Mech102-DiseasesOfImmunityContinued
advertisement

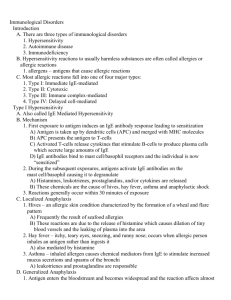
MOD #102 Thurs, 05/15/03, 1pm Dr. Putthoff J. Uxer for Prateek Chaudhary Page 1 of 8 I. II. III. Diseases of Immunity Introduction A. Miscellaneous Note on the calendar that solo professor CILs are 2 hours long and joint professor CILs are 3 hours long. Next, we got to sit through an extensive diatribe concerning cheating on quizzes and the amount of e-mail Dr. Putthoff has received about it. Again, the class was reamed for things that the majority are not participating in. Dr. Putthoff reminds us of the big picture and concepts in lectures. Keep the disease generation process in mind—don’t just focus on 1 word in the scenario ~30% of diseases present with the common, classic signs and symptoms listed in textbooks. So, understand the diagnostic reasoning. Novices go step-by-step; experts can leap over some of the steps. This may involve pattern recognition. B. For this exam Look at the tables in the power points and refer to the book for these. Dr. P said he won’t ask it on an exam if it’s not in the text. 1. Robbins Pathologic Basis of Disease, 6th Ed., Chapter 7, Diseases of Immunity 2. McKenna, et al, Handbook of Clinical Pathology, 2nd. Ed. o Chapter 29, Autoimmune Diseases o Chapter 30, Immunodeficiency Diseases General features of the Immune System Review material* Cells of the Immune system Hypersensitivity Learn to distinguish between Type I, II, III, & IV hypersensitivities Table 7-2**, pg. 196 A. Type I - anaphylactic type Can be defined as a rapidly developing immunologic reaction occurring within minutes after the combination of an antigen with antibody bound to mast cells or basophils in individuals previously sensitized to the antigen Fig. 7-9, pg. 197* May be a local or systemic phenomenon The role of basophils and mast cells In humans, type I reactions are mediated by IgE antibodies Primary mediators Secondary mediators Fig 710, p. 198 Summary of the action of mast cell mediators in type I hypersensitivity o Cellular infiltration o Vasoactive o Smooth muscle spasm Table 7-3 p. 199** MOD #102 Thurs, 05/15/03, 1pm Dr. Putthoff J. Uxer for Prateek Chaudhary Page 2 of 8 The thought is that histamine is a major factor in Type I reactions. Histamine causes vasodilation, increased vascular permeability leading to edema, and smooth muscle spasm. Learning that leukotrienes are just as important in Type I reactions as histamine is. Do people die of asthma? Yes. (also die from epilepsy, typically in their sleep) Histamine: stimulate kinins, C3a pg. 72 Note Fig. 3-18, pg. 71 proteoglycans B. Type II - cytotoxic type Mediated by antibodies directed toward antigens present on the surface of cells or other tissue components o Complement –dependent reactions o Antibody-dependent cell mediated cytotoxicity o Antibody mediated cellular dysfunction Figures are in the next 3 slides but were not discussed in class. C. Type III - Immune complex disease Mysthenia gravis Old term = serum sickness is induced by antigen-antibody complexes that produce tissue damage as a result of their capacity to activate the complement system Two types of antigens o exogenous* o endogenous** Table 7-5, p. 201* Systemic immune complex dz – 3 phase Formation of Ag-Aby complexes in the circulation Deposition of the immune complexes in various tissues, thus MOD #102 Thurs, 05/15/03, 1pm Dr. Putthoff J. Uxer for Prateek Chaudhary Page 3 of 8 Initiation of an inflammatory reaction in dispersed sites throughout the body Again, more slides of pictures that were not discussed. The ultimate result is vascular injury o Blood vessels = vasculitis o Glomeruli = glomerulonephritis o Joint surfaces = arthritis o 2 things can happen: the intima and smooth muscle are left intact and you see inflammatory cells streaming through as below. Or, the intima and smooth muscle can be destroyed and there is a fibrinoid appearance—this is the hallmark of immune injury. Arthus reaction – [def] a local area of tissue necrosis resulting from acute immune complex vasculitis, typically in the skin D. Type IV – cell mediated (delayed) hypersensitivity** Granulomas are characteristic of Type IV hypersensitivity. They must meet 3 criteria: 1. space occupying 2. made of epitheliod cells, histioid cells—activated macrophages 3. not around blood vessels (if they are, it’s vascultis) You don’t have to see giant cells Mycobacteria infection (TB)—see caeseating or necrotizing granuloma Sarcoidosis—no central necrosis or caeseation Fungi infection—angioinvasive fungi—opportunistic. Aspergillus The cell mediated type of hypersensitivity is initiated by specifically sensitized T lymphocytes. It includes the classic delayed-type hypersensitivity reactions initiated by CD4 T cells and direct cell cytotoxicity mediated by CD8 T cells. It is the principal pattern of immunologic response not only to a variety of intracelluar microbiologic agents, particularly Mycobacterium tuberculosis, but also to many viruses, fungi, protozoa and parasites. So-called contact skin sensitivity to chemical agents and graft rejection are other instances of cell-mediated reactions. Delayed-type (classic example) – tuberculin reaction