Toe walking hand-out (Autism)
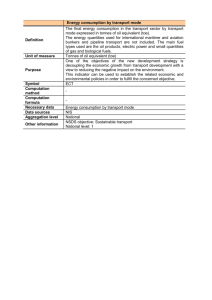
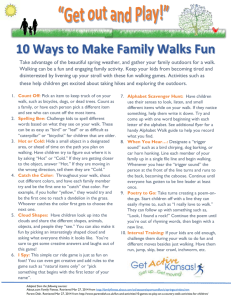
advertisement

Toe Walking in Children with Autism Written by Catherine Yoell, BScPT, 2001, Centre for Ability What is Toe Walking? Toe walking is defined as walking on the tiptoes or without the heels touching the ground, most of the time. Toe walking can be a normal stage in learning to walk. Many children walk on their toes at some point, however, they usually outgrow it by about 18 months of age. Toe walking is commonly seen in children with autism. These children are usually able to walk with their feet flat on the ground, put prefer to walk on their toes. For most children with autism, toe walking is not a problem, however, it tends to be quite “obvious” or “noticeable”, and therefore we focus on it. Toe walking itself does not harm the child. What Causes Toe Walking? Toe walking that persists beyond 18 months of age can be due to... Tightness in the Achilles tendon (a.k.a. heel cord) and the calf muscle Habit – this is the way the child has learned to walk “Liking the sensation” of walking on the toes A problem with spatial orientation (not knowing where their body is) and therefore a dislike for “letting go of the ground” Having hypersensitive feet Having poor proprioception (the ability to know where your body is in space) – walking on the toes tightens calf muscles which makes it easier to feel “in control” An inappropriate foot position (i.e. pronated (flat) feet or in-turning or out-turning of the feet) when standing with their heels on the ground. They feel more secure on their tiptoes as it allows them to “lock” all of the muscles in their feet. Why Do Children With Autism Often Walk On Their Toes? The answer to this is not known for sure, however there has been a link established between toe walking and other neurological problems such as delayed speech and fine motor skills. Again, it may be due to enjoying the sensation or having poor proprioception or hypersensitive feet. Is Toe Walking Really A Problem? Toe walking itself is not a problem. However, a child who walks on his or her toes should be seen by a physiotherapist to check if there is tightness in the heel cords and to look at the position of the foot when the child is standing with heels flat on the ground. Toe walking hand-out (Autism), Page 2 of 4 Children who do not have tightness in their heel cords and who have an appropriate foot position do not need to have any treatment. The toe walking tends to bother the parent more than the child – i.e. it is a cosmetic or visible problem but is not harming the child. Children who have tightness in their heel cords should try some stretches to keep this from progressing. Please see the “What Can Be Done” section. Children whose feet are not in an appropriate position when they stand with their heels on the ground (i.e. – pronated feet or feet that turn outward or inward) should be seen by an orthopaedic specialist and may need to have orthotics for their shoes. Can Toe Walking Lead to Problems? Generally, children with autism who walk on their toes have enough flexibility in their heel cords to be able to walk with their feet flat on the ground, but prefer not to. Toe walking itself is not a problem, however, it can lead to some potential problems that should be monitored. It should be emphasized that these problems are often minor and may not be worth the effort to treat them, as children with autism often are not able to tolerate the treatments such as stretching and wearing orthotics. Toe walking can potentially lead to... Tightening of the heel cords – please see the stretches in the “What Can Be Done” section Incorrect foot position (pronated, turned in or turned out) – this can potentially lead to problems at the knees if severe enough. Orthotics may help correct this. What Can Be Done? Remember again that most children with autism who walk on their toes do not need to have it corrected. The toe walking tends to bother the parents more than the child. However, some strategies are: Stretches – if your child has tight heel cords. Active stretches tend to be more effective, however, passive ones may be easier to carry out Proprioceptive Activities – Play games that give firm pressure through the legs such as marching, stomping, and jumping on a trampoline. Toe walking hand-out (Autism), Page 3 of 4 Orthotics – if your child’s foot position needs to be corrected. Passive Stretches With the child in a sitting or lying position, bring the toes up toward the shin. You can do this for 30-60 seconds with the knee straight, then with the knee bent. Have the child sit with their back against the sofa and their legs out straight while they watch their favourite show. Have something for their legs to push up against to keep them straight. Night boots or stretching splints that are worn at night can be made by your Physiotherapist. Active Stretches Sit facing your child with your legs out straight, hold hands and lean back and forth as far as you can. Try singing “Row Your Boat”. Encourage your child to walk up inclines such as steep hills or a slide. Try getting your child to play standing on a sturdy binder or wedge of 10-20º. Have your child push heavy objects such as a grocery cart or heavy doors. Play “the lean game” – stand facing one another (you may need to be on your knees) and put your hands against your child’s hands. Lean forward so that you are both being supported by your hands. Try animal walks with legs straight such as: o An elephant walk – legs straight, arms and head are the trunk. Try to pick things up with the “trunk”. o A bear walk – hands and feet are on the ground, legs straight. Toe walking hand-out (Autism), Page 4 of 4 Are There Any Other Options? If your child has very tight heel cords that are not responding to stretching, then your physiotherapist and orthopaedic specialist may suggest some further treatment such as Botox injections, serial casting, and rarely surgery. Botox – Botox is a type of toxin that temporarily paralyzes part of the heel cord muscle so that it can be stretched out. When the muscle is less tight, the child can walk with the heels down. The child sometimes is put in a stretching cast for a couple of weeks, two weeks after the injection. Serial Casting – Serial casting involves putting a cast on the child’s leg for approximately one week to help stretch the muscle. The cast is taken off for a day and then reapplied two or three more times. Surgery – An orthopaedic surgeon decides if a child needs to have surgery to increase the flexibility of their heel cords. This involves cutting the muscle to make it longer, then putting the child in a cast for a few weeks. Physiotherapy suggestions should be associated with all of these procedures. Other Suggestions: ____________________________ Physiotherapist ______________________________ Date If you have any questions, please ask your physiotherapist!