SCP 7 SHARED CARE PROTOCOL Epoetin Clinical Indication: M
advertisement

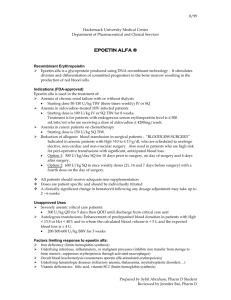
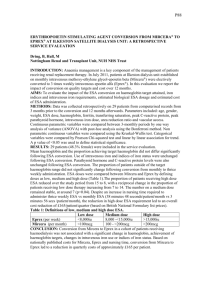
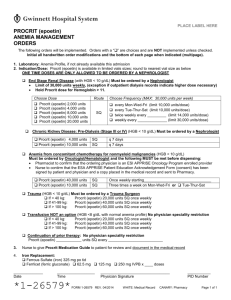
SCP 7 SHARED CARE PROTOCOL Epoetin Clinical Indication: Management of anaemia in Chronic Renal Failure Version 1: June 2014 due for review: June 2016 Introduction Erythropoietin is a hormone that is produced by the kidney; in chronic renal failure there may be lower levels of erythropoietin, which can lead to anaemia. Epoetin (recombinant human erythropoietin) is a major advance in the treatment of anaemia in chronic renal failure. It stimulates erythropoesis by increasing proliferation and maturation of erythroid progenitors. Correction of anaemia in chronic renal failure with epoetin reduces the risk of cardiovascular disease, improves patient well-being, exercise tolerance, quality of life and reduces the need for blood transfusions. Blood transfusions carry the risk of transfusion related hepatitis, which may have major implications for the management of dialysis patients. In addition, sensitisation to foreign HLA antigens may occur making the possibility of successful renal transplantation less likely. Shared Care A shared care protocol is used to facilitate the sharing of care and transfer of prescribing. This would usually take place once the patient’s condition is stable; the patient is demonstrably benefiting from the treatment and is free from any significant side effects. GPs should only take on the prescribing when they are confident in the use of the drug, in the context of the protocol. Contingency plans must be in place to enable the patient to receive the recommended treatment, should the GP decline to prescribe. Indication for Therapy This leaflet provides information on epoetin and guidelines for the shared care of home haemodialysis, peritoneal dialysis and pre-dialysis patients. Patients will be stabilised on epoetin over the first 12 weeks of treatment by the hospital and thereafter prescribing of epoetin will be continued in general practice. Before starting on epoetin therapy the patient must be medically stable, iron replete, have well controlled blood pressure and no contraindications (e.g. uncontrolled hypertension). The patient’s iron, Total Iron Binding Capacity (TIBC) and ferritin will be checked prior to initiating therapy. Most renal patients take iron supplements and additional parenteral iron may be given if necessary. The aim of therapy is to increase haemoglobin (Hb) levels by 10 to 20g/L per month to a target range of 105 to 125g/L. This stabilisation period lasts approximately 12 weeks and the patient will normally be under the care of the renal physicians at RIE / BGH who will prescribe epoetin in this period. During this time Hb and blood pressure should be checked fortnightly. Not all patients respond rapidly and a slower response may occur in some patients. Rarely a poor response is seen, in such situations a cause must be looked for. Preparations Available Eprex® (Janssen-Cilag): Epoetin alfa Pre-filled syringe: 1000, 2000, 3000, 4000, 5000, 6000, 8000, 10000, 20000, 30000, 40000 units Mircera®▼ (Roche): Epoetin beta (Methoxy polyethylene glycol-epoetin beta) Pre-filled syringe: 30, 50, 75, 100, 120, 150, 200, 250, 360 micrograms Supplied directly from manufacturer to community pharmacy, usually within 48 hours of receiving telephone order -1Created by amcvean 13/02/2016 Recommended Dosage and Administration Epoetin can be administered intravenously or subcutaneously. Dosage - Initial dose Haemodialysis: (Eprex®) 50 units/kg three times a week (IV). Patients will receive a maintenance dose according to their haemoglobin levels. Peritoneal or pre-dialysis: (Mircera®▼) 0.6 micrograms/kg once every two weeks (SC), until Hb >100g/L is reached. Maintenance dose of Mircera®▼ can then be given monthly at double the previous fortnightly dose. Cost The cost of epoetin treatment is approximately £200 per month per patient for Eprex® at a dose of 3000 units three times a week and £177 for Mircera®▼ at a dose of 120micrograms once monthly. Shared Care Responsibilities Aspects of Care for which the Consultant is responsible Assessing suitability of patients with epoetin Prescribing epoetin during the 12 week initiation and stabilisation phase Adjusting dosage of epoetin Monitoring Hb, urea and