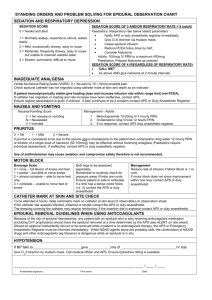
Epidural Analgesia Care Plan
advertisement
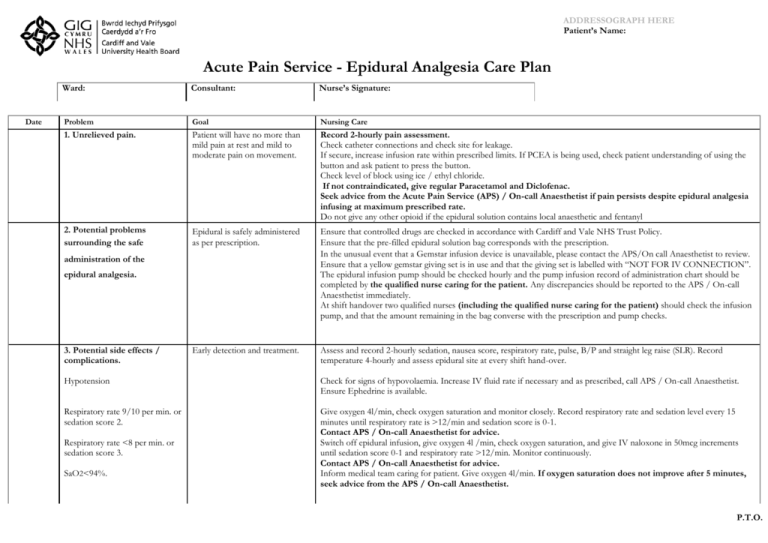
ADDRESSOGRAPH HERE Patient’s Name: Acute Pain Service - Epidural Analgesia Care Plan Date Ward: Consultant: Nurse’s Signature: Problem Goal Nursing Care 1. Unrelieved pain. Patient will have no more than mild pain at rest and mild to moderate pain on movement. Record 2-hourly pain assessment. Check catheter connections and check site for leakage. If secure, increase infusion rate within prescribed limits. If PCEA is being used, check patient understanding of using the button and ask patient to press the button. Check level of block using ice / ethyl chloride. If not contraindicated, give regular Paracetamol and Diclofenac. Seek advice from the Acute Pain Service (APS) / On-call Anaesthetist if pain persists despite epidural analgesia infusing at maximum prescribed rate. Do not give any other opioid if the epidural solution contains local anaesthetic and fentanyl 2. Potential problems surrounding the safe Epidural is safely administered as per prescription. Ensure that controlled drugs are checked in accordance with Cardiff and Vale NHS Trust Policy. Ensure that the pre-filled epidural solution bag corresponds with the prescription. In the unusual event that a Gemstar infusion device is unavailable, please contact the APS/On call Anaesthetist to review. Ensure that a yellow gemstar giving set is in use and that the giving set is labelled with “NOT FOR IV CONNECTION”. The epidural infusion pump should be checked hourly and the pump infusion record of administration chart should be completed by the qualified nurse caring for the patient. Any discrepancies should be reported to the APS / On-call Anaesthetist immediately. At shift handover two qualified nurses (including the qualified nurse caring for the patient) should check the infusion pump, and that the amount remaining in the bag converse with the prescription and pump checks. Early detection and treatment. Assess and record 2-hourly sedation, nausea score, respiratory rate, pulse, B/P and straight leg raise (SLR). Record temperature 4-hourly and assess epidural site at every shift hand-over. administration of the epidural analgesia. 3. Potential side effects / complications. Hypotension Check for signs of hypovolaemia. Increase IV fluid rate if necessary and as prescribed, call APS / On-call Anaesthetist. Ensure Ephedrine is available. Respiratory rate 9/10 per min. or sedation score 2. Give oxygen 4l/min, check oxygen saturation and monitor closely. Record respiratory rate and sedation level every 15 minutes until respiratory rate is >12/min and sedation score is 0-1. Contact APS / On-call Anaesthetist for advice. Switch off epidural infusion, give oxygen 4l /min, check oxygen saturation, and give IV naloxone in 50mcg increments until sedation score 0-1 and respiratory rate >12/min. Monitor continuously. Contact APS / On-call Anaesthetist for advice. Inform medical team caring for patient. Give oxygen 4l/min. If oxygen saturation does not improve after 5 minutes, seek advice from the APS / On-call Anaesthetist. Respiratory rate <8 per min. or sedation score 3. SaO2<94%. P.T.O. Date Problem Goal Nursing Care 3. Potential side effects / complications (continued) Opioid-induced itching. Early detection and treatment. Give IV Naloxone 50mcg, repeat when necessary, if problem remains unresolved, seek advice as the prescription may need amending. Nausea and vomiting. Assess for nausea / vomiting every 2 hours and record on observation chart. Give anti-emetic (see Acute Pain Service Adult Guidelines Nausea and Vomiting Protocol - Appendix 1). Motor loss in limbs. Ask the patient to straight leg raise (SLR) both legs 2-hourly and record on observation chart. Call APS / On-call Anaesthetist if unable to SLR either leg. Check pressure areas. Epidural catheters must be removed within 5 days of insertion unless the Acute Pain Service stipulate otherwise. Epidural site / space infection. Epidural site should be covered with a transparent IV 3000. A window should be made in 4 inch Mefix and placed over and around the dressing. The epidural catheter should be secured up the back and over the patient's shoulder. The filter should be secured to the front of the patient over gauze swabs. Change bags using no touch technique. At each shift change, check epidural site (ESC) for pus, inflammation, tenderness or leakage and record on observation chart and nursing care evaluation. If any of the above is present, contact the APS / On-call Anaesthetist to review. If the epidural catheter is to be removed - See 4. Send tip and swab from site for C+S. The patient will be reviewed regularly by the APS until the problem has resolved. If an epidural site infection is suspected, then Vancomycin or Teicoplanin should be started along with either a Cephalosporin or Ciprofloxacin. This treatment should be reviewed when the C+S results