G2(T) Detection of donor specific antibodies predicts antibody
advertisement
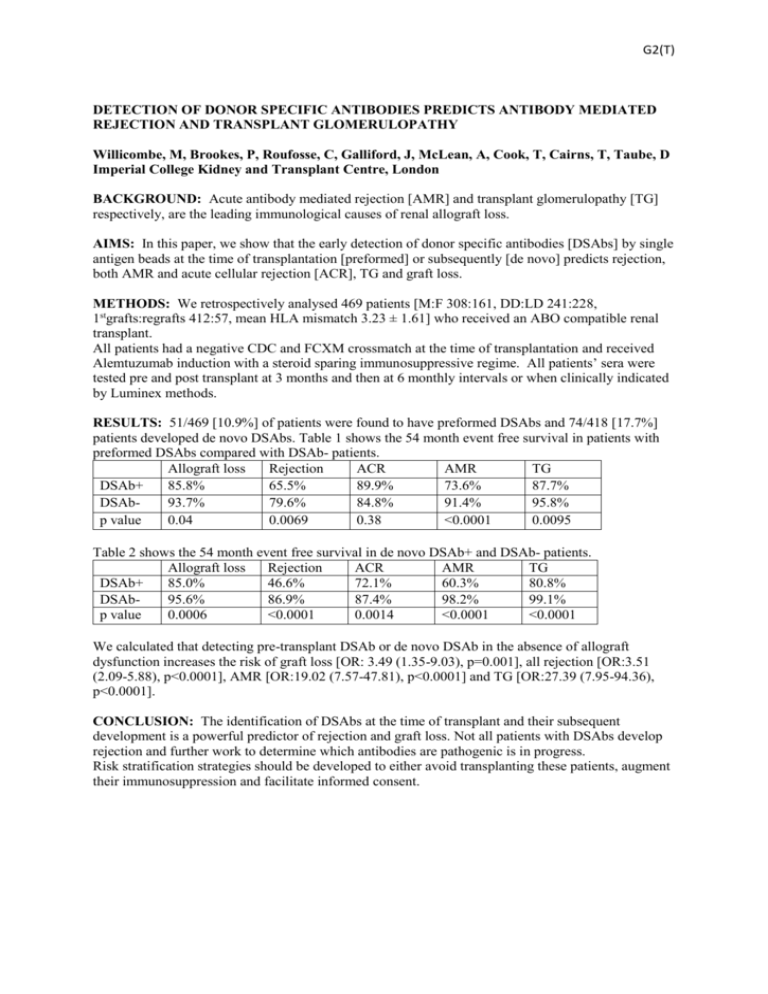
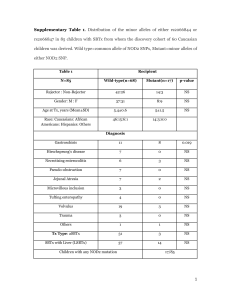
G2(T) DETECTION OF DONOR SPECIFIC ANTIBODIES PREDICTS ANTIBODY MEDIATED REJECTION AND TRANSPLANT GLOMERULOPATHY Willicombe, M, Brookes, P, Roufosse, C, Galliford, J, McLean, A, Cook, T, Cairns, T, Taube, D Imperial College Kidney and Transplant Centre, London BACKGROUND: Acute antibody mediated rejection [AMR] and transplant glomerulopathy [TG] respectively, are the leading immunological causes of renal allograft loss. AIMS: In this paper, we show that the early detection of donor specific antibodies [DSAbs] by single antigen beads at the time of transplantation [preformed] or subsequently [de novo] predicts rejection, both AMR and acute cellular rejection [ACR], TG and graft loss. METHODS: We retrospectively analysed 469 patients [M:F 308:161, DD:LD 241:228, 1stgrafts:regrafts 412:57, mean HLA mismatch 3.23 ± 1.61] who received an ABO compatible renal transplant. All patients had a negative CDC and FCXM crossmatch at the time of transplantation and received Alemtuzumab induction with a steroid sparing immunosuppressive regime. All patients’ sera were tested pre and post transplant at 3 months and then at 6 monthly intervals or when clinically indicated by Luminex methods. RESULTS: 51/469 [10.9%] of patients were found to have preformed DSAbs and 74/418 [17.7%] patients developed de novo DSAbs. Table 1 shows the 54 month event free survival in patients with preformed DSAbs compared with DSAb- patients. Allograft loss Rejection ACR AMR TG DSAb+ 85.8% 65.5% 89.9% 73.6% 87.7% DSAb93.7% 79.6% 84.8% 91.4% 95.8% p value 0.04 0.0069 0.38 <0.0001 0.0095 Table 2 shows the 54 month event free survival in de novo DSAb+ and DSAb- patients. Allograft loss Rejection ACR AMR TG DSAb+ 85.0% 46.6% 72.1% 60.3% 80.8% DSAb95.6% 86.9% 87.4% 98.2% 99.1% p value 0.0006 <0.0001 0.0014 <0.0001 <0.0001 We calculated that detecting pre-transplant DSAb or de novo DSAb in the absence of allograft dysfunction increases the risk of graft loss [OR: 3.49 (1.35-9.03), p=0.001], all rejection [OR:3.51 (2.09-5.88), p<0.0001], AMR [OR:19.02 (7.57-47.81), p<0.0001] and TG [OR:27.39 (7.95-94.36), p<0.0001]. CONCLUSION: The identification of DSAbs at the time of transplant and their subsequent development is a powerful predictor of rejection and graft loss. Not all patients with DSAbs develop rejection and further work to determine which antibodies are pathogenic is in progress. Risk stratification strategies should be developed to either avoid transplanting these patients, augment their immunosuppression and facilitate informed consent.