File
advertisement

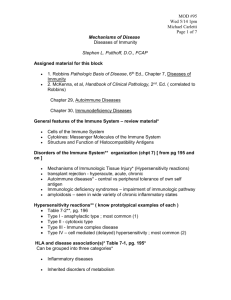
Immunopathology • Hypersensitivity • Autoimmunity • Immunodeficiency • Primary • Secondary Hypersensitivity • In hypersensitivity, the antigens are not destructive, but the responses to them cause tissue damage • 4 types (1-4) • Antigen can be exogenous or endogenous (self) Type I • IG-E mediated response. • Requires repeated exposure to allergen • Immediate and late responses (both mediated by mast cells) • Immediate (30mins – 1hr): vasoactive amines, lipid mediators • Late phase response (2hr-24hrs): mediated by cytokines and includes: • Eosinophils • Basophils • TH2 activation Type I • Localized • Asthma, urticaria, allergic rhinitis. • Systemic • Anaphylaxis • • • • • Systemic vascular dialation and leakage w/ drop in BP. Edema drop in BP (loss of fluid) Bronchial constriction (mediated by LTC4/D4/E4) Runny nose, wheezing, swelling, coughing, sneezing, itching, vomiting. Key players? • Mast cells, IG-E antibody, inflammatory mediators secreted by mast cells. Type 1: predisposition • Atopy = a predisposition to develop localized immediate hypersensitivity reactions to inhaled and ingested antigens • Atopic individuals tend to have: • High serum Ig-E • More IL-4-producing TH2 cells • 50% of patients have a family history of allergies Type II- antibody mediated • Antibody mediated reaction. IG-G/M bound to cells in our bodies opsinize cells for phagocytosis by MQs. We start initiating an immune response against our own cells and therefore destroy our tissues. • Side effects of drugs (penicillin), transfusion (you’re getting antibodies that will target your cells and initiate an immune response against them). • Erthyroblastosis fetalis • Autoimmune hemolytic anemia, thrombocytopenia. • Pernicious anemia (IF). Type III- Antibody-Antigen complex • • • • • • • • Mediated by antigen-antibody complex deposits in tissues. The recruited neutrophils and monocytes cause tissue damage. Local response is called arthus reaction (cutaneous vasculitis) Systemic reaction is known as serum sickness 3 phase: Phase 1 Immune complex formation Phase 2 immune complex deposition Phase 3 immune complex mediated inflammation and tissue damage. Examples: Rx to penicillin most common cause of serum sickness in US. Use of horse serum from immunized horses for immunization against diptheria. Type IV- delayed type • Cell mediated and not antibody mediated!! • Take 2-3 days to develop • CD4 TH1 cells and sometimes CD8 T cells respond to the tissue antigens by secreting cytokines that stimulate inflammation and activate phagocytes. • Delayed type hypersensitivity: • PPD skin test for TB • Insect venom. • Contact hypersensitivity: • Small molecules like Nickel and poison Ivy. Autoimmune Diseases • Chronic diseases caused by immune responses directed toward autologous (self) components of the body. • Involves loss of self tolerance. • More common in females than males…Ratio of 9-10:1 • Except for ankylosing spondylitis (More common in males) • Classically affects women of childbearing age • Type II Autoimmune response: autoimmune hemolytic anemia. • Type III autoimmune response: Lupus. • Clinically progressive with relapse and remissions. Lupus • Chronic, systemic autoimmune disease. • Flares and remissions are common. • An example of type III HSR (antibody-antigen complex deposits damage tissues). • Autoantibodies to cell surface/cytoplasm/nucleus (nucleic acids and nucleoprotein particles). • Almost any tissue can be involved. Lupus • • • • • • • Classical signs/symptoms: Malar “butterfly” rash/ discoid rash, especially upon exposure to sunlight. Stiff fingers and hips in morning Associated with low complement. High blood ANA titer 1:1280 (Highly sensitive). Anti dsDNA antibodies (Highly specific) Antibody-antigen complexes can be deposited in kidneys and joints (small vessels) resulting in glomerulonephritis and arthritis respectively. • Management: corticosteroids to suppress the immune response. Rheumatoid arthritis • Chronic, systemic autoimmune disease. • An example of type IV HSR- cell mediated. • More common in women • Rheumatoid factor (Ig-M antibody against the Fc region of Ig-G; marker of tissue damage and disease). Present in 80% of patients with Lupus. • Progressive destruction of cartilage and bone. • Symmetric involvement of joints; TMJ in 50-60% • Occurs with other autoimmune diseases. Rheumatoid arthritis • White blood cells infiltrate into the synovium : CD4/8, B cells, neutrophils, macrophages. All together mediate damage. • Autoimmune CD4 get activated by dendritic cells, which then activate macrophages, which accumulate in synovium. • Pro inflammatory mediators and proteinases and collagenases produced by activated cells destroy tissue in joints. Graves’ Disease • Heat intolerance, nervousness, irritability, weight loss. • Thyroid enlargment. • Autoimmune? Antibody