Autoimmunity & Multiple Sclerosis Lab Notes
advertisement
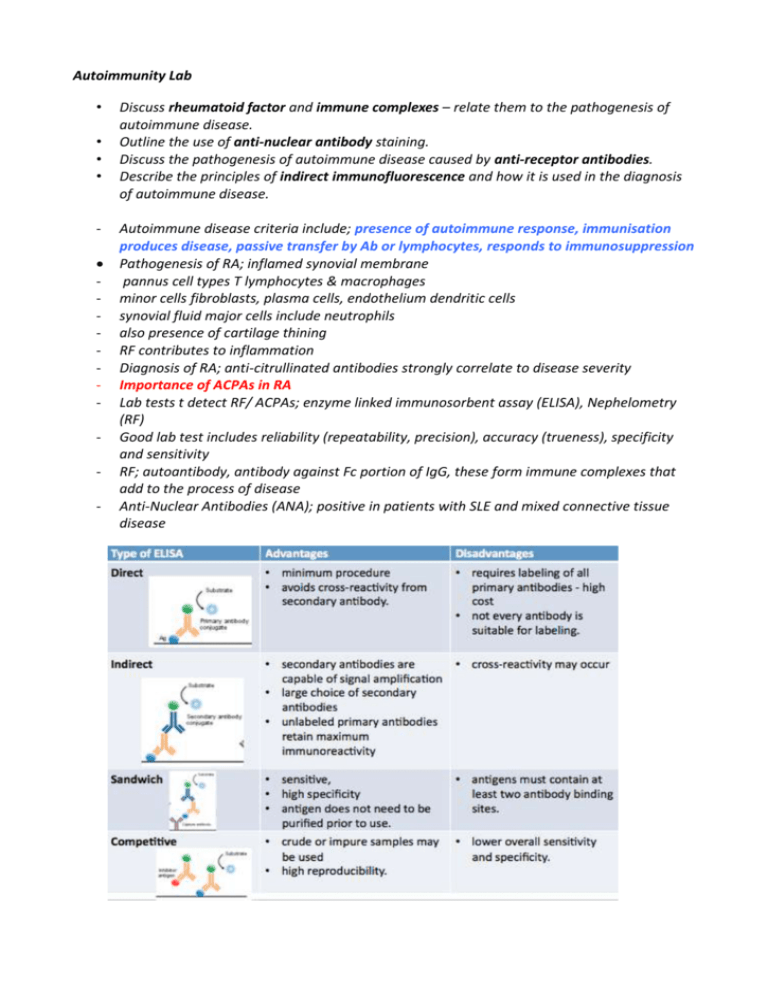
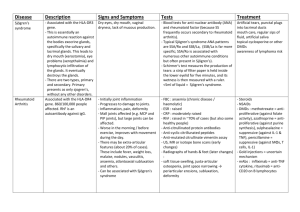
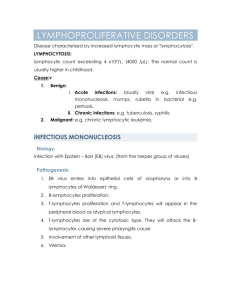
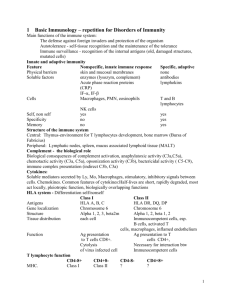
Autoimmunity Lab • • • • - Discuss rheumatoid factor and immune complexes – relate them to the pathogenesis of autoimmune disease. Outline the use of anti-nuclear antibody staining. Discuss the pathogenesis of autoimmune disease caused by anti-receptor antibodies. Describe the principles of indirect immunofluorescence and how it is used in the diagnosis of autoimmune disease. Autoimmune disease criteria include; presence of autoimmune response, immunisation produces disease, passive transfer by Ab or lymphocytes, responds to immunosuppression Pathogenesis of RA; inflamed synovial membrane pannus cell types T lymphocytes & macrophages minor cells fibroblasts, plasma cells, endothelium dendritic cells synovial fluid major cells include neutrophils also presence of cartilage thining RF contributes to inflammation Diagnosis of RA; anti-citrullinated antibodies strongly correlate to disease severity Importance of ACPAs in RA Lab tests t detect RF/ ACPAs; enzyme linked immunosorbent assay (ELISA), Nephelometry (RF) Good lab test includes reliability (repeatability, precision), accuracy (trueness), specificity and sensitivity RF; autoantibody, antibody against Fc portion of IgG, these form immune complexes that add to the process of disease Anti-Nuclear Antibodies (ANA); positive in patients with SLE and mixed connective tissue disease ANAs - useful auto-antibody tests that detect autoimmune conditions, it’s a group of antibodies that are able to bind to locations in the nucleus binding sites include; homogenous, centromere, peripheral (nuclear envelope), speckled (proteins) and nucleolus the ANA’s are detected through immunoflourescence and ELIZA diseases that can be identified include SLE, RA, Scleroderma etc. Sjogren’s syndrome is identified using ‘Schirmer’s Test’, this looks at the dry eye condition, it tests tear production in patients Anti receptor antibodies are diagnostic for myasthenia gravis and graves disease AID’s caused by anti-receptor antibodies - Myadthenia gravis -> anti-acetylcholine receptor - Grave’s disease ->anti-TSH receptor - Type B insulin resistance syndrome -> anti-insulin receptor - Anti-NMDA autoimmune encephalitis -> anti-NMDA (glutamate) receptor (controls synaptic plasticity & function of memory) Immune complex mediated - Systemic lupus rythromatosis - Rheumatoid arthritis - Vasculitis Antibody mediated - Thyrotoxicosis Pernicious anaemia Myasthenia gravis Immune thrombocytopenia Cell mediated - Hashimoto’s Thyrodiditis Diabetes mellitus Multiple sclerosis Sjogrens syndrome MY RESEARCH TEAM TASK – MULTIPLE SCLEROSIS MULTIPLE SCLEROSIS - It’s a demyelinating disorder characterised by white mater lesions that are separated in space. Immune system attacks myelin covering nerves this damage disrupts communication between the brain and the body. Nerves may deteriorate- loss of motor control. 