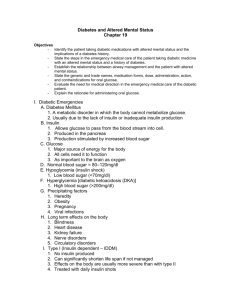
Basic Outline Ch 19 I. Diabetes (pp. 448–458) A. Diabetes mellitus
advertisement

Basic Outline Ch 19 I. Diabetes (pp. 448–458) A. Diabetes mellitus, “sugar diabetes,” or just “diabetes” 1. Decreased insulin production or inability (commonly older patients) to use insulin properly, resulting in high bloodsugar (p. 449) a. B. Person suffering from this condition is a diabetic Diabetic emergencies (p. 450) 1. Hypoglycemia (low blood sugar) a. b. c. d. Caused by the following i. Takes too much insulin (or oral medication used to treat diabetes) ii. Reduces sugar intake by not eating iii. Overexercises or overexerts himself iv. Vomits a meal, emptying stomach of sugar as well as other food Children are more at risk for hypoglycemia than diabetic adults. i. Children can exhaust blood sugar levels by playing hard. ii. Children are less likely to be disciplined about eating correctly and on time. Signs i. Rapid onset ii. Abnormal behavior iii. Very sweaty skin Treatment i. Quick administration of glucose (1) 2. Patient must be conscious and be able to swallow if oral glucose used Hyperglycemia (high blood sugar) a. Caused by a decrease in insulin, which leaves sugar in the bloodstream rather than allowing it to enter the cells b. Unlike hypoglycemia, generally has a slower onset i. Patient experiences increased urination, thirst, and hunger (1) C. May be nauseated and have an acetone-like odor on his or her breath Patient assessment (p. 450) 1. Diabetic emergencies a. To access patient i. Perform initial assessment (identify altered mental status). ii. Perform a focused history and physical exam. (1) History of present episode from patient or bystanders (2) SAMPLE history (3) b. (a) Look for medical identification bracelet or wallet card. (b) Look for medications (insulin and medication to treat diabetes). Perform glucose monitoring if permitted by local protocol. iii. Determine if patient is alert enough to swallow. iv. Determine baseline vital signs. Signs and symptoms associated with diabetic emergency i. Onset of altered mental status (1) After a meal on day patient took prescribed insulin (2) Vomiting a meal on a day took prescribed insulin (3) After unusual amount of physical exercise or work (4) No identifiable predisposing factor D. ii. Intoxicated appearance, staggering, slurred speech, to unconscious iii. Cold, clammy skin iv. Elevated heart rate v. Hunger vi. Uncharacteristic behavior vii. Anxiety viii. Combativeness ix. Seizures Blood glucose meters (pp. 451–455) (Scan 19-2, p. 453) 1. Calibrated and stored according to manufacturer’s recommendations 2. Steps to follow a. Take Standard Precautions. b. Prepare device, including test strip and lancet. c. Cleanse finger with alcohol prep. d. Stick the finger and wipe away the first drop of blood. e. Apply second drop of blood to strip. f. Meter analyzes the sample and provides a reading. g. Less than 60 to 80 milligrams per deciliter in a symptomatic diabetic is typical of hypoglycemia and indicates need for prompt administration of glucose. i. Value less than 50 milligrams per deciliter will usually indicate significant altered mental status. ii. Reading over 120 to 140 milligrams per deciliter indicates hyperglycemia. iii. A reading inconsistent with patient’s symptoms should have EMT question the result. (1) Consider insufficient blood sample, expired strip, not stored properly, meter needs calibration, or device not used properly. E. Calibration and testing on a regular basis are essential. (3) The blood glucose monitor is just one tool and should never be done before a thorough initial assessment. Patient care (p. 455) 1. II. (2) Diabetic emergencies a. Determine all of the following criteria for administration of oral glucose are present: history of diabetes, altered mental status, and is awake enough to swallow b. If criteria met, then administer oral glucose. c. Reassess patient and consult medical direction about administering more oral glucose. d. If patient not awake enough to swallow, treat him or her like any other patient with altered mental status. i. Secure airway, provide artificial ventilations if necessary, and be prepared to perform CPR. ii. Position the patient appropriately. iii. Request an ALS intercept if available. Additional Information on Diabetes (pp. 457–458) A. B. Types of diabetes 1. Type I is usually insulin-dependent 2. Type II is non-insulin-dependent (usually associated with obesity) Hyperglycemia (p. 449) 1. High blood sugar a. Occurs when the diabetic does not produce enough