are available. If an epidural site infection is confirmed, then antibiotic treatment should be commenced as per Microbiology Department advice. If the epidural site becomes exposed, the epidural catheter should be removed - See 4. Contact the APS / On-call Anaesthetist to review. If the dressing becomes loose or fluid pools beneath it, the site must be redressed. ** Use an aseptic technique and carefully clean the site using forceps, sterile swabs and sterile 0.9% saline, rubbing in a circular motion from the centre to the periphery. ( +/-) Potential displacement of epidural catheter. Ensure the filter is in situ and all connections are secure. If they are not, seek immediate advice from the APS/ On-call Anaesthetist. Use aseptic technique to remove epidural catheter. Clean the epidural site with sterile normal saline and apply a transparent IV 3000 dressing. Observe epidural site for 3 days after removal for potential infection. If patient is discharged before the end of this 3 day period, the discharging nurse must ensure that either a community nurse conducts a day 3 check, or if appropriate, the patient/carer is educated to check the site. Ensure the patient has been provided with a written epidural patient information leaflet. Suspected local anaesthetic toxicity Early detection and treatment Observe patient for any signs of circum-oral numbness, dizziness, light-headedness, fitting, twitching, drowsiness, ringing in the ears (tinnitus), respiratory arrest, un-consciousness. If any of the above occur stop infusion immediately, contact patients medical team for review, if appropriate contact arrest team, APS/On-call Anaesthetist to review. Guidelines for the management of local anaesthetic toxicity can be found in the acute pain guidelines, page 23 section 5.12. Date Problem Goal Nursing Care 3. Potential side effects / complications (continued) a) Epidural site becomes exposed. or b) Epidural filter becomes disconnected. No epidural site infection. The epidural catheter should be removed, however the guidance outlined in 4. regarding the timing of the catheter removal should be followed. Whilst waiting to safely remove epidural catheter: a) Aseptically clean and redress the epidural site with an IV3000 dressing. Use technique detailed previously on page 2.** b) Do not reconnect filter. Stop infusion and wrap end of catheter in sterile gauze. Contact APS / On-call Anaesthetist who will connect new filter until line can be removed. 4. Problems related to the removal of the epidural catheter. At least 12 hours should elapse between epidural catheter removal and the last prophylactic dose of Low Molecular Weight Heparin (LMWH) e.g. Enoxaparin (Clexane) 20mg - 40 mg. If the patient is receiving a therapeutic dose of LMWH e.g. Enoxaparin >40mg, 24 hours should elapse between the last dose and epidural catheter removal. At least 4 hours should elapse between last dose of Mini-hep and epidural catheter removal. The next dose of LMWH (e.g. Enoxaparin) or Mini-hep should not be administered for at least 4 hours following epidural catheter removal. At least 18 hours should elapse between the removal of the epidural catheter and the last dose of rivaroxaban. The next dose of rivaroxaban should not be administered for at least 6 hours following the removal of the epidural catheter If patient is receiving a concurrent intravenous heparin infusion contact APS and see APS Protocols Section 5.10. Clopidogrel or Warfarin should NOT be administered whilst a patient is receiving epidural analgesia. No haematoma in epidural space. Safe and easy removal of catheter. * If epidural site is red or if pus is present and an epidural infection is suspected or has been confirmed: Infection at site of epidural is avoided or prevented from worsening. Position patient in a lateral lying position or sitting on the edge of bed, with back curved forward to increase the space between vertebrae and facilitate easy removal. Check markings of catheter after removal to ensure catheter is intact and record in nursing records. Once epidural catheter has been removed, clean the epidural site with sterile normal saline and apply a transparent IV 3000 dressing. Remove epidural catheter immediately, regardless of when last dose of LMWH or Mini-hep was administered. N.B. However, if patient has a Coagulopathy or is receiving an IV Heparin Infusion - DO NOT REMOVE - Contact APS / On-call Anaesthetist. See APS Protocols - Section 5.10. In accordance with the Cardiff and Vale infusion device policy training and assessment in the use of epidural infusion devices is mandatory for ANY nurse caring for a patient with epidural analgesia. University Hospital Llandough: Acute Pain Service: bleep 4560. Out of hours, On-call Anaesthetist: bleep 4800 should be contacted. University Hospital of Wales: Acute Pain Service: bleep 5414. Out of hours, the Obstetric On-call Anaesthetist: bleep 5101 should be contacted. GB/APS/Sep/2009