Epidural nursing Care Plan 2009
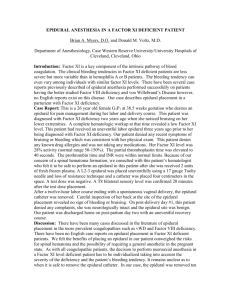
advertisement
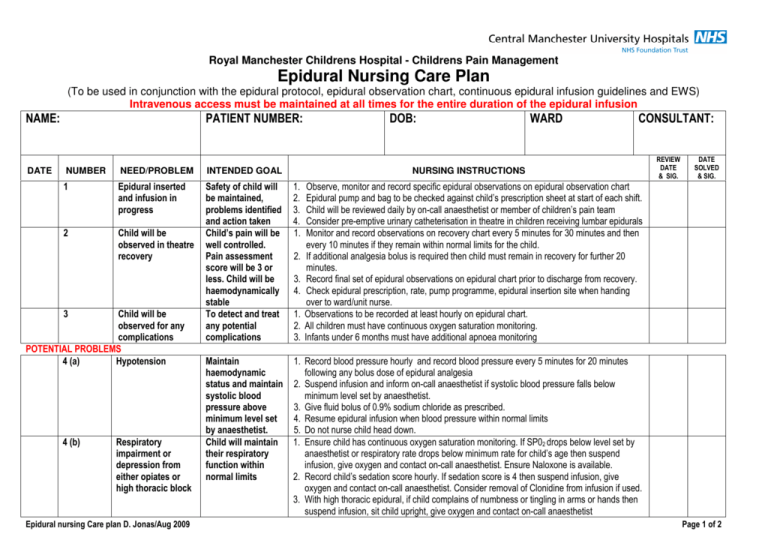
Royal Manchester Childrens Hospital - Childrens Pain Management Epidural Nursing Care Plan (To be used in conjunction with the epidural protocol, epidural observation chart, continuous epidural infusion guidelines and EWS) Intravenous access must be maintained at all times for the entire duration of the epidural infusion NAME: DATE PATIENT NUMBER: DOB: WARD CONSULTANT: NUMBER NEED/PROBLEM INTENDED GOAL 1 Epidural inserted and infusion in progress 2 Child will be observed in theatre recovery Safety of child will be maintained, problems identified and action taken Child’s pain will be well controlled. Pain assessment score will be 3 or less. Child will be haemodynamically stable To detect and treat any potential complications 1. 2. 3. 4. 1. Maintain haemodynamic status and maintain systolic blood pressure above minimum level set by anaesthetist. Child will maintain their respiratory function within normal limits 1. Record blood pressure hourly and record blood pressure every 5 minutes for 20 minutes following any bolus dose of epidural analgesia 2. Suspend infusion and inform on-call anaesthetist if systolic blood pressure falls below minimum level set by anaesthetist. 3. Give fluid bolus of 0.9% sodium chloride as prescribed. 4. Resume epidural infusion when blood pressure within normal limits 5. Do not nurse child head down. 1. Ensure child has continuous oxygen saturation monitoring. If SP02 drops below level set by anaesthetist or respiratory rate drops below minimum rate for child’s age then suspend infusion, give oxygen and contact on-call anaesthetist. Ensure Naloxone is available. 2. Record child’s sedation score hourly. If sedation score is 4 then suspend infusion, give oxygen and contact on-call anaesthetist. Consider removal of Clonidine from infusion if used. 3. With high thoracic epidural, if child complains of numbness or tingling in arms or hands then suspend infusion, sit child upright, give oxygen and contact on-call anaesthetist 3 Child will be observed for any complications POTENTIAL PROBLEMS 4 (a) Hypotension 4 (b) Respiratory impairment or depression from either opiates or high thoracic block Epidural nursing Care plan D. Jonas/Aug 2009 NURSING INSTRUCTIONS 2. 3. 4. 1. 2. 3. REVIEW DATE & SIG. DATE SOLVED & SIG. Observe, monitor and record specific epidural observations on epidural observation chart Epidural pump and bag to be checked against child’s prescription sheet at start of each shift. Child will be reviewed daily by on-call anaesthetist or member of children’s pain team Consider pre-emptive urinary catheterisation in theatre in children receiving lumbar epidurals Monitor and record observations on recovery chart every 5 minutes for 30 minutes and then every 10 minutes if they remain within normal limits for the child. If additional analgesia bolus is required then child must remain in recovery for further 20 minutes. Record final set of epidural observations on epidural chart prior to discharge from recovery. Check epidural prescription, rate, pump programme, epidural insertion site when handing over to ward/unit nurse. Observations to be recorded at least hourly on epidural chart. All children must have continuous oxygen saturation monitoring. Infants under 6 months must have additional apnoea monitoring Page 1 of 2 4 (c) Loss of motor function or diminished sensation Child’s skin will