natural insulin to take sugar out of blood and into cells i. Usually occurs due to one of the following: (1) Diabetic hasn’t taken enough insulin (2) Diabetic has forgotten to take insulin ii. C. Diabetic has overeaten (4) Diabetic has an infection that has upset his insulin/glucose balance Body uses other alternate forms of food energies, particularly stored fats, which results in ketones in the blood turning the blood acidic (1) Person will drink large quantities of water to make up for fluid loss through excess urination (2) Leads to a serious condition known as diabetic ketoacidosis Hypoglycemia and hyperglycemia compared (p. 449) 1. Onset—hyperglycemia usually slower 2. Skin 3. a. Hyperglycemic patient often warm, red, and dry b. Hypoglycemic patient cold, pale, moist, or “clammy” Breath a. Hyperglycemic patient often has acetone breath and hypoglycemic patient does not 4. Hyperglycemic patient frequently breathes very deeply and rapidly with a dry mouth, intense thirst, abdominal pain, and vomiting 5. Distinguishing some of the differences in the field may be difficult. a. 6. III. (3) Consult medical direction if questions or concerns. “Sugar (glucose) for everyone” Other Causes of Altered Mental Status (pp. 458–469) (Fig. 19-4, p. 460) (Scan 19-4, p. 464) A. Seizure disorders 1. Common causes (pp. 458–461) a. Adults—failure to take prescribed antiseizure medications b. Infants/children (3 months to 3 years)—febrile seizures 2. 3. Categories (pp. 458–459) a. Toxic—drug or alcohol use, abuse, or withdrawal b. Brain tumor c. Congenital brain defects—defects in the brain d. Infection—swelling and inflammation in the brain e. Metabolic—irregularities in brain body chemistry f. Trauma—head injury g. Idiopathic—spontaneously with unknown cause h. Epilepsy i. Stroke j. Measles, mumps, and other childhood diseases k. Hypoglycemia l. Eclampsia m. Hypoxia (lack of oxygen) n. Heat stroke (resulting from exposure to high temperature) Patient assessment a. Seizure disorders i. Ask the following questions (usually from bystanders): (1) What was the person doing before the seizure started? (2) Exactly what did the person do during the seizure— movement by movement—was there loss of bladder or bowel control? (3) How long did the seizure last? (a) Two or more convulsive seizures without regaining full consciousness and lasting 5 to 10 minutes or more is known as status epilepticus. (4) 4. What did the person do after the seizure? Was he asleep? Was he awake? Was he able to answer questions? (If not sure, use AVPU scale to assess mental status.) Patient care a. Seizure disorders i. Present during the seizure (1) Place patient on floor/ground. (a) ii. 5. IV. If no possibility of spine injury, position patient on side. (2) Loosen restrictive clothing. (3) Remove objects that may harm the patient. (4) Protect the patient from injury, but do not try to hold the patient still during convulsions. After convulsions have ended (1) Protect the airway. (2) If patient is cyanotic, ensure an open airway and provide artificial ventilations with supplemental oxygen. (3) Treat any injuries the patient may have sustained during the convulsions, or rule out trauma (immobilize the neck and spine if trauma suspected). (4) Transport to a medical facility, monitoring vital signs and respirations closely. If patient refuses transportation, try to encourage patient to go to hospital—if he or she still won’t go, then patient should not be left alone and should not drive. Types of Seizure (p. 461) A. Partial seizures 1. Also called focal motor, focal sensory, or Jacksonian a. Simple seizure b. B. ii. May be an aura (sensation such as smell, bright lights, or burst of color) Complex partial seizure (also called psychomotor or temporal lobe) i. Patient confusion, glassy stare, aimless moving about, lip smacking, and chewing or fidgeting with clothing ii. May appear to be drunk or on drugs iii. Not violent but may struggle or fight restraint iv. No loss of consciousness v. May be confusion and no memory of episode vi. Rarely develops into a tonic-clonic seizure Tonic-clonic (also called grand mal) seizure a. Three distinct phases i. Tonic phase—body becomes rigid and stiffens for no more than 30 seconds; breathing may stop; patient may bite tongue; bladder and bowel control lost ii. Clonic phase—body jerks about violently, usually no more than 1 to 2 minutes; patient may foam at mouth and drool; face and lips become cyanotic iii. Postictal phase—begins when convulsions stop; patient may regain consciousness immediately and enter a state of drowsiness