Proteinuria
advertisement

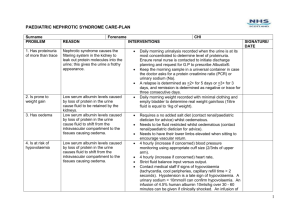
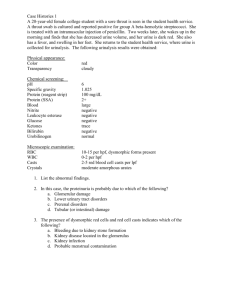
Measurement of Protein in Urine Samples Proteinuria The kidney glomerulus acts as an ultrafiltration unit, allowing passage of water, electrolytes and small organic molecules such as glucose out of its semi-permeable membrane, but not blood cells and large protein molecules. The filtrate produced by the glomeruli of both kidneys amounts to about 170 liters per day; this rate is termed the glomerular filtration rate. Over 99 percent of the glomerular filtrate is reabsorbed during passage through the tubules, with most of the reabsorption taking place in the proximal tubules. Albumin is an important protein constituent of the blood; it makes up over half of the total protein in circulation and has an important osmoregulatory role as well as being involved in the transport of small molecules such as fatty acids, steroid hormones and drugs. Because the albumin molecule is relatively small, it is often among the first proteins to enter the urine after glomeruli are damaged. Therefore, even minor kidney dysfunction is detectable with proper diagnosis of micoralbuminuria. Reduced albumin level in the blood causes fluid retention and swelling that is first noticeable in the hands, lower legs, and feet. In more serious cases, the abdomen and face may swell. Nephrotic Syndrome Nephrotic syndrome is a condition marked by very high levels of protein in the urine (proteinuria); low levels of protein in the blood; swelling, especially around the eyes, feet, and hands; and high cholesterol. Nephrotic syndrome results from damage to the kidneys' glomeruli and can occur with many diseases, including the kidney diseases caused by diabetes mellitus, but some causes are unknown. Prevention of nephrotic syndrome relies on controlling these underlying diseases. Nephrotic syndrome may go away once the underlying cause, if known, has been treated. In children, 80 percent of cases of nephrotic can be successfully treated. However, in adults, there are a number of underlying causes, including diabetes. In some cases, the kidneys may gradually lose their ability to filter wastes and excess water from the blood. If kidney failure occurs, the patient will need dialysis or a kidney transplant. Foamy urine and swelling of the abdomen (oedema) are two signs of proteinuria that become more evident as the disease progresses. Excess protein can cause the urine to foam in water. This occurs because protein changes the surface tension between urine and water. Oedema usually only occurs in nephrotic syndrome. Because the albumin molecule is relatively small, it is often among the first proteins to enter the urine after glomeruli are damaged. Therefore, even minor kidney dysfunction is detectable with proper diagnosis of micoralbuminuria. Reduced albumin level in the blood causes fluid retention and swelling that is first noticeable in the hands, lower legs, and feet. In more serious cases, the abdomen and face may swell. Normal Protein excretion Albumin excretion can be determined by timed urine collection e.g. over a 24 hr period. The presence of albumin in the urine is normal and we can use a sensitive assay method to show that up to 0.03g per 24 hours is lost by a normal individual. A normal person produces between 1 to 2 litres of urine per day. What is the range of protein concentration in the urine of a normal individual? Calculation: Maximum concentration 0.03 g (= 30mg or 30,000 g) per 24hr or per litre urine = 30 mg/litre (or 30 g/ml) (1 litre = 1000 ml, 1 mg = 1000 g) Microalbuminuria (could be benign or an indication of progressive kidney failure) 0.03 to 0.3 g protein per 24 hr What is the maximum urinary concentration of protein expected? Nephrotic Syndrome Between 0.3 g and 5 g protein excreted per day Calculate the range of concentrations expected Bradford’s Reagent- how does it work? The structure of Coomassie Brilliant Blue is shown in the Study Session 1 handout Note that the dye has hydrophobic regions (lots of aromatic rings) and also basic and acidic groups. The dye is dissolved in acid and so at low pH only a very small amount is present as the anionic species but it is this anionic form which interacts with protein to give a form of the dye which is intensely blue. The more dye binds to protein , the more dye is converted to its anionic form (mass action effect). The interaction of protein and dye is mainly with the arginine residues, which are strongly basic amino acids (look up the structure of arginine in a textbook). Different proteins have different arginine contents and so the intensity of the colour will be dependent on the amino acid composition of the protein as well as concentration. However the majority of proteins contain a substantial amount of arginine residues. Albumin is used as a standard because it has the amino acid composition of a typical protein. D R Davies Oct 2005