antigens present on the surface of cells or other tissue components Complement –dependent reactions : to produce injury antibody-antigen complex activates the complement system; by itself it is not pathogenic, however: example is of autoimmune hemolytic anemia – target cell is RBC Antibody-dependent cell mediated cytotoxicity : example is ADCC Antibody mediated cellular dysfunction : example myasthenia gravis affecting motor end plate in which there are antibodies against acetylcholine recptors and block them; end up with lack of ability of muscle to contract; early manifestation is droopy eyelids Type III hypersensitivity (immune complex mediated) – Table 7-5 pg 201 [ damage depends on where things are deposited ] Old term = serum sickness is induced by antigen-antibody complexes that produce tissue damage as a result of their capacity to activate the complement system Two types of antigens exogenous* - pathogens and some drugs and injected substances (due to their contaminants that cause immunologic reactions); will endocarditis of drug abusers endogenous** - most important is systemic lupus; another is rheumatoid arthritis which the antigen is an antibody Systemic immune complex dz – 3 phases - Formation of Ag-Aby complexes in the circulation - Deposition of the immune complexes in various tissues, thus - Initiation of an inflammatory reaction in dispersed sites throughout the body platelet aggregation – any disorder of platelets; most studied by bleeding time most often ends in necrosis Wed 5/14 1pm Page 4 of 7 look over complement pathway – MAC the inflammatory complement mediators Type III hypersensitivity (immune complex mediated) – systemic, usually The ultimate result is vascular injury Blood vessels = vasculitis Glomeruli = glomerulonephritis, but doesn’t always mean inflammatory or infectious Joint surfaces = arthritis, mostly rheumatoid in which an IgG is directed against IgM called leukocytoclastic vascultits indicating multiple inflammatory cells, necrosis and don’t know what the inciting agent is, until it is diagnosed Type III hypersensitivity (immune complex mediated) - local Arthus reaction – [def] a local area of tissue necrosis resulting from acute immune complex vasculitis, typically in the skin ; not used anymore – they use purified protein derivative (PPD) Type IV hypersensitivity (cell mediated not so much humoral, therefore T cell)** The cell mediated type of hypersensitivity is initiated by specifically sensitized T lymphocytes. It includes the classic delayed-type hypersensitivity reactions initiated by CD4 T cells and direct cell cytotoxicity mediated by CD8 T cells. It is the principal pattern of immunologic response not only to a variety of intracelluar microbiologic agents, particularly Mycobacterium tuberculosis, but also to many viruses, fungi, protozoa and parasites. So-called contact skin sensitivity to chemical agents and graft rejection are other instances of cell-mediated reactions. Delayed-type (classic example) – tuberculin reaction ; not used anymore – they use purified protein derivative (PPD) granulomatous inflammation is often characteristic of Type IV hypersensitivity- differs from lymphoid follicle which is composed of B lymphocytes in the center and T lymphocytes surrounding – found in TB, sarcoidosis, fungal diseases T cell-mediated cytotoxicity CTLs (cytotoxic T lymphocytes) Wed 5/14 1pm Page 5 of 7 A variety of roles antigen presenting cell is normally a macrophage transplant rejection Appears to involve several of the hypersensitivity reactions Rejection is a complex process in which both cell mediated immunity and circulating antibodies play a role T cell mediated reactions Antibody mediated reactions morphology - hyperacute - acute - chronic note schematics and photomicrographs pg 208,209 Autoimmune diseases [def] pathologic immunity (3 criteria) Table 7-6** pg 211 look at single organ / single cell type / systemic ones The autoimmune diseases form a spectrum - autoantibodies specifically directed against B cells in the pancreatic islets (ID DMI) - antibodies directed against components of glomerular and alveolar septal basement membranes cause injury and disease in those specific organs) - a diversity of antibodies directed against DNA, platelets, red cells and protein-phospholipids complexes resulting in lesions ubiquitous throughout the body (SLE) Immunologic tolerance ( know how they go wrong ) Wed 5/14 1pm Page 6 of 7 - Central tolerance - Peripheral tolerance Mechanisms of autoimmune diseases -it is clear that there are a number of ways by which tolerance can be bypassed, thus terminating a previously unresponsive state to autoantigens pp. 214 – 215, esp. genetic factors Systemic lupus erythematosus ( SLE ) [wolf like facies around eyes and cheeks] The classic prototype of the multisystem disease of autoimmune origin, characterized by a bewildering array of autoantibodies, particularly antinuclear antibodies (ANAs) Acute or insidious in its onset, it is a chronic, remitting and relapsing, often febrile illness characterized principally by injury to the skin, joints, kidney and serosal membranes. However, virtually any and possibly every other organ in the body may also be affected Table 7-7, pg. 217* clinical manifestations: fluid from cavities lined by mesothelial cells causing plural effusions, pericarditis (virtually every body cavity) Prevalence gender predilection – more common in women ethnic predilection Etiology and pathogenesis -ANAs can be grouped into (4) categories* -Know the patterns of nuclear immunofluorescence -Which antibodies (2) are virtually diagnostic of SLE? (anti-DNA, anti-Sm) See Table 7-8**pg 218 and group by antibody system know the ones in boxes ; these are just clinical correlations so don’t just do an ANA unless you suspect the disease, and don’t just diagnose based on the ANA pattern genetic factors Wed 5/14 1pm Page 7 of 7 nongenetic factors immunologic factors Morphology -Table 7-9, pg. 220* -Summary of disease, pg. 220* Clinical course (what are the most common causes of death due to SLE?) Chronic discoid lupus erythematosus Subacute cutaneous LE Drug-induced LE