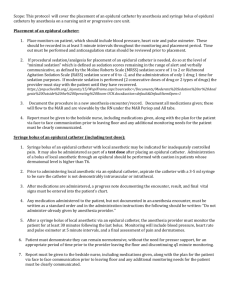
sedation score
advertisement

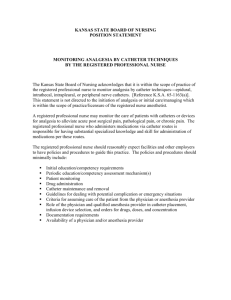
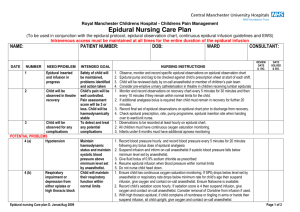
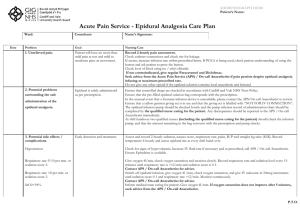
STANDING ORDERS AND PROBLEM SOLVING FOR EPIDURAL OBSERVATION CHART SEDATION AND RESPIRATORY DEPRESSION SEDATION SCORE SEDATION SCORE OF 3 AND/OR RESPIRATORY RATE < 9 (adult) 0 = Awake and alert Paediatrics: Respiratory rate below stated parameters Notify APS or duty anaesthetic registrar immediately. Give O2 6 litre/min via Hudson mask; Cease epidural infusion Reduce PCEA bolus dose by half; Consider Naloxone: Adults: 100mcg IV PRN to a maximum 400mcg Paediatrics: Prepare Naloxone as ordered SEDATION SCORE OF 4 (REGARDLESS OF RESPIRATORY RATE) CALL MET As above AND give naloxone at 2 minute intervals 1 = Normally asleep, responds to stimuli, wakes easily 2 = Mild, occasionally drowsy, easy to rouse 3 = Moderate, frequently drowsy, easy to rouse but unable to maintain wakeful state 4 = Severe, somnolent, difficult to rouse INADEQUATE ANALGESIA Verbal Numerical Rating Scale (VNRS): 0 = No pain to 10 = Worst possible pain Check epidural catheter has not migrated using catheter mark at skin and depth as an indicator. If patient hemodynamically stable give loading dose and increase infusion rate within range limit (not PCEA). If catheter has migrated, or loading and rate increase have been ineffective, contact APS. Ensure regular paracetamol is given if ordered. If pain continues to be a problem contact APS or Duty Anaesthetic Registrar NAUSEA AND VOMITING Nausea/Vomiting Score 0 = No nausea or vomiting N = Nauseated V = Vomited Management - Adults 1. 2. 3. Metoclopramide 10-20mg IV 4 hourly PRN. Ondansetron 4mg IV/oral 12 hourly PRN. If no response, contact APS duty anaesthetic registrar. PRURITUS 0 = Nil 1 = Mild 2 = Severe If pruritus is considered to be due to the opioids and is troublesome to the patient then ondansetron 4mg wafer 12 hourly PRN or titration of a single dose of naloxone (50-100mcg) may be effective without reversing analgesia (Paediatrics require individual assessment). If ineffective, contact APS or duty anaesthetic registrar. Use of antihistamines may cause sedation and compromise safety therefore is not recommended. MOTOR BLOCK Bromage Scale 0 = none – full flexion of knees and feet 1 = partial – just able to move knees 2 = almost complete – able to move feet only 3 = complete – unable to move feet or knees Both legs to be assessed separately Remember to routinely check for pressure areas if limbs are numb Ensure patient is safe to ambulate If a limb has a dense motor block (i.e. 3) contact the APS or duty anaesthetist Management Reduce rate of infusion if Motor Block is 1 or over. If motor block does not show improvement within one hour contact APS or duty anaesthetist. CATHETER MARK AT SKIN AND SITE CHECK To be attended 4 hourly. Note centimetre mark on catheter at skin level (if observable) on observation sheet. If the catheter site appears infected, inflamed or tender contact the APS or duty anaesthetist. The dressing covering the catheter may require reinforcing. If the insertion site is exposed contact APS or duty anaesthetist. EPIDURAL REMOVAL GUIDELINES WHEN USING ANTICOAGULANTS Because of the risk of epidural haematomas, any patient with an epidural who is also receiving anticoagulant medication (including DVT prophylaxis) should have the epidural removed at a time determined by the APS (see ALERT on obs sheet). Should an epidural inadvertently fall out or be removed while a patient is on anticoagulant therapy, the APS or Emergency Anaesthetic Registrar must be informed immediately. While NSAID agents alone are probably safe, the combination of NSAID drugs and other anticoagulants (eg Clexane) is dangerous while an epidural is in situ. HYPOTENSION If BP falls to ________________________give ___________mls of ____________________________IV stat. Give O 6 litre/min by Hudson mask. Call medical officer and APS. Ensure Ephedrine 30mg is available. 