Hepatic arterioportal fistula – Doppler and Ultrasound
advertisement

Hepatic arterioportal fistula – Doppler and Ultrasound
findings
Author(s)
Belo-Oliveira P, Vaz O, Belo-Soares P, Martins M, Pinto E
Patient
female, 69 year(s)
Clinical Summary
A 69 years old female patient presented to our Radiology department to control a hepatic
cyst that have been drained because of its great dimensions.
Clinical History and Imaging Procedures
A 69 years old female patient presented to our Radiology department to control a hepatic
cyst that have been drained because of its great dimensions. Ultrasound confirmed the
presence of the cyst at the left hepatic lobe, with a small size. However we could see a
small hypoechoic nodule nearby. Colour Doppler ultrasound demonstrated the highly
vascular nature of the nodule. Pulsed Doppler ultrasound of the enlarged hepatic artery
demonstrated high-velocity flow and a low resistivity index, and colour speckling in the
hepatic parenchyma adjacent to the nodule. Contrast enhanced ultrasound confirmed the
highly vascular nature of the nodule establishing the diagnosis of a hepatic arterioportal
fistula.
Discussion
Arterioportal fistulas may be intra- or extrahepatic and acquired or congenital. The most
common causes of acquired arterioportal fistulas are cirrhosis and hepatic neoplasms, blunt
or penetrating trauma, percutaneous liver biopsy, transhepatic cholangiography,
gastrectomy, and biliary surgery. They can be associated with hereditary hemorrhagic
telangiectasia, Ehlers-Danlos syndrome, and biliary atresia, although in most case reports
they are not associated with any other disease. Arteriovenous fistula is a known
complication of percutaneous liver biopsy. Most are arterial—portal fistulas, which are
believed to occur more frequently than hepatic arteriovenous fistulas because of the closer
proximity in the liver of the hepatic artery to the portal vein. Doppler US is the single most
useful imaging modality for making the diagnosis. Common findings include enlargement
of the hepatic artery and dilatation of the segment of the portal vein where the fistula is
located. Doppler US features of arterioportal fistula include pulsatile hepatofugal flow in
the portal vein and colour speckling in the hepatic parenchyma adjacent to the fistula
(vibration artefact). Both contrast-enhanced CT and contrast-enhanced MR imaging may
demonstrate marked enhancement of the main portal vein, segmental branches, or major
tributaries, with attenuation or signal intensity approaching that of the aorta on arterialphase images. Perfusion anomalies of the adjacent parenchyma can also be demonstrated
(eg, regional increase in arterial inflow as a response to the inverted portal flow, increase in
portal vein inflow due to the shunt itself). If left untreated, arterialization of the portal vein
causes early onset of portal hypertension. Hepatoportal sclerosis and fibrosis of the portal
radicles subsequently develop, further contributing to portal hypertension. Congenital
hepatic arterioportal fistula in infants with biliary atresia is difficult to resolve because
these infants are abnormally dependent on arterial inflow, and ligation or embolization of
the hepatic artery could lead to fatal hepatic necrosis. Embolization of the feeding artery
with or without subsequent surgery is currently the preferred therapeutic option. It is
important to closely observe affected patients because the fistula can recur through arterial
collateralization. If the symptoms cannot be controlled with therapeutic manoeuvres, liver
transplantation is the only remaining option.
Final Diagnosis
Hepatic arterioportal fistula – Doppler and Ultrasound findings
MeSH
1. Arteriovenous Fistula [C14.907.150.125]
An abnormal communication between an artery and a vein.
References
1. [1]
Arterioportal fistula causing acute pancreatitis and hemobilia after liver biopsy.
Machicao VI, Lukens FJ, Lange SM, Scolapio JS. J Clin Gastroenterol. 2002
Apr;34(4):481-4
2. [2]
Arterioportal fistula and hemobilia with associated acute cholecystitis: a
complication of percutaneous liver biopsy. Cacho G, Abreu L, Calleja JL, Prados E,
Albillos A, Chantar C, Perez Picouto JL, Escartin P. Hepatogastroenterology. 1996
Jul-Aug;43(10):1020-3
3. [3]
Coil embolization of a solitary congenital intrahepatic hepatoportal fistula.