remain intact. Full movement of toes or feet, arms and hands will be maintained 4 (d) Inadequate analgesia Child’s pain will be controlled 4 (e) Nausea & vomiting 4 (f) Urinary retention 4 (g) Itching (Pruritus) 4 (h) Infection Child will have relief Child will maintain bladder function Child will have relief Infection will be prevented 1. Lower thoracic or lumbar epidural – monitor movement in both legs hourly. If no movement in both legs (motor score = 3) then suspend infusion and contact on-call anaesthetist. Loss of motor function may indicate severe neurological complication. 2. High thoracic epidural – monitor movement in hands, arms and shoulders. If child complains of numbness or tingling in arms or hands then suspend infusion, sit child upright, give oxygen and contact on-call anaesthetist. 3. Observe child’s skin and pressure areas 3 hourly. Ensure 3 hourly movement or turning. 1. Assess child’s pain hourly on scale of 0-10 using a pain assessment tool (Faces/numerical ladder or FLACC scale. 2. If pain score 7 or more contact on-call anaesthetist. 3. Give 6 hourly Paracetamol 4. Reposition child if pain apparent on only one side of body – unilateral or patchy block. 5. Check epidural insertion site 3 hourly. 1. Treat nausea and vomiting according to postoperative nausea and vomiting protocol. 1. 2. 1. 2. 1. 2. 4 (i) 5 Loss of epidural catheter or leakage Removal of epidural catheter Inadequate analgesia or catheter loss will be prevented Child’s epidural catheter will be removed safely and intact 3. 4. 1. 2. 3. 1. 2. 3. 4. 5. 6 Observe for further complications To ensure no further adverse complications 1. Ensure optimum position for micturation. Catheterise child if necessary. Give intravenous Piriton (Chlorpheniramine) as prescribed according to BNFC. Contact on-call anaesthetist if itching persists – consider removal of Fentanyl from infusion Epidural bacterial filter will remain in place at all times secured to epidural catheter with Tegaderm. Bacterial filter position will be checked hourly. If disconnection occurs contact on-call anaesthetist and follow disconnection advice in continuous epidural infusion guidelines. Check epidural catheter insertion site 3hourly, if red or inflamed contact on-call anaesthetist. Record child’s temperature at least 4 hourly. Check epidural site 3 hourly for any leakage. Contact on-call anaesthetist if excessive leakage around site and child in pain. Protect catheter by ensuring it is kept free from catching on bed sides etc. Take care when moving child around bed or out onto parent’s knee or into a chair. Ensure catheter is connected to filter and secured with Tegaderm. The epidural catheter will be removed following ANTT principles. Lie child on their side with spine curved or sit forward in bed or chair. Remove epidural dressing and tape humanely Slowly pull out the epidural catheter, examine the tip to ensure the entire catheter has been removed. Document removal. Send catheter tip to pathology for culture and sensitivity. If child receiving heparin follow advice regarding LMWH in continuous epidural infusion guidelines Continue to record all epidural observations for period of 6 hours post removal or cessation of the epidural infusion if Fentanyl has been administered in the infusion. Please do not hesitate to contact on-call anaesthetist or children’s pain team if you have any concerns regarding a child with an epidural catheter in situ. Epidural nursing Care plan D. Jonas/Aug 2009 Page 2 of 2