Early pancreas graft failture after simultaneous pancreas kidney
advertisement

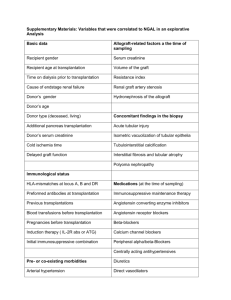
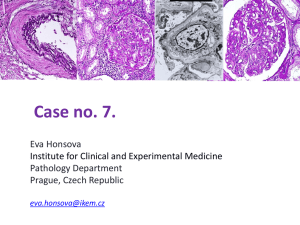
EARLY PANCREAS GRAFT FAILURE AFTER SIMULTANEOUS PANCREAS KIDNEY TRANSPLANTATION H. de Kort1, M.J.K. Mallat3, C. van Kooten3, E. de Heer1, S.H. Brand-Schaaf2, A.M. v.d. Wal1, D.L. Roelen2, J.A. Bruijn1, F.H. Claas2, H.W. de Fijter3, I.M. Bajema1 Department of Pathology1, Immunohematology and Blood Transfusion2, and Nephrology3 Leiden University Medical Center, Leiden, the Netherlands Objectives: Pancreas transplantation, primarily performed as simultaneous pancreas kidney transplantation (SPKT), is a well-established cure for diabetes. Many improvements were made since the first pancreas transplantation in 1966, resulting in a long-term survival advantage. However, SPKTs are still faced with both immunological and non-immunological graft loss. Graft failure within 1 year is worse for the pancreas than for the kidney in SPKT. Early loss of the pancreas graft is clinically mostly attributed to technical failure, encompassing loss through vascular thrombosis, anastomotic leaks, bleeding, pancreatitis, or infection. Until now, there has been little attention for the role of antibody-mediated rejection (AMR) in pancreas graft loss. The aim of the present study was to investigate how many early pancreas graft losses within 1 year after transplantation were due to AMR. Methods: At Leiden University Medical Center, a total of 256 pancreas transplantations were performed between 1985 and February 2010, of which 59 resulted in graft failure and transplantectomy. Fourty-two failed within 1 year, and we were able to include 33 SPKT pancreata within this study (excluded were patients with pancreas after kidney transplantation or pancreas transplantation alone (n=3), patients with graft loss due to post transplant lympho-proliferative disease (n=2), and tissue samples with extensive damage unsuitable for Banff scoring (n=4)). Immunohistochemistry for C4d, CD3, CD20, CD68, BK-virus, and CMV was performed on paraffin-embedded tissue samples. HE-slides were scored according to the Banff ‘08 working proposal for classification. Histological components scored for were; active septal inflammation, (peri)neural inflammation, ductitis, venulitis, interacinar capillaritis, acinar inflammation, acinar cell injury/ necrosis, intimal arteritis, necrotizing arteritis, and transplant arteriopathy. In most cases, pre-transplantation and post-transplantectomy (27 out of 33) DSA serology results were available or additional tests were performed. Results: C4d-staining was negative in 19 cases, focally positive in 6 cases, and diffusely positive in 8 cases. DSA were found after transplantectomy in 8 out of 27 patients, none of the patients had DSA prior to transplantation. In 4 patients both DSA after transplantation and diffuse C4d staining in the excised pancreas graft were found, which established the diagnosis of a true AMR in these 4 patients. There were 14 patients without C4d depositions in their lost grafts and no DSA detected after transplantectomy: in these patients the graft was lost due to other causes than AMR. There were 9 patients with a suspected AMR in their lost grafts: they either had DSA alone (i.e. in the absence of C4d positivity), diffuse C4d positivity without DSA, or focal C4d positivity either with or without DSA. True AMR, diffuse C4d positivity, or DSA on their own correlated with interacinar capillaritis. True AMR was significantly correlated with the total number of rejection episodes. DSA positivity was also significantly correlated with acinar inflammation and (peri)neural inflammation. Immunohistochemical parameters CD3, CD20 and CD68 did not contribute to the diagnosis AMR. All grafts were negative for BK-virus and CMV. Of the 4 true AMR patients, 3 lost their kidney graft on average 1.5 months prior to their pancreas and 1 lost his kidney 4 months after the pancreas was lost. Conclusions: In 4 out of the 33 pancreas graft losses included in this study, true AMR was found characterized by presence of DSA, diffuse C4d staining patterns and with interacinar capillaritis as a prominent histological parameter. Our finding provides evidence that AMR can be the cause of early pancreas graft loss. Furthermore, a substantial number of the pancreas transplantectomies were suspected for AMR, for instance on the basis of focal C4d deposition, either with or without DSA. AMR as a cause for early graft loss in pancreas transplantation is an important differential diagnosis of technical failure. Early recognition of AMR might provide means for therapeutic intervention, to prevent graft loss.