Diabetes and Altered Mental Status
advertisement

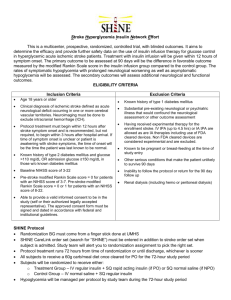
Diabetes and Altered Mental Status Chapter 19 Objectives - Identify the patient taking diabetic medications with altered mental status and the implications of a diabetes history. - State the steps in the emergency medical care of the patient taking diabetic medicine with an altered mental status and a history of diabetes. - Establish the relationship between airway management and the patient with altered mental status. - State the generic and trade names, medication forms, dose, administration, action, and contraindications for oral glucose. - Evaluate the need for medical direction in the emergency medical care of the diabetic patient. - Explain the rationale for administering oral glucose. I. Diabetic Emergencies A. Diabetes Mellitus 1. A metabolic disorder in which the body cannot metabolize glucose. 2. Usually due to the lack of insulin or inadequate insulin production B. Insulin 1. Allows glucose to pass from the blood stream into cell. 2. Produced in the pancreas 3. Production stimulated by increased blood sugar C. Glucose 1. Major source of energy for the body 2. All cells need it to function 3. As important to the brain as oxygen D. Normal blood sugar = 80–120mg/dl E. Hypoglycemia (insulin shock) 1. Low blood sugar (<70mg/dl) F. Hyperglycemia [diabetic ketoacidosis (DKA)] 1. High blood sugar (>200mg/dl) G. Precipitating factors 1. Heredity 2. Obesity 3. Pregnancy 4. Viral infections H. Long term effects on the body 1. Blindness 2. Heart disease 3. Kidney failure 4. Nerve disorders 5. Circulatory disorders I. Type I (Insulin dependent – IDDM) 1. No insulin produced 2. Can significantly shorten life span if not managed 3. Effects on the body are usually more severe than with type II 4. Treated with daily insulin shots J. Type II (Non-insulin dependent – NIDDM) 1. Usually appears later in life 2. Patient produces inadequate insulin or insulin doesn’t function correctly 3. Treated with diet/exercise and/or oral medications 4. Can progress to type I diabetes II. Diabetic Medical Emergencies A. DKA (Diabetic ketoacidosis) 1. Decreased insulin which results in increased blood sugar 2. Slow in onset 3. Mimics dehydration Pathophysiology of Hyperglycemia (DKA) Decreased insulin and/or increased blood sugar Increased sugar in the urine Starving cells Water is pulled into urine Fat and protein breakdown Increased urine output Production of ketones and other acids/byproducts Dehydration Irritability Diabetic coma Death 4. Common causes a. Infection – raises metabolism b. Stress – raises metabolism c. Exercise/diet changes d. Pregnancy e. Some drugs (prescription or street) 5. Pertinent questions (may have to ask family members) a. Do you take insulin or control your diabetes with diet/oral meds? b. Have you taken your insulin/oral meds today? c. Have your meds been changed lately? d. When did you last eat, and how much? e. Have you been unusually stressed? (heat, cold, sickness, physical or emotional stress) f. When did you last take your blood sugar reading and what was it? 6. Signs/symptoms a. Altered LOC b. Skin warm/dry c. Tachycardia d. Kussmaul respirations – Rapid/deep respirations in an attempt to blow off acids (CO2) e. Blood pressure normal or low (dehydration) f. Smell of acetone on the breath (fruity odor) – acids g. ABD pain h. Polydipsia – Thirsty i. Polyphagia – Hungry j. Polyuria – Increased urine output 7. Treatment a. ABC’s, High flow O2 b. Position as per blood pressure c. Rapid transport d. ALS support e. If unsure treat as hypoglycemia B. Hypoglycemia (Insulin shock) 1. Increased insulin which leads to low blood sugar 2. Rapid onset 3. Mimics shock 4. True medical emergency 5. Can be seen in non-diabetic patients Pathophysiology of Hypoglycemia Increased insulin Decreased blood sugar Sugar stores used up Irritability Seizures/Coma/Death Starved brain (brain damage) 6. Common causes a. Too much insulin b. Normal insulin/not enough food c. Starvation d. Alcohol e. Hypothermia f. Exercise g. Tumors of the pancreas h. Liver problems i. ASA overdose 7. Pertinent questions (same as for DKA) a. Do you take insulin or control your diabetes with diet/oral meds? b. Have you taken your insulin/oral meds today? c. Have your meds been changed lately? d. When did you last eat, and how much? e. Have you been unusually stressed? (heat, cold, sickness, physical or emotional stress) f. When did you last take your blood sugar reading and what was it? 8. Signs/symptoms a. Altered LOC (combatitive) b. Skin pale/cool/diaphoretic c. Tachycardia d. Rapid/shallow respirations e. Blood pressure usually normal f. Seizures g. Stroke like symptoms h. Rapid onset 9. Treatment a. ABC’s, High flow O2 b. Oral glucose between cheek and gum c. DO NOT place anything into mouth of patient if they can’t protect their own airway d. Position of comfort e. Rapid transport f. ALS support Major Differences in presentation Hypoglycemia Onset Rapid (minutes) Skin vitals (most obvious) Diaphoretic Respirations Rapid shallow Hyperglycemia Slow (days) Dry Rapid deep (kussmaul) III. Medication A. Oral Glucose 1. Medication Name a. Generic - Glucose, Oral b. Trade - Glutose, Insta-glucose 2. Indications - patients with altered mental status with a known history of diabetes controlled by medication. 