granulomatous inflammation is often characteristic of Type IV hypersensitivity—look at the power points for the histo slide T cell-mediated cytotoxicity CTLs (cytotoxic T lymphocytes) have a variety of roles KNOW WHAT TYPE OF HYPERSENSITIVITY HEMOLYTIC ANEMIA REPRESENTS!!! (1st subtype [complement-dependent] of Type II) IV. Transplant rejection Transplants are done at most major referral hospitals Graft vs Host reaction o In bone marrow transplantations, 1st the marrow is irradiated to kill the neoplastic cells. o Next, bone marrow from someone else is injected into the patient (note that there’s a HLA match with this) MOD #102 Thurs, 05/15/03, 1pm Dr. Putthoff J. Uxer for Prateek Chaudhary Page 4 of 8 o The bone marrow = the graft. It can react against the host. Appears to involve several of the hypersensitivity reactions Rejection is a complex process in which both cell mediated immunity and circulating antibodies play a role T cell mediated reactions Antibody mediated reactions Morphology—Know what these are and how they’re different! o hyperacute o acute o chronic Note schematics and photomicrographs in the text p. 208-209 Look at methods of increasing graft survival, transplantation of other solid organs, and transplantation of hematopoietic cells. Autoimmune Diseases Collagen vascular disease is another name for autoimmune disease Go through the mechanisms of autoimmune diseases. Pick out the major elements—the italicized and/or bolded things. Know the criteria for being considered an autoimmune disease Only a few diseases fit this criteria; systemic lupus erythematosus is one that does. There is an arrangement of antinuclear antibodies (DNA, RNA, histones, illicit antibody formations) in all autoimmune diseases. As you age, you increase the number of antibiodies titered from your body, yet you’re perfectly healthy. [def] pathologic immunity (3 criteria) Table 7-6** The autoimmune diseases form a spectrum o autoantibodies specifically directed against B cells in the pancreatic islets (ID DM) o antibodies directed against components of glomerular and alveolar septal basement membranes cause injury and disease in those specific organs o a diversity of antibodies directed against DNA, platelets, red cells and protein-phospholipid complexes resulting in lesions ubiquitous throughout the body (SLE) Immunologic tolerance o Central tolerance o Peripheral tolerance Mechanisms of autoimmune diseases o -it is clear that there are a number of ways by which tolerance can be bypassed, thus terminating a previously unresponsive state to autoantigens o pp. 214 – 215, esp. genetic factors V. A. Systemic lupus erythematosus MOD #102 Thurs, 05/15/03, 1pm Dr. Putthoff J. Uxer for Prateek Chaudhary Page 5 of 8 The classic prototype of the multisystem disease of autoimmune origin, characterized by a bewildering array of autoantibodies, particularly antinuclear antibodies (ANAs) Acute or insidious in its onset, it is a chronic, remitting and relapsing, often febrile illness characterized principally by injury to the skin, joints, kidney and serosal membranes. However, virtually any and possibly every other organ in the body may also be affected Table 7-7, pg. 217* Prevalence gender predilection ethnic predilection Etiology and pathogenesis – ANAs can be grouped into (4) categories* – Know the patterns of nuclear immunofluorescence – Which antibodies (2) are virtually diagnostic of SLE? – See Table 7-8** and group by antibody system Note what the latest experimental evidence says about o genetic factors o nongenetic factors o immunologic factors Presentation: melar rash, sericitis—inflammation or transudate, pleurities, pericarditis, joint effusions, endocarditis—very common Morphology – Table 7-9, pg. 220* – Summary of disease, pg. 220* – kidney – skin – joints – CNS – pericarditis and other serosal cavities – heart, endocarditis, etc.—can see Lipman Sack’s endocarditis plateletfibrin deposits on the heart valves. These are not infectious. Infectious endocarditis is seen in IV drug users and immunocompromised patients. Staff endocarditis is necrotizing and eats through the heart valves. – spleen – lungs – other organs and tissues – ?: “lupus anticoagulant” (referred to by Dr. Wasson) These cause DVT and thrombosis in other parts of the body. This is counterintuitive to what you’d expect. Clinical course (what are the most common causes of death due to SLE?) Important to differentiate between the types of lupus. Chronic discoid lupus erythematosus—primarily involves skin MOD #102 Thurs, 05/15/03, 1pm Dr. Putthoff J. Uxer for Prateek Chaudhary Page 6 of 8 Subacute cutaneous LE Drug-induced LE—primarily has skin manifestations, but does not have the entire spectrum that SLE has Know the antibodies. They will be on the exam. B. Sjogren Syndrome (60-90 RNP; either RNP) This is a clinicopathologic entity characterized by dry eyes (keratoconjunctivitis sicca) and dry mouth (xerostomia) resulting from immunologically mediated destruction of the lacrimal and salivary glands o Xerostomia predisposes a person to infection because enzymes and secretory IgA are in the mouth when it is wet. o Woldyers ring—at the back of the throat including the palatine tonsils. Leukemias