production that bind to TSH receptors… • CD4 TH2 response. • Tx: Drugs that inhibit thyroid function, thyrodectomy. Hashimoto’s • Can’t make thyroid hormone. • CD4 TH1 response: both antibodies and effector T cells for thyroid antigens produced. • Lymphocytes infiltrate and we get progressive destruction of normal thyroid tissue. • Hypothyroidism. • Tx: replacement therapy. Type 1 DM • Selective destruction of insulin producing cells in pancreas : islets of Langerhans • Antibody and T-cell responses against insulin, glutamic acid decarboxylase, and other specialized proteins of the pancreatic β cell. • CD8 T cells mediate β-cell destruction, gradually decreasing the number of insulin-secreting cells. Individual islets become successively infiltrated with lymphocytes. • Disease begins when there are insufficient β cells to provide the insulin necessary to control the level of blood glucose Autoimmunity and infections: Rheumatic fever • Infection with S. pyogenes • Same antibodies made against S. Pyogenes react to epitopes present on human heart, joint, and kidney. • When bind to self tissue activate complement and generate acute inflammation Rheumatic fever Immunodeficiencies • Primary: – Most are congenital – Most are inherited – Often significant family history – Can present initially in children and adults – Some are combined with other congenital defects • Secondary: – Induced by environmental, infectious or iatrogenic factors – Common factors: malnutrition, HIV infection, radiation, chemotherapy, cancer. Primary immunodeficiency • Most are genetically determined. • Most common is IgA deficiency. • Blood cell count with differential is #1 for the diagnosis of primaries. • Therapy and prophylaxis always require anti microbial. • Other TX: specific for disease, may include: replacement of immunoglobins, or stem cell transplantation. Primary • X-Linked Agammaglobulinemia (Bruton's Agammaglobulinemia) • Common variable immunodeficiency • Isolated IgA Deficiency • Hyper-IgM Syndrome • DiGeorge Syndrome (Thymic Hypoplasia) • Severe Combined Immunodeficiency • Deficiencies in Phagocytosis Leukocyte adhesion deficiency Missing integrins, cant migrate into tissues. Can’t clear infections persistent periodontal/gingival infection. Neutropenia Drugs: Anti-cancer chemotherapeutic agents, antibiotics, other Infections: Viral hepatitis A and B, rubella, measles, varicella, HIV, typhoid, TB, etc. Destruction of bone marrow by malignancies Chronic Granulomatous Disease • Phagocytes cannot produce superoxide radical (lack NADPH oxidase which converts oxygen to superoxide anion). • Chronic infections with granuloma formation • Bacterial infections; fungal infections; foreign body (non-infectious); hypersensitivity reactions Secondary Immunodeficiencies • Environmental • Malnutrition, radiation • Infections • Human immunodeficiency virus (HIV), other microorganisms • Iatrogenic • Chemotherapeutic agents, immunosuppressive drugs, radiation therapy • Tissues Very Sensitive to Ionizing Radiation: any cells that undergo a lot of cell divisions. AIDS • Esophageal candidiasis (bronchi, trachea or lungs) • Deep fungal infections: Coccidioidomycosis, • Cryptococcosis, Cryptosporidiosis • Cytomegalovirus disease • HSV longer than 1 month • Kaposi’s sarcoma (HHV-8 associated) (<60yrs) • Lymphoma (B Cell - EBV associated) Immunodeficiency Secondary to HIV: Mechanisms • Infected cells: • Receptor: CD4, co-receptors: CCR5, CXCR4 • Clinical latency: Active viral replication in lymphoid tissue, spreading from cell to cell • How do you measure? CD4+ lymphocyte counts, viral load, activation markers on CD8+ T cells • Persistent T cell activation leads to increased depletion rates • Depletion of naive T cell pool (thymus involution after puberty) DM • Accumulation of glycosylation products in vessel walls • T cell function is depressed • Neutrophil function is depressed • Adherence, chemotaxis, phagocytosis, anti-oxidant activity • Oral problems: accelerated periodontal disease, poor healing, candidiasis • Zygomycosis (rhizopus) in diabetic patient with ketoacidosis AKA Mucormycosis Iatrogenic Cause of Immunodeficiency Immunosuppressive Drugs • Organ transplantation • Cyclosporin: blocks (NFAT), which is required for transcription of cytokine genes (IL-2)- Blocks T –CELL activatio! • Tacrolimus – Inhibits IL-2 and therefore blocks T-cell activation • Azathioprine: Inhibits leukocyte development from bone marrow precursors), • Corticosteroids Block inflammation by blocking NFKB and therefore cytokine production. • Rapamycin and mycophenolate: Inhibit lymphocyte proliferation • Cancer chemotherapy • affects dividing cells in marrow • Corticosteroids • Inhibits leukocyte infiltration at the site of inflammation • Suppresses humoral immune responses • Affects mediators of inflammation such as prostaglandins and leukotrienes