Presentation
advertisement

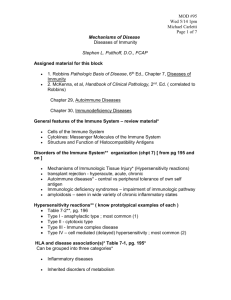
Lecture outline • Types of hypersensitivity • Immediate hypersensitivity, allergy • Antibody-mediated diseases • T cell-mediated diseases • Therapeutic approaches Immunological (hypersensitivity) diseases • Diseases caused by aberrant immune reactions – Reactions against self antigens (autoimmunity) – Uncontrolled or excessive reactions against foreign antigens – Component of normal immune responses to microbes • Mechanisms of tissue injury are the same as the effector mechanisms of protective immunity – The immune response is inappropriately directed or inadequately controlled • The nature of the disease is determined by the type of immune response – Diseases are classified based on immune mechanisms: useful for understanding pathogenesis, but many diseases involve multiple mechanisms Types of hypersensitivity disease Pathogenic immune response Mechanism of tissue injury Immediate hypersensitivity (Type I) IgE antibody, mast cells Mast cell mediators Antibody mediated (Type II) IgM and IgG antibodies against cell and matrix antigens •Phagocytosis •Complement •Interference with cell functions Complexes of circulating Immune complex antigens and IgM or mediated (Type III) IgG antibodies Complement and Fc receptor mediated inflammation T cell mediated (Type IV) •Cytokinemediated inflammation •Killing by CTLs Type of hypersensitivity CD4 and CD8 T cells Immediate hypersensitivity reaction Stages of immediate hypersensitivity reactions Sequence of events in immediate hypersensitivity Actions of mast cell mediators Mast cell products are responsible for the manifestations of immediate hypersensitivity Clinical manifestations of immediate hypersensitivity Treatment of immediate hypersensitivity disorders Genetic susceptibility for immediate hypersensitivity • Allergic diseases run in families – Different members of the same family may show different manifestations of immediate hypersensitivity (“atopy”) • Multiple susceptibility genes have been identified by gene mapping and family studies – Genes may influence TH2 responses, IgE production, mast cell activation, end-organ sensitivity – Susceptibility loci identified include: HLA (immune responsiveness); cytokine gene cluster; others How antibodies deposit in tissues Antibody is specific for tissue antigen (typically self): disease is specific for target tissue Antibody reacts with circulating antigen (self or foreign), and complexes tend to deposit in small vessels; not specific for any tissue How antibodies cause disease -- 1 Neutrophils (and monocytes) are recruited by complement products (generated by the classical pathway) and bind to Fc tails of deposited antibodies, and are activated. Leukocyte recruitment and activation are part of inflammation. Experimental models of immune complex diseases • Serum sickness – Systemic immunization with large dose of protein antigen --> circulating immune complexes --> complexes deposit in vessels and cause inflammation (Fc receptor and complement-mediated) – Arthritis, vasculitis, glomerulonephritis • Arthus reaction – Subcutaneous administration of antigen in previously immunized individual --> formation and deposition of local immune complexes – Cutaneous vasculitis Immune complex-mediated glomerulonephritis Anti-basement membrane antibodymediated glomerulonephritis How antibodies cause disease -- 2 Antibody and/or complement (C3b) are deposited on cell and are recognized by receptors for Fc or C3b on phagocytes --> coated (opsonized) cell is ingested and destroyed. Basis of autoantibody-mediated depletion of RBCs, platelets How antibodies cause disease -- 3 Causes of antibody-mediated diseases • Autoimmunity (production of autoantibodies) – May be due to failure of self-tolerance in autoreactive B cells or helper T cells • Antibody responses to foreign antigens – Antibodies against hepatitis B form immune complexes --> vasculitis (polyarteritis nodosa) – Post-streptococcal glomerulonephritis: immune complexes of Strep antigen + anti-Strep antibodies; may be formed in circulation or on GBM – Not known why immune complex diseases develop in rare individuals after common infections How T cells injure tissues -- 1 CD4+ T cells respond to self (or microbial) antigens, produce cytokines that recruit and activate macrophages and neutrophils, and the products of these leukocytes damage tissues; also called delayed type hypersensitivity because of the time involved in recruiting and activating specific T cells and other leukocytes. Recall that the same reaction destroys phagocytosed microbes (cell-mediated immunity, one arm of host defense) Delayed type hypersensitivity (DTH) reaction Morphology of a delayed type hypersensitivity (DTH) reaction Classically attributed to Th1 response; may include Th17. This reaction is also the cause of several immunological diseases of humans (MS, Crohn’s, type 1 diabetes, etc) How T cells injure tissues -- 2 Cytotoxic T lymphocytes (CTLs) react against antigens in host tissues and kill (“lyse”) the host cells. Causes of T cell-mediated hypersensitivity diseases • Autoimmunity – Type 1 diabetes, multiple sclerosis, rheumatoid arthritis • Reaction to microbes and other foreign antigens – Contact sensitivity (DTH) to chemicals (poison ivy) – Tuberculosis (granulomatous inflammation in response to a persistent microbe: chronic DTH) – Crohn’s disease (excessive Th1 and Th17 responses to gut commensals?) – Viral hepatitis (CTLs kill virus-infected hepatocytes); not considered an example of “hypersensitivity” Immune-mediated inflammatory diseases • A term for diseases caused by abnormal or unregulated immune responses (usually excluding allergies) in which inflammation (usually chronic) is prominent – Multiple immune mechanisms (antibodies, T cells) may be involved in one disease; classification of types I - IV is of limited use clinically – Similar therapeutic strategies are effective for different diseases in this group • Typically caused by autoimmunity; sometimes, exaggerated responses to microbes Chronicity of immune-mediated inflammatory diseases • Many of these hypersensitivity diseases are chronic and even self-perpetuating because: – The initiating stimuli cannot be removed (self or environmental antigens, persistent microbes) – The immune response tends to amplify itself (normally, enables few antigen-specific lymphocytes to deal with infections) Amplification loop in DTH reactions Cytokines are powerful amplifiers of immune reactions Therapy of immune diseases: the current way • Block the production or counteract the actions of effector molecules that cause tissue injury – Anti-inflammatory drugs, e.g. steroids – Block T cell activation (immunosuppressive drugs, e.g. cyclosporine) – Deplete pathogenic antibodies (plasmapheresis), B or T lymphocytes (depleting antibodies) • Empirical – Desensitization for allergy – Intravenous IgG (IVIg): engages inhibitory FcR on B cells? Therapy of immune disorders: rational approaches target lymphocyte activation and subsequent inflammation CTLA-4.Ig Inhibitors of calcineurin, (block costimulation) various kinases (inhibit signaling) CD28 IL-2 APC TCR T cell Anti-IL-2R (block cytokine receptor) IL-17A Anti-IL-17A IL-12, IL-23 (p40) TNF, IL-1, TNF, IL-1, IL-6R IL-6 Anti-p40 antagonists (block cytokines) Inflammation Anti-integrin antibodies (block adhesion) Molecularly targeted therapies for immunological diseases: the rational approach • Target the molecular basis of lymphocyte activation and effector functions: rationally designed therapies – Based on understanding of lymphocyte biology – Risks -- reactivation of infections • Induce antigen-specific immunological tolerance: requires identification of target antigens – Being tried in MS, type 1 diabetes