electrolytes and BP at clinic visits Monitoring and adjusting dry weight, dialysis therapy, diet and phosphate binding agents and antihypertensive drugs Monitoring iron status and giving appropriate therapy Aspects of Care for which the General Practitioner is responsible Monitoring Hb, urea and electrolytes and BP between clinic visits by arrangement with hospital staff Contacting the anaemia co-ordinator or the consultant in charge if concerned about the results Adjusting antihypertensives to control BP in conjunction with hospital staff Prescribing epoetin after the 12 week stabilisation period Reporting of adverse reactions to Yellow Card Scotland is the responsibility of both the Consultant and GP https://yellowcard.mhra.gov.uk/ Adverse Effects The following have been reported: Diarrhoea, nausea, vomiting, dose dependent increase in blood pressure or aggravation of hypertension, headache, seizures, rash, arthralgia, influenza-like symptoms, fistula thrombosis. Hot flushes have also been reported with Mircera®▼. For a full list of adverse effects please refer to the Summary of Product Characteristics. Management Suspend treatment if blood pressure is too high (above 170/95mmHg) or patient has persistent severe headache. Mircera®▼ is a black triangle ▼ medicine - report all suspected adverse effects via Yellow Card Centre Scotland. Drug Interactions As ciclosporin is bound by red blood cells there is potential for a drug interaction. If epoetin is given concomitantly with ciclosporin, blood levels of ciclosporin should be monitored and the dose of ciclosporin adjusted as the haematocrit rises. Contra-Indications Uncontrolled hypertension, hypersensitivity to the active substance or to any of the excipients. Caution in patients with active malignancy. Pure red cell aplasia has been reported with epoetin - treatment must be discontinued if this occurs -2Created by amcvean 13/02/2016 Pregnancy and Lactation Eprex® There are no adequate and well-controlled studies in pregnant women. Studies in animals have shown reproduction toxicology therefore in chronic renal failure patients, Eprex® should be used in pregnancy only if the potential benefit outweighs the potential risk to the foetus. Mircera®▼ There is no data from the use of Mircera® in pregnant women. Animal studies do not indicate direct harmful effects with respect to pregnancy, embryo-foetal development, parturition or postnatal development but indicate a class-related reversible reduction in foetal weight. Caution should be exercised when prescribing to pregnant women. It is unknown whether Eprex® or Mircera® is excreted in human breast milk. One animal study has shown excretion of Mircera® in maternal milk. A decision on whether to continue or discontinue breastfeeding or to continue or discontinue therapy with Eprex® or Mircera® should be made taking into account the benefit of breast-feeding to the child and the benefit of therapy to the woman. Monitoring After stabilisation regular review is needed to keep the patient’s haemoglobin at the target concentration as several factors can reduce response to epoetin, e.g. deficiencies of iron, folic acid or vitamin B12 which will require to be corrected. Response may also be reduced in sepsis, blood loss, chronic inflammation and malignancy. Dose adjustment may be required and many patients can be maintained on lower doses than during the initiation phase. When the patient is stable, haemoglobin and blood pressure should be checked monthly and iron status three-monthly. Contact Points Contact Points Anaemia co-ordinator can be contacted via RIE switchboard on 0131 536 1000 (bleep 5487) or 0131 242 1204 between 9.00am – 5.00pm Monday to Friday. Other numbers 0131 242 1217 renal registrar, renal ward 0131 242 2061 The renal pharmacists may be contacted via RIE switchboard on 0131 536 1000 (bleep 8006 or 2294) between 8.30am – 5.00pm Monday to Friday. The Edinburgh Renal team may also be contacted for advice regarding their patients via the renal email advice line at rie.renaladvice@luht.scot.nhs.uk This information was prepared by the consultants and pharmacists of the Renal Unit, Royal Infirmary of Edinburgh, through liaison with the General Practice Prescribing Committee and Drug and Therapeutics Committee, Lothian University Hospitals Division . Used and adapted with permission. -3Created by amcvean 13/02/2016