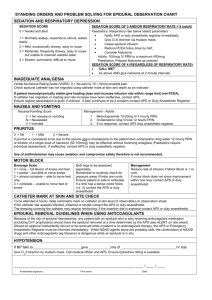
Epidural bolus and placement guidelines
advertisement
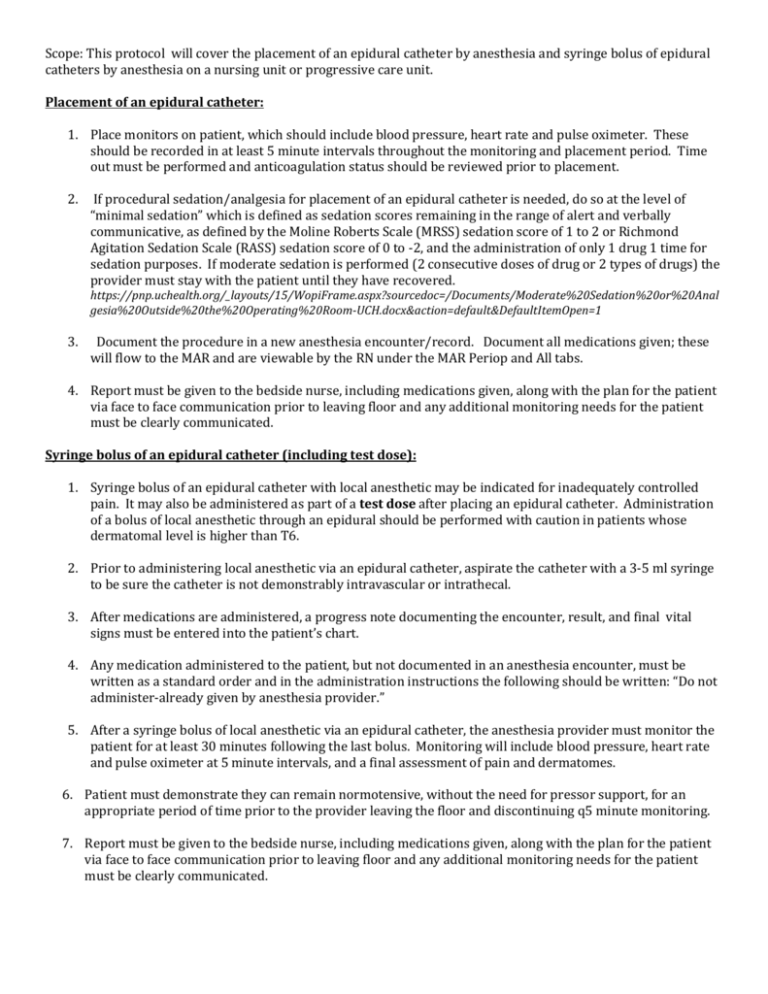
Scope: This protocol will cover the placement of an epidural catheter by anesthesia and syringe bolus of epidural catheters by anesthesia on a nursing unit or progressive care unit. Placement of an epidural catheter: 1. Place monitors on patient, which should include blood pressure, heart rate and pulse oximeter. These should be recorded in at least 5 minute intervals throughout the monitoring and placement period. Time out must be performed and anticoagulation status should be reviewed prior to placement. 2. If procedural sedation/analgesia for placement of an epidural catheter is needed, do so at the level of “minimal sedation” which is defined as sedation scores remaining in the range of alert and verbally communicative, as defined by the Moline Roberts Scale (MRSS) sedation score of 1 to 2 or Richmond Agitation Sedation Scale (RASS) sedation score of 0 to -2, and the administration of only 1 drug 1 time for sedation purposes. If moderate sedation is performed (2 consecutive doses of drug or 2 types of drugs) the provider must stay with the patient until they have recovered. https://pnp.uchealth.org/_layouts/15/WopiFrame.aspx?sourcedoc=/Documents/Moderate%20Sedation%20or%20Anal gesia%20Outside%20the%20Operating%20Room-UCH.docx&action=default&DefaultItemOpen=1 3. Document the procedure in a new anesthesia encounter/record. Document all medications given; these will flow to the MAR and are viewable by the RN under the MAR Periop and All tabs. 4. Report must be given to the bedside nurse, including medications given, along with the plan for the patient via face to face communication prior to leaving floor and any additional monitoring needs for the patient must be clearly communicated. Syringe bolus of an epidural catheter (including test dose): 1. Syringe bolus of an epidural catheter with local anesthetic may be indicated for inadequately controlled pain. It may also be administered as part of a test dose after placing an epidural catheter. Administration of a bolus of local anesthetic through an epidural should be performed with caution in patients whose dermatomal level is higher than T6. 2. Prior to administering local anesthetic via an epidural catheter, aspirate the catheter with a 3-5 ml syringe to be sure the catheter is not demonstrably intravascular or intrathecal. 3. After medications are administered, a progress note documenting the encounter, result, and final vital signs must be entered into the patient’s chart. 4. Any medication administered to the patient, but not documented in an anesthesia encounter, must be written as a standard order and in the administration instructions the following should be written: “Do not administer-already given by anesthesia provider.” 5. After a syringe bolus of local anesthetic via an epidural catheter, the anesthesia provider must monitor the patient for at least 30 minutes following the last bolus. Monitoring will include blood pressure, heart rate and pulse oximeter at 5 minute intervals, and a final assessment of pain and dermatomes. 6. Patient must demonstrate they can remain normotensive, without the need for pressor support, for an appropriate period of time prior to the provider leaving the floor and discontinuing q5 minute monitoring. 7. Report must be given to the bedside nurse, including medications given, along with the plan for the patient via face to face communication prior to leaving floor and any additional monitoring needs for the patient must be clearly communicated.