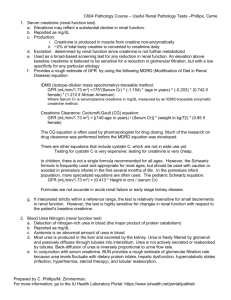
27 Apr 2010- Nephrotic Syndrome in Children
advertisement
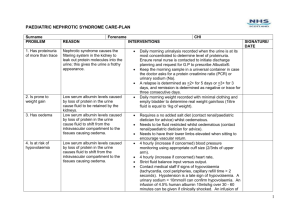
Diagnosing nephrotic syndrome Principles of management Case study of a severely affected child Complications Proteinuria Hypoalbuminaemia Oedema (periorbital, ascites, pleural effusions) Commoner in boys and atopic families. Often precipitated by respiratory infections. Dipstick test positive Check urine protein/creatinine ratio in an early morning sample. Protein should not exceed 20mg/mmol of creatinine. Transient proteinuria can occur during a febrile illness or after exercise. Orthostatic proteinuria – check early morning and daytime urine P:C ratios. Cause is largely unknown. Idiopathic – over 80% minimal change, 20% FSGS Secondary to systemic diseases eg HSP, SLE, infections eg malaria Congenital (rare, severe) Age 1-10 years Normal BP Normal renal function Normal complement levels No macroscopic haematuria These children normally respond to steroids. Atypical features or non-responders need consideration for renal biopsy Check bloods – FBC, U+Es, creatinine, LFTs, ASOT, C3/C4, Varicella titres Urine protein/creatinine ratio and urine culture Urine dip for blood/glucose Urinary sodium concentration BP Varicella status/hep B status. 9 year old boy Known nephrotic syndrome, steroid dependent Unwell for 1 week with cough and cold Parents test urine dipstick for protein daily as frequent previous relapses – 4+ Initial periorbital oedema, now distended abdomen and groin oedema, ankle oedema and breathlesness/wheeze on lying flat. Already taking long term daily prednisolone treatment Started mycophenylate a few days earlier in OPD, as relapses becoming more frequent Developed loose stool post admission – s/e of medication – exacerbating hypovoloaemia BP stable, oliguric Hgb 14.1 wcc 32 urea 10.5, creat 47, albumin <10 Went into remission after approx 1 week Prednisolone continued, mycophenylate stopped IV albumin with furosemide Prophylactic penicillin Ranitidine to help gut s/es. Daily weights High dose prednisolone, weaned over several weeks Albumin if hypovolaemic (not just for low albumin) Diuretics may be needed to help treat peripheral oedema – but caution if hypovolaemic. Penicillin V tends to be given in relapses – increased risk of infection including cellulitis Fluid restriction Remission = trace or neg protein on dip More specialised drugs – levamisole, cyclophosphamide, mycophenylate Hypovolaemia (despite peripheral oedema) Infection – urinary loss of immunoglobulin Thrombosis Hyperlipidaemia Most (>90%) children respond to prednisolone within 2-4 weeks. Can be an isolated episode, lead to infrequent or frequent relapses. Most children grow out of nephrotic syndrome. GENERAL CONSIDERATIONS DURING FOLLOW UP* For children on long-term steroids: 1) Monitor BP 2) Monitor growth (including bone age and pubertal stage where appropriate) 3) Monitor weight – dietetic review where appropriate 4) Glycosuria / HbA1c 5) Bone mineral density / calcium supplements 6) Ophthalmology review 7) VACCINATION Pneumococcal: recommended for all children with NS. Varicella: consider in varicella negative children with frequent relapses.Aim to administer vaccine when prednisolone dose is low. * Guideline for the management of nephrotic syndrome, Dr J Beattie, Royal Hospital for Sick Children, Yorkhill division, Greater Glasgow Oct 07 www.clinicalguidelines.scot.nhs.uk


![Detection of proteinuria[1]](http://s3.studylib.net/store/data/007549979_2-02bd2c299a632d6a55125f2f2a73449c-300x300.png)