Live donor kidney transplantation across a positive flow crossmatch
advertisement
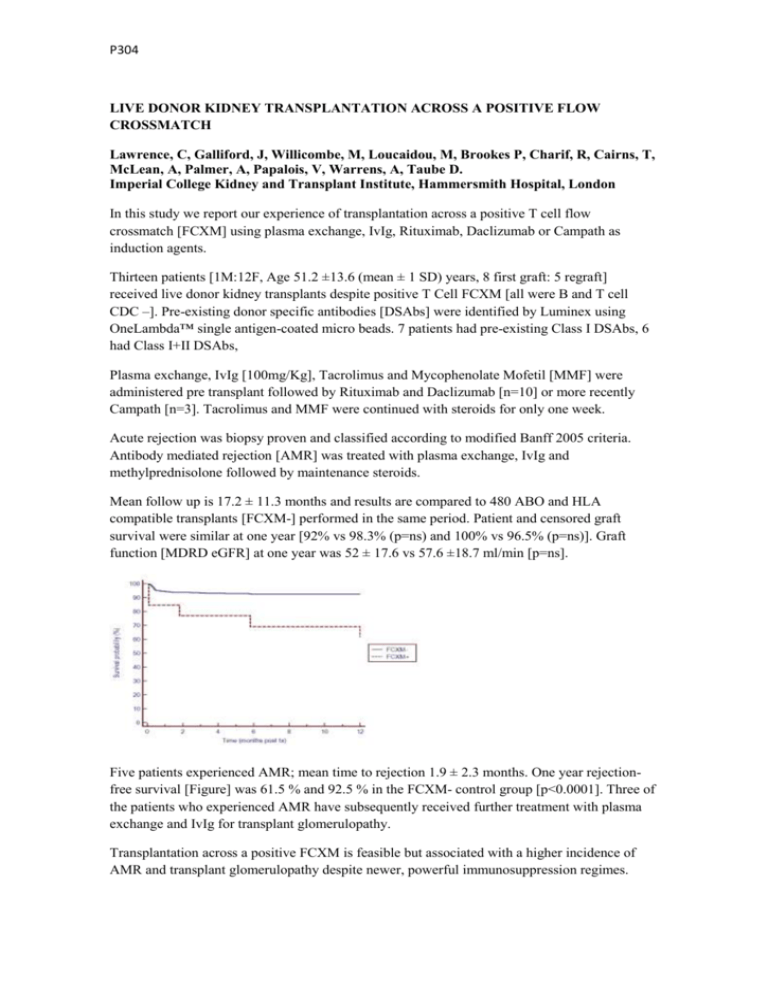
P304 LIVE DONOR KIDNEY TRANSPLANTATION ACROSS A POSITIVE FLOW CROSSMATCH Lawrence, C, Galliford, J, Willicombe, M, Loucaidou, M, Brookes P, Charif, R, Cairns, T, McLean, A, Palmer, A, Papalois, V, Warrens, A, Taube D. Imperial College Kidney and Transplant Institute, Hammersmith Hospital, London In this study we report our experience of transplantation across a positive T cell flow crossmatch [FCXM] using plasma exchange, IvIg, Rituximab, Daclizumab or Campath as induction agents. Thirteen patients [1M:12F, Age 51.2 ±13.6 (mean ± 1 SD) years, 8 first graft: 5 regraft] received live donor kidney transplants despite positive T Cell FCXM [all were B and T cell CDC –]. Pre-existing donor specific antibodies [DSAbs] were identified by Luminex using OneLambda™ single antigen-coated micro beads. 7 patients had pre-existing Class I DSAbs, 6 had Class I+II DSAbs, Plasma exchange, IvIg [100mg/Kg], Tacrolimus and Mycophenolate Mofetil [MMF] were administered pre transplant followed by Rituximab and Daclizumab [n=10] or more recently Campath [n=3]. Tacrolimus and MMF were continued with steroids for only one week. Acute rejection was biopsy proven and classified according to modified Banff 2005 criteria. Antibody mediated rejection [AMR] was treated with plasma exchange, IvIg and methylprednisolone followed by maintenance steroids. Mean follow up is 17.2 ± 11.3 months and results are compared to 480 ABO and HLA compatible transplants [FCXM-] performed in the same period. Patient and censored graft survival were similar at one year [92% vs 98.3% (p=ns) and 100% vs 96.5% (p=ns)]. Graft function [MDRD eGFR] at one year was 52 ± 17.6 vs 57.6 ±18.7 ml/min [p=ns]. Five patients experienced AMR; mean time to rejection 1.9 ± 2.3 months. One year rejectionfree survival [Figure] was 61.5 % and 92.5 % in the FCXM- control group [p<0.0001]. Three of the patients who experienced AMR have subsequently received further treatment with plasma exchange and IvIg for transplant glomerulopathy. Transplantation across a positive FCXM is feasible but associated with a higher incidence of AMR and transplant glomerulopathy despite newer, powerful immunosuppression regimes.