and confusion or may remain unconscious; headache is common Absence seizure (also called petit mal) 1. Brief only lasts 1 to 10 seconds a. D. Patient tingling, stiffening, or jerking in just one part of the body Generalized seizures (p. 461) 1. C. i. No dramatic motor activity Stroke (pp. 462–466) 1. Death or injury to brain tissue that is deprived of oxygen a. b. c. Causes i. Blockage of artery that supplies the brain (called ischemic stroke) ii. Bleeding from a ruptured blood vessel in the brain (called hemorrhagic stroke) Signs i. One-sided weakness (hemiparesis)—body weakness is opposite from the side of the brain that is affected ii. Headacheiii. Inability to speak or use words (aphasia is a general term that refers to difficulty in communication) Transient ischemic attack (TIA) i. Patient is confused, weak on one side, and having difficulty speaking but may be acting normal when EMS arrives. (1) d. Initially may look like a stroke ii. Patient is at risk for a full-blown stroke. iii. If patient refuses transport, should be encouraged to be evaluated as soon as possible. Patient assessment (pp. 464–465) i. Cincinnati Stroke Scale (1) (2) (3) Ask patient to grimace or smile (ask that they show their teeth). (a) Normal is to move both sides of face equally (b) Abnormal is unequal movement or no movement Ask patient to close eyes and extend arms straight out in front for 10 seconds. (a) Normal is patient moves both arms at the same time (b) Abnormal is one arm drifts down or does not move at all Ask patient to say something like “The sky is blue in Cincinnati.” ii. e. (a) Normal is clear speech. (b) Abnormal response is slurred speech, wrong words, or no speech at all. Other signs and symptoms (1) Confusion (2) Dizziness (3) Numbness, weakness, or paralysis (usually onesided) (4) Loss of bowel or bladder control (5) Impaired vision (6) High blood pressure (7) Difficult respiration or snoring (8) Nausea or vomiting (9) Seizures (10) Unequal pupils (11) Headaches (12) Loss of vision in one eye (13) Unconsciousness (uncommon) Patient care (pp. 465–466) i. ii. For conscious patient (1) Maintain and monitor airway. (2) Administer high-concentration oxygen. (3) Calm and reassure patient. (4) Transport in a semisitting position. For unconscious patient (1) Open airway if patient can’t maintain on own. iii. E. (2) Provide high-concentration oxygen. (3) Transport with patient lying on the affected side. Follow any special protocols. Dizziness and syncope (pp. 466–469) (Fig. 19-6, p. 467) 1. Dizziness can be described in many ways by patients: loss of strength, spinning, lightheadedness, weakness 2. Syncope is a brief loss of consciousness with spontaneous recovery a. 3. May have some symptoms as a warning before an episode i. Lightheadedness ii. Dizziness iii. Nausea iv. Weakness v. Vision changes vi. Sudden pallor (loss of normal skin color) vii. Sweating viii. Occasionally incontinence ix. Patient may describe palpitations, racing heart, slow heart rate, or a headache. Causes of dizziness and syncope (pp. 467–469) a. b. Hypovolemia i. Low fluid/blood volume (dehydration) ii. Women of childbearing age may have ruptured ectopic pregnancy iii. Slow leaking abdominal aortic aneurysm iv. Gastrointestinal bleeding Metabolic i. Hypoglycemia c. d. Environmental/toxicological i. Alcohol/drugs ii. Carbon monoxide poisoning iii. Panic attacks Cardiovascular i. ii. e. 4. Dysrhythmias (1) Bradycardia (2) Tachycardia Vasovagal syncope Other causes Patient assessment (p. 469) a. Questions for focused history and physical exam i. What do you mean by dizziness? weakness? a spinning sensation? lightheadedness? ii. Did you have any warning? If so, what was it like? iii. When did it start? iv. How long did it last? v. What position were you in when the episode occurred? vi. Have you had any similar episodes in the past? If so, what cause was found? vii. Are you on medication for this kind of problem? viii. Did you have any other signs or symptoms? Nausea? Vomiting (what did it look like)? Black tarry stools? ix. Did you witness any unpleasant sight or experience a strong emotion? x. Did you hurt yourself? xi. Did anyone witness involuntary movments of the extremities (like seizures)? 5. Patient care (p. 469) a. Administer high-concentration oxygen. b. Loosen any tight clothing around the neck. c. Get the patient flat and elevate the legs if there is no reason not to do so. d. Call ALS if it is available in your area. e. Treat any associated injuries the patient may have incurred from the fall. f. Transport in the position of comfort.