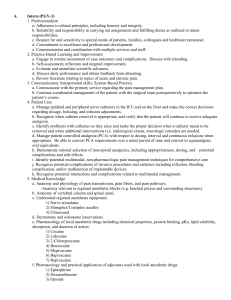
PCEA

PCEA
Analgesia delivered through an indwelling epidural catheter is a safe and effective method for management of acute post-op pain, allowing mobility and incentive spirometer use and with those faster recovery. It creates a band of analgesia in the dermatomes were the solution of epidural infusion is given.
Post op PCEA can provide superior analgesia compared with systemic opioids. However, it is important to realize that the term Epidural Analgesia incorporate a wide range of options , including Dose, Drugs,
Localization of catheter , Onset and Duration of Perioperative use.
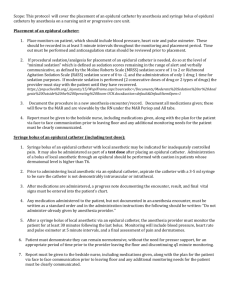
Technique: under Steril technique with patient awake and in sitting or lateral decubitus.
Epidural Catheter Level:
Thoracic Surgery: T6-T8
Abdominal Surgery: T8-T11
Contraindicaton: Use of heparin, levonox, warfarin, or any other situation that may increase INR, also low platelet count is a contraindication for epidural catheter placement.
Drugs:
1.
Local Anesthetic:
Mechanism of Action: LA Blocks voltage gated Na channels, interfiering with membrane despolarization, the impulse conduction slows, and action potential decrease until cannot be generated.
Lidocaine: 0.5%, 1.0%, 1.5%, 2% shorter duration, keep in mind that can produce seizures if administered IV in high dose.
Bupivacaine:0.1%, 0.25%, 0.5%, 0.75% longer duration of action, if administered IV can be cardiotoxic, producing lethal arrytmias. Intralipid is use as antidote.
The higher the concentration of local anesthetic, the more motor blockage.
If used alone, local anesthetic have limited effect for pain control.
2.
: Opioids:
Mechanism of Action: action on mu receptors at the spinal cord level and nerve roots.
Fentanyl: lipophilic, producing its effect at the level of spinal cord and also systemic level.
Dilaudid: hydrophilic , producing effect at the spinal cord level.
3.
Local anesthetis and Opioid combination:
Increased analgesic effect with less side effects. From the local anesthetic drugs, Bupivacaine is preferred because of minimal motor blockade with adecuate sensory blockade.
Lipophilic: Fentanyl 2-5 ucg/ml Hydrophilic: Dilaudid 0.01-0.05 mg/ml
Sufentanyl 0.5-1mcg/ml Morphine 0.05- 0.1 mg/ml
4.
Adjuvants Drugs:
Drugs added to Epidural infusion to enhance analgesia and decrease side effects:
Clonidine: action through descending noradrenergic pathway, side effects: BP, HR and sedation.
Epinephrine
Ketamine: produces attenuation of central sensitization.
SIDE EFFECTS OF NEUROAXIAL BLOCK:
Before attributing ay side effect to the epidural drugs that are being administered, it is important to first consider other causes contributing or causing “ side effects”,
--for HYPOTENSION consider low intravascular volume, bleeding, low cardiac output
-- and for RESPIRATORY DRESSION: CVA, Pulmonary Edema, Sepsis.
It is important to have protocols for analgesia regimen , neurologic monitoring, treatment of side effects and Physician notification about critical parameters.
HYPOTENSION caused by PCEA :
Local anesthetic block sympathetic fibers, that can lead to hypotension, could be treated decreasing concentration or taking LA out of the solution.
MOTOR BLOCKADE in patients with PCEA:
Local anesthetic may contribute to motor blocade of Lower extremities and may contribute to developing pressure sores in heels. If motor blockade persists after decreasing concentration need to rule out for SPINAL HEMATOMA formation or migration of catheter.
NAUSEA /VOMITING: 45-80%
Because of migration of opioids within CSF to the area postrema in the Medulla, that is the center of vomit.
PRURITUS: 66%
Associated with histamine release or activation of itch center in medulla.
RESPIRATORY DEPRESION:
Respiratory depression associated with use of opioids is not higher when it is used Neuroaxial than when used systemic.
Neuroaxial use of lypohilic opiods is considered to cause less delayed respiratory depression than hydrophylic opoids, although lipophilic opioids may be associated with significant early respiratory depression.
Risk factors for respiratory depression are: use of high dose opioid, elderly patient, if systemic opioids or sedatives are also administered, prolonged extensive surgery and other comorbidities.
URINARY RETENSION: 70-80%
Decreases detrussors muscle strength due to opiod action in spinal cord. Epidural administration of local anesthetics can also cause urinary retention in 10-30%.
BENEFITS OF PCEA:
1 . Decrease Pathophysiologic response to surgery that may be associated with reduction in mortality and morbidity compared with analgesia with systemic opioids.
2. Earlier return of GI function.
3. Decrease pulmonary complication, use of spirometer.
4. Thoracic epidural decreases incidence of MI possibly by attenuating the stress response and hypercoagulability, improving analgesia and improving coronary blood flow.
5. some studies suggest decrease incidence of DVT/ PE and graft failure.
RISKS:
1.
Hematoma
2.
Abcess
3.
Migration of the catheter to a vessel: administration of epinephrine in a very low concentration throught the catheter produces tachycardia and helps with diagnose.
4.
Migration of the catheter to subdural space: can produce intense blockade and can be prevented with aspiration of the catheter before the administration of solution.