Raghuram L, Korah IP, Jaya V, Athyal RP, Thomas A, Thomas G. Abdom
Imaging. 2001 Mar-Apr;26(2):194-6
Citation
Belo-Oliveira P, Vaz O, Belo-Soares P, Martins M, Pinto E (2005, Nov 22).
Hepatic arterioportal fistula – Doppler and Ultrasound findings, {Online}.
URL: http://www.eurorad.org/case.php?id=3859
DOI: 10.1594/EURORAD/CASE.3859
To top
Published 22.11.2005
DOI 10.1594/EURORAD/CASE.3859
Section Liver, Biliary System, Pancreas, Spleen
Case-Type Clinical Case
Views 38
Language(s)
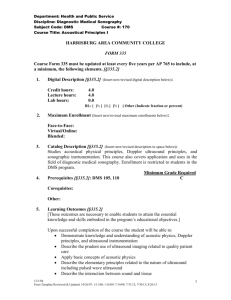
Figure 1
Abdominal ultrasound
Abdominal ultrasound showing the hepatic cyst
Figure 2
Abdominal ultrasound
Abdominal ultrasound showing the hypoechoic nodule
Figure 3
Abdominal ultrasound
Abdominal ultrasound showing the hypoechoic nodule
Figure 4
Colour Doppler ultrasound
Colour Doppler ultrasound demonstrated the highly vascular nature of the nodule.
Figure 5
Colour Doppler ultrasound
Colour Doppler ultrasound demonstrated the highly vascular nature of the nodule.
Figure 6
Pulsed Doppler ultrasound
Pulsed Doppler of the enlarged hepatic artery demonstrated high-velocity flow and a low
resistivity index
Figure 7
Pulsed Doppler ultrasound
Pulsed Doppler of the enlarged hepatic artery demonstrated high-velocity flow and a low
resistivity index
Figure 8
Contrast enhanced ultrasound
arterial phase contrast enhanced ultrasound confirmed the highly vascular nature of the
nodule
Figure 9
Contrast enhanced ultrasound
portal phase contrast enhanced ultrasound confirmed the highly vascular nature of the
nodule
Figure 10
Contrast enhanced ultrasound
late phase contrast enhanced ultrasound confirmed the vascular nature of the nodule
Figure 11
Contrast enhanced ultrasound
contrast enhanced ultrasound confirming the presence of the cyst
Figure 1
Abdominal ultrasound
Abdominal ultrasound showing the hepatic cyst
Figure 2
Abdominal ultrasound
Abdominal ultrasound showing the hypoechoic nodule
Figure 3
Abdominal ultrasound
Abdominal ultrasound showing the hypoechoic nodule
Figure 4
Colour Doppler ultrasound
Colour Doppler ultrasound demonstrated the highly vascular nature of the nodule.
Figure 5
Colour Doppler ultrasound
Colour Doppler ultrasound demonstrated the highly vascular nature of the nodule.
Figure 6
Pulsed Doppler ultrasound
Pulsed Doppler of the enlarged hepatic artery demonstrated high-velocity flow and a low
resistivity index
Figure 7
Pulsed Doppler ultrasound
Pulsed Doppler of the enlarged hepatic artery demonstrated high-velocity flow and a low
resistivity index
Figure 8
Contrast enhanced ultrasound
arterial phase contrast enhanced ultrasound confirmed the highly vascular nature of the
nodule
Figure 9
Contrast enhanced ultrasound
portal phase contrast enhanced ultrasound confirmed the highly vascular nature of the
nodule
Figure 10
Contrast enhanced ultrasound
late phase contrast enhanced ultrasound confirmed the vascular nature of the nodule
Figure 11
Contrast enhanced ultrasound
contrast enhanced ultrasound confirming the presence of the cyst
To top
Home Search History FAQ Contact Disclaimer Imprint
![Jiye Jin-2014[1].3.17](http://s2.studylib.net/store/data/005485437_1-38483f116d2f44a767f9ba4fa894c894-300x300.png)