Immunity Vivas - WordPress.com
advertisement

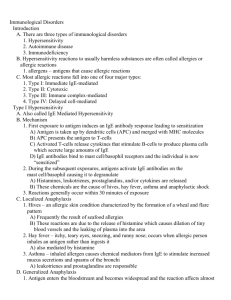
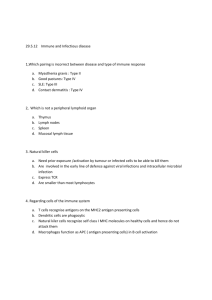
IMMUNITY VIVAS 2010-2, 2009-2, 2007-2 What are the features of Type 1 hypersensitivity? - Rapid immunologic reaction (within 5 – 30 minutes after exposure to the antigen) - Previously sensitised individuals - IgE mediated -> immediate release of vasoactive amines and other mediators by - Mast cells (and or basophils involved), later recruitment of inflammatory cells - Immediate response characterized by vasodilation, increased vascular permeability, bronchial SMC contraction, glandular secretions – typically resolves within 60 minutes - Late phase reaction (2-24h, lasting days) – inflammatory infiltrates and tissue damage driven by activated macrophages via lipid mediators and cytokines - TH2 cells play an important role in initiation and propagation by stimulating IgE production What are the actions of mast cell mediators in Type I Hypersensitivity (and give examples)? Mediators Preformed and stored in secretatory mast cell granules (vesicles) - Biogenic amines: Histamine, other amines -> bronchial SMC contraction, vascular permeability and dilation, glandular secretions - Enzymes – neutral proteases (chymase, tryptase) -> tissue damage and generate kinins and active complement - Proteoglycans (heparin and chondroitin suphate) – involved in packaging of the amines Produced by the activated macrophages Lipid mediators (released from mast cell membrane by phospholipase A2) - Leukotriene B4 - highly chemotactic for neutrophils, eosiniphils and monocytes - Leukotrienes C4, D4 – most potent vasoactive and spasmogenic substances known - Prostaglandins, - PAF – platelet aggregation, histamine release, bronchospasm, vascular permeability and dilation Cytokines (TNF, IL-1) Summary: Vasoactive effects – Hist, PAF, Leukotrienes C4 and D4, PG Smooth muscle spasm – Hist, PAF, Leukotrienes C4 and D4, PG Cellular infiltration – PAF, Leukotrienes B4, Cytokines What is the late phase reaction? Ongoing inflammatory reaction without additional exposure to triggering antigen. The late phase reaction is characterized by infiltration of the tissues with eosinophils, neutrophils, basophils, monocytes, and CD4+ T cells as well as tissue destruction, typically in the form of mucosal epithelial cell damage. The recruited cells amplify and sustain the inflammatory response, without additional exposure to the antigen. Time course 2-24 hours later without additional exposure – may last for days List some agents that can cause type 1 hypersensitivity 2007-2 Drugs (especially penicillins), Foreign proteins (antisera), Foods (peanuts, shellfish, egg proteins), Insect stings (Bee stings), Pollens Additional: What characterises anaphylaxis Vascular shock, widespread oedema and difficulty breathing (bronchospasm) 2010-2, 2010-1, 2008-2, 2005-2 What is type 2 hypersensitivity? Type 2 hypersensitivity is mediated by antibodies directed toward antigens present on the surface of cells or other tissue components (e.g. ECM). Antigens can be intrinsic to the membrane or matrix or exogenous (e.g. a drug metabolite) Describe the different types of type 2 hypersensitivity reactions and give examples of each Three types (A) Opsonisation and Phagocytosis - Complement and Fc Receptor Mediated - IgG and IgM activate complement, C3b (& C4b) recognised by phagocytes -> phagocytosis Probably lesser or unknown role in hypersensitivity: - Activates complement system & membrane attack complex causing lysis of cells (need thin wall) - Ab dependent cellular cytotoxicity (ADCC) Mono, Macro, Neut, Eosin, NK (unknown role) - Examples: 1. Transfusion reactions 2. Haemolytic disease of the new born (erythroblastosis foetalis) 3. Auto immune haemolytic anaemia, agranulocytosis, thrombocytopaenia 