Negative pressure pulmonary edema
advertisement

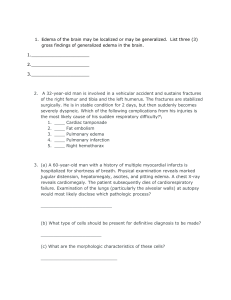
Michelle Torres 1/7/09 CASE: 30 y.o. male with right thyroid mass who underwent right thyroid lobectomy. Patient with h/o hypertyroidism and hyperlipidemia, otherwise healthy. Surgery was uneventful. However, after extubation, patient starting biting on his tongue and lip, and starting coughing blood-tinged secretions. He was suctioned after an oral airway was placed, and he was taken to the PACU. In the PACU, patient appeared to be tachypneic and was using his accessory muscles of respiration. Rales were present bilaterally on physical exam, and he was coughing up pinkish secretions. He satted in high 80s on 5L FM, which was subsequently increased to 10L FM with no improvement. Sat dropped to as low as 77%. ABG was performed: pH 7.26, pCO2 51, pO2 54, base excess -5, bicarb 22.4, O2 sat 82.9%. Pre-op CXR: no active cardiopulmonary disease CXR in PACU: Hazy diffuse lung opacification likely represents noncardiac edema Why would a fairly healthy young male have hypoxia after an uneventful right thyroid lobectomy? NEGATIVE PRESSURE PULMONARY EDEMA (NPPE) What is the cause of NPPE? Type I: acute upper airway obstruction - LARYNGOSPASM (causes 50% of cases in adults) - epliglottitis/croup (causes 75% of cases in pediatric population) - biting on endotracheal tube/LMA - strangulation - hematoma - foreign body aspiration - hiccups - goiter Type II: occurs after relief of a chronic obstructive process ex: laryngeal CA s/p surgery (except laryngectomy) obstructive sleep apnea with correction obstructive goiter undergoing thyroidectomy Pathophysiology: -> sudden high negative intrathoracic pressure, which causes fluid exudate to enter the lungs 1. acute glottic closure -> patient continues to inspire against a closed glottis 2. high negative intrathoracic pressure -> increased venous return to right heart and pulmonary arteries 3. volume expansion -> high arteriole/capillary fluid pressures -> transudation into alveolar space 4. hypoxic vasoconstriction of pulmary and systemic arterioles -> Increased SBP and afterload 5. hypoxia -> catecholamine release -> increased peripheral resisance ---> increased fluid volume within thoracic cavity and unbalanced transmembrane pressures in alveoli 1 Michelle Torres 1/7/09 Mortality rate varies from 10-40% Most cases resolve within 24 hours, however some take several days to weeks. Who is at risk? patients undergoing surgeries involving the upper aerodigestive tract (because more likely than other procedures to cause laryngospasm secondary to laryngeal irritation) -> upper GI endoscopy -> general otolaryngologic, nasal, and paranasal sinus surgery athletic men (because can generate higher intrathoracic pressures and maintain periods of apnea longer) Treatment? maintain airway supplemental O2 gentle diuresis, fluid restriction continuous positive pressure ventilation or even intubation depending on the severity monitored setting steroid use to lessen the pulmonary damage is controversial How do you prevent it? (measures to prevent laryngeal stimulation) topical anesthesia on larynx prior to intubation in high risk groups IV lidocaine prior to extubation throat pack, careful oropharyngeal suctioning extubation in stage 1 anesthesia (not 2, when patients are more likely to go into laryngospasm) Differential diagnosis: aspiration pneumonia What happened to the patient? Patient was placed on 10L NRB, and sats improved to mid 90s. He was also given a dose of lasix 10mg IV, with UOP of 1100cc in the PACU. Patient was titrated down to 5L FM, and was able to maintain sats in the mid-90s. Later on that evening in the floor, patient did not require any more oxygen supplementation, and he was satting in the mid90s. He was subsequently discharged the next day. References: Chuang YC, Wang CH, Lin YS. Negative pressure pulmonary edema: report of three cases and review of the literature. Eur Arch Otorhinolaryngol. 2007 Sep;264(9):1113-6. Epub 2007 Jun 28. Lang SA, Duncan PG, Shephard DA, Ha HC. Pulmonary oedema associated with airway obstruction. Can J Anaesth. 1990 Mar;37(2):210-8. Westreich R, Sampson I, Shaari CM, Lawson W. Negative-pressure pulmonary edema after routine septorhinoplasty: discussion of pathophysiology, treatment, and prevention. Arch Facial Plast Surg. 2006 Jan-Feb;8(1):8-15. 2