3. Contraindications a. Unresponsive. b. Unable to swallow. 4. Medication form - Gel, in toothpaste type tubes 5. Dosage - one tube 6. Administration a. Obtain order from medical direction either on-line or offline. b. Assure signs and symptoms of altered mental status with a known history of diabetes. c. Assure patient is conscious and can swallow and protect their airway. d. Administer glucose. (1) Between cheek and gum. (2) Place on tongue depressor between cheek and gum. e. Perform ongoing assessment. 7. Actions - increases blood sugar 8. Side effects - none when given properly. May be aspirated by the patient without a gag reflex. 9. Re-assessment strategies - if patient loses consciousness or seizes, remove tongue depressor from mouth. IV. Altered Mental Status A. Causes of Altered Mental Status 1. Hypoglycemia 2. Poisoning (Including Alcohol & Drugs) 3. Infection 4. Head Trauma 5. Hypoxia B. Emergency Care of Altered Mental Status 1. Secure airway 2. Ventilate and suction as needed 3. Transport 4. Evaluate potential causes 5. Treat patient as trauma patient if injury cannot be ruled out V. Seizures A. Definition - Sudden change in sensation, behavior, or movement caused by irregular electrical activity of the brain B. Causes of Seizure 1. Toxin (Including drugs and alcohol) 2. Brain tumor 3. Congenital brain defects 4. Trauma 5. Infection/Fever a. #1 cause in pediatric patients 6 months to 3 years old 6. Epilepsy 7. Stroke 8. Hypoglycemia 9. Eclampsia (complication of pregnancy) 10. Hypoxia 11. Unknown C. Information to Obtain 1. What was the patient doing before seizure? 2. What movements were exhibited? 3. Loss of bladder or bowel control? 4. What did the patient do after seizure? 5. Length of episode? D. Emergency care during seizure 1. Place patient on floor 2. Position patient on side 3. Loosen restrictive clothing 4. Remove harmful objects 5. Protect patient from injury; do not hold patient still or place anything in mouth. 6. After seizure subsides: a. protect airway with positioning and suction b. If cyanotic, ventilate with oxygen c. Treat injuries d. Transport E. Status Epilepticus 1. Definition - A life-threatening condition in which the patient has two or more convulsive seizures without regaining consciousness 2. Emergency Care a. Secure the airway b. Ventilate with 100% oxygen c. Request ALS d. Transport immediately VI. Cerebrovascular Accident (CVA) – Stroke A. Pathophysiology 1. Death or injury of brain tissue that is deprived of oxygen. 2. Caused by a blockage (ischemic) or bleeding (hemorrhagic) of a blood vessel in the brain. B. Signs and Symptoms 1. Intoxicated appearance, slurred speech, unconsciousness 2. Severe headache, vision changes 3. One-sided weakness on body 4. Confusion 5. Loss of bowel and/or bladder control 6. Unequal pupils 7. High blood pressure C. Transient Ischemic Attack (TIA) 1. Sometimes called a “mini stroke” 2. Signs and symptoms of a stroke 3. Often resolved before EMS arrival 4. Symptoms resolve without treatment in less than 24 hours 5. Significant risk of having a “full” stroke D. Treatment of stroke patient 1. Prompt transport is critical 2. Identify potential stroke patients and notify the hospital 3. Maintain airway, administer oxygen E. Cincinnati Prehospital Stroke Schedule 1. Facial drooping 2. Arm drift 3. Slurred speech VII. Dizziness and Syncope A. Syncope is a brief loss of consciousness B. It can occur at any age, more common in the elderly C. It may be an indicator of a more serious medical problem D. Causes of Syncope 1. Hypovolemia a. Trauma b. Dehydration 2. Metabolic a. Hypoglycemia b. Stroke c. Seizure 3. Environmental / Toxicological a. Drugs and Alcohol b. Carbon Monoxide c. Panic / Anxiety 4. Cardiovascular a. Fast or slow heart rates b. Electrical system disturbance c. Vagus nerve stimulation E. Assessment of dizziness and syncope 1. Obtain a SAMPLE history 2. Ask about onset time, activities 3. Length of episode 4. Any previous episodes 5. Any medications for this condition 6. Any nausea / vomiting / bowel changes F. Treatment of dizziness and syncope 1. Administer high-concentration oxygen 2. Loosen restrictive clothing 3. Lay patient flat and elevate legs (if no suspected spinal injury) 4. Treat any associated injuries 5. Request ALS and transport