4. Certain drug reactions (B) Inflammation - Complement and Fc Receptor Mediated - Deposition of antibodies in tissues activating complement causing inflammation - C5a (& C3a) stimulate Neutrophil and Monocyte attack via Fc receptors releasing enzymes and Oxygen free radicals - Examples: 1. Vascular Organ graft rejection and vasculitis by ANCA 2. Goodpastures (BM of glomeruli and lung) -> nephritis and lung haemorrage 3. Acute rheumatic fever (step cell wall/cross reactivity w/ myocardial antigen) (C) Cellular Dysfunction - Antibody Mediated - Antireceptor antibodies disturb the normal function of receptors without causing cell injury or inflammation - Examples: 1. Myasthenia gravis (ACh receptor antibodies) 2. Graves Disease (TSH receptor) 3. Type II (insulin resistant) diabetes 4. Pernicious anaemia (Intrinsic factor of gastric parietal cell neutralization) 2008-2, 2005-2, 2003-2, 2003-1 What is the pathogenesis of type III hypersensitivity? Antibodies bind antigens & then these complexes induce inflammation at a remote location directly or by activating complement. The recruited leukocytes produce tissue damage by release of lysosomal enzymes and generation of toxic free radicals. The antigens involved may be exogenous or endogenous, and the effects may be systemic or localized. 3 phases (systemic diseases) 1. Formation of antigen-antibody complexes in circulation (typically ~ 1week after introduction) 2. Deposition of immune complexes in various tissues 3. Inflammatory reaction at the site of deposition (~10 days after antigen introduction) - By complement activation which damages directly and leads to recruited inflammatory cells (neutrophils) producing lysozomal enzymes and toxic free radicals What are the common sites for immune complex deposition? - Medium size complexes most pathogenic - Organs where blood is filtered at high pressures to form other fluids are effected, e.g. urine and synovial fluid. Thus: renal glomeruli and joints - Also: skin, heart, serosal surfaces, small blood vessels Give some examples of diseases caused by Type III hypersensitivity - SLE: Nuclear antigens -> nephritis, skin lesions, arthritis and others - Polyarteritis nodosa: Viral (Hep B) antigens -> systemic vasculitis - Post strep GN: Step cell wall antigens -> nephritis - Acute GN - Reactive arthritis: Bacterial antigens - Serum sickness: Various proteins -> arthritis, vaculitis, nephritis - Arthus reaction: from various proteins -> localized area of tissue necrosis, cutenous vasculitis What is the role of complement in systemic immune complex disease 2003-1 1. Opsonisation (C3b -> phagocytosis) 2. Chemotaxis (C5a) 3. Anaphylotoxins (C3a & C5a) 4. Membrane Attack Complexes (C5b binds C6-9) 2007-2 What is type IV hypersensitivity T cell mediated (type IV) hypersensitivity is initiated by specifically sensitised T lymphocytes. It includes the classic delayed type of hypersentivity reactions by CD4+ (TH1) cells and the direct cell mediated cytotoxicity mediated by CD8+ (CTL) cells What is a delayed type of hypersensitivity reaction - Tissue antigen recognized by CD4+ (TH1) cells - Secrete cytokines (INF-, TNF-, IL-1 and IL-12) - Activation of macrophages (amplify the TH1 response) - Inflammation and tissue damage - Accumulation of mononuclear cells around small veins and venules (perivascular cuffing) - Increased microvascular permeability: escape of plasma proteins and fibrin into interstitium - Response will start 8-12 hours and take 24-72 hours to peak (delayed) What is T-cell mediated cytotoxicity 2007-2 Principal pattern of response to many viral infections and tumour cells. CTL also contribute to allograft rejection. CTL induced injury is mediated by perforin-granzyme and Fas-FasL pathways that ultimately induce apoptosis 2011-2 What