Epidural Anesthesia Placement in a Factor XI Defecient Patient
advertisement
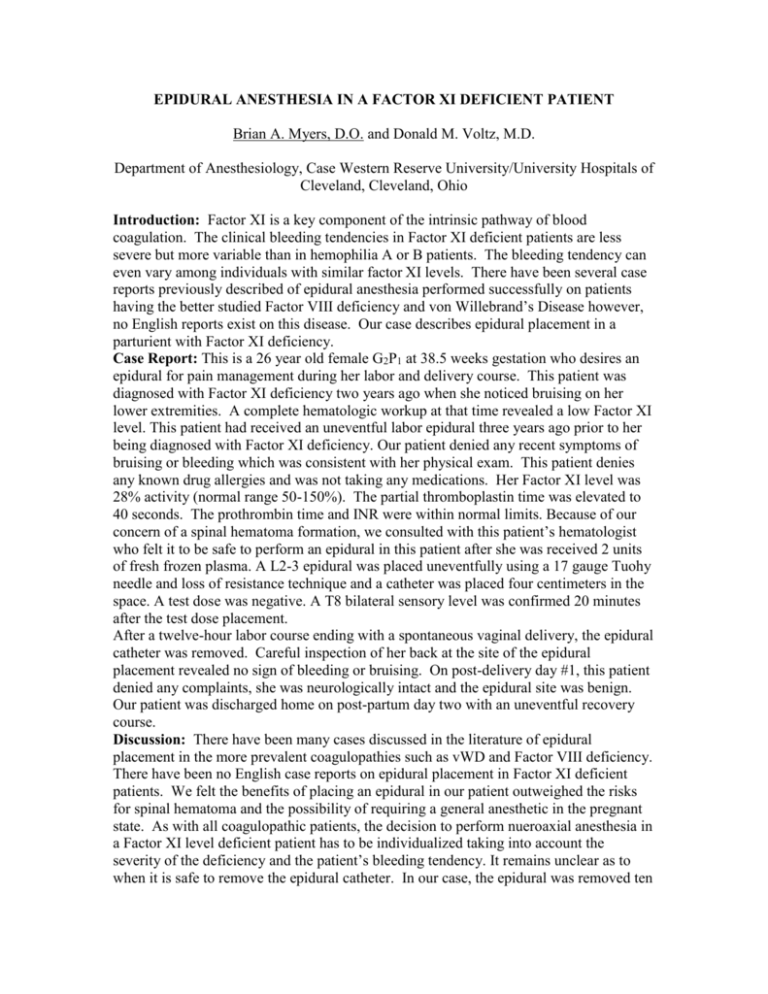
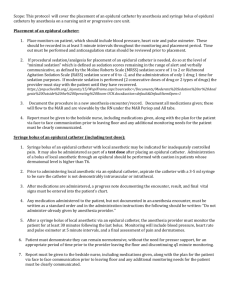
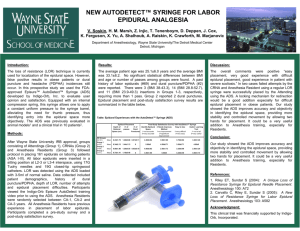
EPIDURAL ANESTHESIA IN A FACTOR XI DEFICIENT PATIENT Brian A. Myers, D.O. and Donald M. Voltz, M.D. Department of Anesthesiology, Case Western Reserve University/University Hospitals of Cleveland, Cleveland, Ohio Introduction: Factor XI is a key component of the intrinsic pathway of blood coagulation. The clinical bleeding tendencies in Factor XI deficient patients are less severe but more variable than in hemophilia A or B patients. The bleeding tendency can even vary among individuals with similar factor XI levels. There have been several case reports previously described of epidural anesthesia performed successfully on patients having the better studied Factor VIII deficiency and von Willebrand’s Disease however, no English reports exist on this disease. Our case describes epidural placement in a parturient with Factor XI deficiency. Case Report: This is a 26 year old female G2P1 at 38.5 weeks gestation who desires an epidural for pain management during her labor and delivery course. This patient was diagnosed with Factor XI deficiency two years ago when she noticed bruising on her lower extremities. A complete hematologic workup at that time revealed a low Factor XI level. This patient had received an uneventful labor epidural three years ago prior to her being diagnosed with Factor XI deficiency. Our patient denied any recent symptoms of bruising or bleeding which was consistent with her physical exam. This patient denies any known drug allergies and was not taking any medications. Her Factor XI level was 28% activity (normal range 50-150%). The partial thromboplastin time was elevated to 40 seconds. The prothrombin time and INR were within normal limits. Because of our concern of a spinal hematoma formation, we consulted with this patient’s hematologist who felt it to be safe to perform an epidural in this patient after she was received 2 units of fresh frozen plasma. A L2-3 epidural was placed uneventfully using a 17 gauge Tuohy needle and loss of resistance technique and a catheter was placed four centimeters in the space. A test dose was negative. A T8 bilateral sensory level was confirmed 20 minutes after the test dose placement. After a twelve-hour labor course ending with a spontaneous vaginal delivery, the epidural catheter was removed. Careful inspection of her back at the site of the epidural placement revealed no sign of bleeding or bruising. On post-delivery day #1, this patient denied any complaints, she was neurologically intact and the epidural site was benign. Our patient was discharged home on post-partum day two with an uneventful recovery course. Discussion: There have been many cases discussed in the literature of epidural placement in the more prevalent coagulopathies such as vWD and Factor VIII deficiency. There have been no English case reports on epidural placement in Factor XI deficient patients. We felt the benefits of placing an epidural in our patient outweighed the risks for spinal hematoma and the possibility of requiring a general anesthetic in the pregnant state. As with all coagulopathic patients, the decision to perform nueroaxial anesthesia in a Factor XI level deficient patient has to be individualized taking into account the severity of the deficiency and the patient’s bleeding tendency. It remains unclear as to when it is safe to remove the epidural catheter. In our case, the epidural was removed ten hours after treatment with FFP. If there is a concern for an increased bleeding tendency at the time of removal of the epidural catheter, coagulation studies should be repeated paying special attention to the partial thromboplastin time.