can present here, and only here. Sjogren Syndrome is not well understood. Etiology and pathogensis o lymphocytic infiltrates o Genetic factors o T cell involvement? o @ w/ viruses, HIV, HTLV-1? T-cell injury recently associated with HIV and HTLV-1 (note that these are not the same virus. HIV 1, HIV 2 lead to AIDS, HTLV-1 thru 3 lead to T-cell lymphomas) Refer back to Table 7-8, pg. 218* for the antibody patterns and which antibodies are most common Clinical manifestations & laboratory manifestations. It’s a clinical pathologic presentation. o See lacrimal swelling. o Oraniod configuration—epitheliod cells with inflammatory cells infiltrating major lacrimal glands (sublingual, submandibular, parotid). Can also affect minor lacrimal glands in the lips and oral cavity. Many times a lip biopsy is done for confirmation. This is not solely indicative of Sjogren’s. How do you diagnose Sjogren Syndrome? (60-90 RNP; either RNP) C. (Progressive) Systemic sclerosis (scleroderma) (DNA topo I 28-70) Characterized by excessive fibrosis throughout the body Think of it as diffuse systemic scarring. Look at the pictures in the book for a better idea. These patients can even have trouble opening their mouths due to the contractures. Diffuse Localized—morphia CREST syndrome—calcinosis, Raynaud’s phenomena, esophageal problems, sclerodactyly, and telangiectasia Etiology and pathogenesis MOD #102 Thurs, 05/15/03, 1pm Dr. Putthoff J. Uxer for Prateek Chaudhary Page 7 of 8 D. E. F. G. microvascular disease is consistently present early in the course of SS (both immune and non-immune)—CREST syndrome is more limited with a better prognostic (centromeric proteins = 90) Sometimes the small blood vessels are obliterated. Table 7-8, pg. 218* Morphology/organ involvement o Skin—atrophic epidermis, expansion of dermis, destruction of sebaceous glands leading to alopecia. o alimentary tract o musculoskeletal system o kidneys o lungs o Heart Clinical course Inflammatory myopathies (histadyl-t-RNA synthetase = 25) Uncommon Favorite question on national boards Inflammatory myopathies comprise an uncommon, heterogeneous group of disorders characterized by immunologically-mediated injury and inflammation of mainly the skeletal muscles Dermatomyositis—affects proximal muscles, have a skin rash, heliotroph (blue tint) on eyelids, affects bilaterally Polymyositis—proximal muscles; bilaterally affects patient Inclusion-body myositis—1st described in the last 10 years; asymmetrical distribution; affects distal muscles Know the etiology and pathogenesis for each. Also note the differences in age distributions Mixed connective tissue disease Note especially ANA patterns/titers Clinical manifestation Diagnosis Treatment—steroids, radiation treatment Shows different ANA patterns. Note these in the text. Serologically high titers to ribonucleoproteins Polyarteritis Nodosa and other vasulitides Not very common Involve kidneys and all other blood vessels Primarily involves medium caliber arteries (past board question) Inflammatory cells in blood vessel walls May see fibrinoid. Summary Immunologic deficiency syndromes be able to [def], describe, know major manifestations and unique (differentiating) features MOD #102 Thurs, 05/15/03, 1pm Dr. Putthoff J. Uxer for Prateek Chaudhary Page 8 of 8 Tell what immunodeficiency you have in each of the following diseases. Know the MAJOR clinical manifestation. Primary immunodeficiencies – X-linked agammaglobulinemia of Bruton – Common variable immunodeficiency – Isolated IgA deficiency—most common – Hyper IgM syndrome—associated with lymphoma – DiGeorge Syndrome (Thymic hypoplasia)—very little or no thymus – SCID—Severe Combined Immunodeficiency Disease – Immunodeficiency with thrombocytopenia and Eczema (WiskottAldrich Syndrome) – Genetic deficiencies of the complement system VI. Acquired Immunodeficiency Syndrome This book has the “best discussion of AIDS” Every year you hear of extending people’s lives when they have AIDS, so some docs are calling it a chronic disease. This really only occurs because they caught the disease early and begin treatment Many times we will just see them in the end stages. ~40% of the African population is HIV +. This is probably a different strain. AIDS is a retroviral disease characterized by profound immunosuppression that leads to opportunistic infections, secondary neoplasms and neurologic manifestations A modern plague; morbidity and mortality are staggering Epidemiology – at least 5 groups of adults in US are considered high-risk o KNOW THE GROUPS! o Homosexual/bisexual men are the largest group. o Those at highest risk are the receptive partner in anal intercourse because the mucosa is easily torn allowing the virus access to the inside of the body. o In heath care, it usually occurs with very deep needle sticks. 3 major routes of transmission Etiology Know that p24, gp120, and gp41 are used to diagnose AIDS and are capsid proteins. They are important in the search for vaccines. New vaccines have tried to make viruses with the antibodies against the capsid proteins. These are usually attenuated live viruses like polio, but to date this has not worked for AIDS because you cannot attenuate live HIV.