Abstract
advertisement

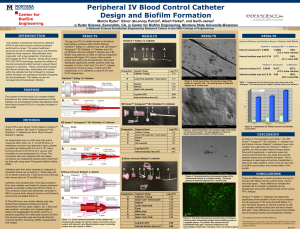
Name of Student: Joey Chor Yee Lo Research Supervisor: Dr. Dirk Lange Title of Presentation: Novel Antimicrobial Peptide Coating to Prevent Catheter-Associated Urinary Tract Infections Abstract BACKGROUND: Catheter-associated urinary tract infections are the most common source of hospital-acquired infection. Similar to most implanted devices, catheters provide ideal surfaces for bacterial adhesion and colonization, leading to the development of bacterial biofilms. These biofilms are surrounded by a thick protective polysaccharide layer, which antibiotics and other antimicrobial agents are unable to penetrate, rendering biofilms resistant to the most common agents used for the treatment of device-associated infections. Alternate approaches to prevent biofilm formation include the use of various antimicrobial surface modifications; however they have resulted in limited success due to their small spectrum of activity, poor stability and modest biocompatibility. The current study aims to take a different approach at preventing catheter-associated infections through the use of antimicrobial peptides (AMPs) linked to the catheter surface via polymer brushes as a novel antimicrobial catheter coating. These AMPs have broad-spectrum activity and, because they are innate to humans, are non-toxic and unlikely to lead to bacterial resistance. Our group has previously shown promising antimicrobial effects of AMP coatings at preventing titanium implant associated infections. The objective of the present project is to further refine this technology using a variety of in vitro and in vivo infection models to optimize the antimicrobial properties and biocompatibility of the AMPs towards their application in the urinary tract. METHODS: Brush+peptide-coated, brush-coated, and uncoated control slides were tested against various uropathogens via co-incubation followed by CFU counts of adherent bacteria. A biofilm formation model was evaluated by incubating bacteria-contaminated slides in a drip flow reactor (DFR), which mimics the in vivo environment of implanted catheters by maintaining continuous, low fluid shear conditions. Finally, an animal bladder catheterization model is being developed using 12week-old female rats to eventually evaluate bacterial adhesion to and biofilm formation on the surface of coated and uncoated catheters. In preliminary studies for the development of this model, the correct location of catheter pieces within the bladder was confirmed using urinary tract necropsy. After verifying the catheterization method, the model was further expanded via the introduction of an infectious amount of uropathogen into the catheterized rodent bladder, and the amount of adherent bacteria on the surface of the catheters was determined 2 days post-implantation. RESULTS: In vitro co-incubation experiments showed a 50% decrease in adherent bacteria by the polymer brush alone compared to uncoated controls, which was further decreased to 75% by linking AMPs to the surface. CFU counts from three independent DFR tests ranged from 6x106 CFU/mL to 1.2x107 CFU/mL, with a standard error of approximately 8x105 CFU/mL demonstrating the reproducibility of this model. Furthermore, urinary tract necropsy of bladder catheterized animals confirmed successful implantation of catheter pieces, allowing for the initiation of infection studies. CONCLUSIONS: Linking AMPs to the surface of urinary catheter materials via polymer brushes significantly reduces the number of bacteria adherent to the surface compared to uncoated control samples. Furthermore, the DFR model is a reliable system that will allow us to study the efficacy of AMPs to prevent biofilm formation using flow conditions similar to those in the urinary tract. Lastly, the successful introduction of catheter pieces into the urinary bladder of rats provides us with a convenient model to study the polymer brush/AMP combination to prevent bacterial adhesion and biofilm formation in an in vivo setting.