diseases are caused by Type 4 hypersensitivity - Type 1 Diabetes: antigens of pancreatic islet cells (Insulin, glutamic acid decarboxylase) - Rheumatoid arthritis: Unknown antigen of joint synovium - Multiple sclerosis: Myelin basic protein, Proteolipid protein - Crohn disease: ?commensal bacteria - Periph neropathy (?GBS): protein Ag of periph nerve myelin - Contact dermatitis environmental, e.g. poison ivy Describe the Tuberculin reaction 2011-2 - Classic DTH response - Intracutaneous injection of purified protein deriviative (PPD) from tubercle bacillus - Prior TB infection -> PPD responsive CD4+ cells - Histologically there is perivascular mononuclear cell infiltrate (perivascular cuffing) - Also endothelial hypertrophy How does it differ in a naïve individual 2009-1 In naïve individual, CD4+T cells differentiate into TH 1cells after recognising antigen presented on APCs in association with class II MHC molecules. TH1cells can enter the circulation and remain in the memory pool of T cells for long periods (years) 2003-2 What are the major pathological sequelae of HIV infection? Attacks CD4+ T cells -> profound immunosuppression -> opportunistic infections, neoplasms, neurologic manifestations. T-cell loss via - Direct cytopathic effects mostly - Destruction of lymphoid organs (the cytokine environment for maturation of CD4+ T cells) - Chronic activation of uninfected cells -> activation-induced death - Fusion of infected and non-infected cells - Soluble gp120 protein -> unifected cell T-cell death via CTL or apoptosis - Also qualitative defects w/ reduced TH1 >TH2 responses Opportunistic infections - Majority of deaths - Mostly via reactivation rather than de novo - Pneumocytis jiroveci, candida, CMV, TB, Cryptococcus, Toxoplasma gondii, HSV and more CNS (40-60% of patients) - Infection via monocytes - Damage via toxic cytokines (IL-1 and TNF), neuronal NO, or via gp120 - Most common is AIDS-dementia complex, a progressive encephalopathy - Also: aseptic meningitis, peripheral neuropathy, CNS infections and neoplasms Neoplasms - Kaposi sarcoma is most common due to KS hepesvirus - Non-Hodgkin B Lymphoma and others What are the modes of transmission of HIV? 1. Sexual contact (75%) , heterosexual globally more common; female partners of IVDUs. Female to male 1/20th as efficient in US, more in Thailand. Abetted by STDs. 2. Parenteral: IVDUs major, blood products almost eliminated. Needle-stick 0.3%, reduced 8-fold by prophylactic treatment with retrovirals 3. Vertical, i.e. Mother-to-infant in utero, at delivery, in breastmilk. 7-49%. Not by insect bites. 2003-1 Where are B lymphocytes located 1. Bone Marrow 2. Circulating 3. Lymph nodes (follicles) 4. Spleen (follicles) 5. Peripheral Lymphoid Tissue How do B cells respond to antigenic stimulation 1. Specific Receptor Complex (IgM) 2. Transformation to Plasma Cell 3. Production of Specific immunoglobulins How are B cells activated in a graft vs host reaction 1. (CD4+) T helper (TH2) cells 2. Cytokines (Interleukin 4&5) 3. B cell stimulated by antigen in presence of cytokines Graft rejection - Host immune system triggered by HLA histo-incompatibility Host T cells by 2 pathways: - Direct via donor APC (dendritic cells): recognize donor HLA and CD8+ -> CTL and CD4+ -> TH1 - Indirect via host APC: usual response of delayed type hypersensitivity via CD4+ T cells Hyperacute rejection - Occurs if previously sensitised (repeat transfusions) - Via complements and ADCC Acute rejection (days – months) - Acute cellular: via macrophages, CD4+ and CD8+ T cells - Acute humoral (rejection vasculitis): via newly synthesised anti-donor antibodies Chronic rejection (months – years), is improved by - HLA matching - Immunosuppresion (blocks T cell activation) - T cell antibodies - Plasmapheresis or anti-B cell therapy