2 _____________________________________________________________ ____ / ____ / ____ Anaesthetist signature Print name Date Calvary Health Care ACT Acute Pain Service Patient Controlled Epidural Analgesia (PCEA) Birthing Suite Patient Label CH -0152 (08/08) Weight: BMI Allergies: Level ______________________ Catheter in Space _________________ Needle Gauge__________________ Test Dose _______________________ Loss of Resistance________________ Effect Achieved ___________________ Skin to Space_____________________ Drug:_________________________ Standing Orders: 1. No opioid or sedatives by any route except as ordered by Acute Pain Service (APS), or attending anaesthetist 2. OXYGEN at ____________litres/min VIA ______________ continuously for 8 hours then when resting or sleeping 3. Maintain patent IV cannula for 12 hours after removing epidural 4. Observations: 4.1 Prior to commencing infusion or giving loading dose: record blood pressure, pulse rate, respiratory rate, sedation score, and pain score (VNRS). 4.2 Sedation score, oxygen saturation, respiratory rate, pain score, vomiting score, pruritus, rate of infusion and total amount infused hourly for the duration of the infusion. Blood pressure and pulse rate hourly for 4 hours, 2 hourly for 4 hours, then 4 hourly. 4.3 Motor block assessment and sensory level 2 hourly, insertion site assessment 4 hourly. 4.4 Motor block assessment to continue 2 hourly for 24 hours after removal of epidural catheter. Notify APS or anaesthetic registrar immediately if any weakness or numbness present 4.5 PCEA only: Record Total Demands and Good Demands 2 hourly for duration of epidural and parameter checks as indicated 4.6 Loading doses: Check blood pressure and pulse rate every 5 minutes for 20 minutes and again 1 hour after loading. Not necessary for PCEA boluses 4.6 Record discarded amounts on observation chart and in S8 discard register 4.7 Patient must be woken for observations Standard Solution: Ropivacaine 2mg/ml in 100mls Normal Saline with Fentanyl 4mcg/ml = concentration 4mcg/ml (poly bag). Local Anaesthetic:________________________________Opioid:__________________________ Volume of PCEA Bolus 4mls 5ml 6mls Lockout:________(min) Signature of Anaesthetist: ________________________Print Name:_________________ Date:______________ Time ________________ Record of Infusion Bags Date Time Signature Witness Date Time Signature Witness Epidural Analgesia Chart Birthing Suite Comments/Complications: PROGRESS NOTES/COMMENTS Epidural Catheter Removed (Note: If patient is on Clexane remove the catheter 12 hours after the last administration to avoid haematoma at epidural site) Date___/___/____ Time________________ Catheter tip: Intact / Not Intact (Circle one) Signature_________________Print Name ___________________Witness ___________________ If catheter NOT INTACT contact APS or Anaesthetic Registrar on call and keep epidural catheter PCEA OBSERVATION CHART Following initial insertion and supplement dose the observations are Pulse, Resps, BP, FHR, 5 minutely for 30 minutes. Then 30 minutely as per partogram. Sedation score, pain score and sensory block hourly. Date Time PCEA Mcg dose Cumulative Volume Pain score Sedation Score Sensory Block BP Pulse Resp FHR Comments