1. Outline the pathogenesis - Caused by combination of environmental and genetic factors result in a loss of tolerance to self proteins ‘myelin antigens’ - Genetic risk is associated to HLA-DR variants, DR2 allele increases the risk of developing MS significantly - Polymorphisms in genes encoding receptors for cytokines IL-2 and IL-7, control the activation and regulation of T-cell mediated immune responses - Immune mediated myelin destruction has a role in MS - CD4+T cells with increase in Th17 and Th1 CD4+ cells critical role in injury to myelin - Demyelination is most evident with some axonal loss - Toxic effects of lymphocytes, macrophages and secreted molecules have been implicated in initiating the process of axonal injury, leads to neuronal death 2. Describe the type of laboratory tests used in diagnosis Laboratory test used in diagnosis - Tests used include MRI, Cerebrospinal fluid analysis, visual evoked potentials MRI is the best diagnostic test for MS Detects areas of the brain/spinal cord that CAT scans may miss MRI involves injections of contrast dye material that allow us to see the abnormalities found in the brain in the scan images 3. Explain the principles of how the tests work - - - Test produces clear images of the human body in this case the brain It uses large magnetic radio waves and a computer to produce theses images Unlike conventional x-ray examinations and computed tomography (CT) scans, MRI does not depend on ionizing radiation. Radio waves redirect the axes of spinning protons, which are the nuclei of hydrogen atoms. The magnetic field is produced by passing an electric current through wire coils in most MRI units. Other coils, located in the machine and in some cases, placed around the part of the body being imaged, send and receive radio waves, producing signals that are detected by the coils. A computer then processes the signals and generates a series of images, each of which the contrast dye allows for certain tissues and blood vessels to be seen in more detail and clarity this is usually gadolinium, may be given to you intravenously The MRI is a cylinder with both sides being open, the patient lies on a motorised bed that moves inside the scanner The MRI scan is studied by a radiologist and specialist 4. Discuss any Limitations or issues with the test There are issues between lesion location and the clinical presentation Can vary in sensitivity and specificity in diagnosis this depends on the number of location findings The strong magnetic field is not harmful, only an issue if patients have implanted medical devices that contain metal may malfunction or cause problems during MRI exam include inner ear implants, artificial joints, defibrillator or pacemaker, particular types of heart valves, vascular stents, brain aneurysm clips Not recommended for pregnant women Doesn’t have the ability to find all cancers (breast- microcalcifications) Cannot always distinguish between benign and malignant Difficult procedure for those who have claustrophobia Sometimes patients may develop allergic reaction to the contrasting agent, this is can be prevented Expensive procedure
![Immune Sys Quiz[1] - kyoussef-mci](http://s3.studylib.net/store/data/006621981_1-02033c62cab9330a6e1312a8f53a74c4-300x300.png)