Hackensack University Medical Center
advertisement

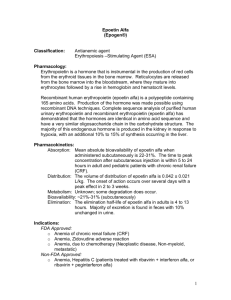
8/99 Hackensack University Medical Center Department of Pharmaceutical and Clinical Services EPOETIN ALFA ® Recombinant Erythropoietin Epoetin alfa is a glycoprotein produced using DNA recombinant technology . It stimulates division and differentiation of committed progenitors in the bone marrow resulting in the production of red blood cells. Indications (FDA-approved) Epoetin alfa is used in the treatment of: Anemia of chronic renal failure with or without dialysis Starting dose 50-150 U/kg TIW (three times weekly) IV or SQ Anemia in zidovudine-treated HIV-infected patients Starting dose is 100 U/kg IV or SQ TIW for 8 weeks. Treatment is for patients with endogenous serum erythropoeitin level is ≤ 500 mUnits/ml who are receiving a dose of zidovudine ≤ 4200mg/week. Anemia in cancer patients on chemotherapy Starting dose is 150 U/kg SQ TIW. Reduction of allogenic blood transfusion in surgical patients : “BLOODLESS SURGERY” Indicated in anemic patients with Hgb >10 to ≤ 13 g/dl, who are scheduled to undergo elective, non-cardiac and non-vascular surgery. Also used in patients who are high risk for peri-operative transfusions with significant, anticipated blood loss. Option 1: 300 U/kg/day SQ for 10 days prior to surgery, on day of surgery and 4 days after surgery. Option 2: 600 U/kg SQ in once weekly doses (21, 14 and 7 days before surgery) with a fourth dose on the day of surgery. All patients should receive adequate iron supplementation Doses are patient specific and should be individually titrated A clinically significant change in hematocrit following any dosage adjustment may take up to 2 – 6 weeks Unapproved Uses Severely anemic critical care patients: 300 U/kg QD for 5 days then QOD until discharge from critical care unit Autologous transfusions: Enhancement of predeposited blood donation in patients with Hgb < 13.5 or Hct < 40% and in whom the calculated blood volume is < 5 L and the expected blood loss is 4 U. 200-300-600 U/kg BIW for 3 weeks Factors limiting response to epoetin alfa: Iron deficiency (limits hemoglobin synthesis) Underlying infectious, inflammatory, or malignant processes (inhibits iron transfer from storage to bone marrow, suppresses erythropoiesis through activated macrophages) Occult blood loss/hemolysis (counteracts epoetin alfa-stimulated erythropoiesis) Underlying hematologic diseases (refractory anemia, thalassemia, myelodysplastic disorders…) Vitamin deficiencies: folic acid, vitamin B12 (limits hemoglobin synthesis) Prepared by Sybil Abraham, Pharm D Student Reviewed by Jennifer Bui, Pharm D 8/99 Aluminum toxicity (inhibits iron incorporation into heme protein) Contraindications Uncontrolled hypertension Known hypersensitivity to mammalian cell-derived products Know hypersensitivity to Albumin (human) Complications Hypertension>10% Fatigue, headache, fever >10% Arthralgias 1-10% Edema, chest pain 1-10% Thrombotic Events ( MI, TIA, CVA) < 1% Monitoring Patient’s iron stores (serum ferritin, transferrin saturation) should be evaluated prior to starting therapy. Transferrin saturation should be at least 20% and ferritin at least 100 ng/ml. Blood pressure should be adequately controlled prior and during therapy, with close monitoring. Hct should be monitored twice a week at start of therapy and after any dosage change, until stable and then should be checked at regular intervals. A rise in Hct should be seen in 2-6 weeks. Reticulocyte count begins to rise before Hct and is a good measure of efficacy. An increase should be seen within 7-10 days (up to 10%). Hgb and CBC with differential should also be closely monitored. Co-Medications Needed Iron: If serum ferritin is low (mild-moderate) but > 100 ng/ml, transferrin saturation 20-30%: Ferrous sulfate PO 325 mg TID during therapy If ferritin is low (severe) and < 100 ng/ml or transferrin saturation is <20%: Iron dextran IV (total IV dose is calculated based on patient’s weight, hemoglobin, amount of blood loss if known) Vitamin B12 Folic acid References 1. Cazzola M, Mercuriali F, Brunara C. Use of Recombinant Human Erythropoietin Outside the Setting of Uremia. Blood 1997;89(2):4248-4267 2. Corwin H, Gettinger A, Rodriguez R, et al. Efficacy of Recombinant Human Erythropoietin in the Critically Ill Patient: A Randomized Double Blind Placebo Controlled Trial. Critical Care Medicine 1998;26 (1):A23 3. EPOGEN®(Epoetin alfa) for injection. Package Insert. California:Amgen Inc.: Dec 1996. 4. Faris PM, Ritter MA. Epoetin Alfa, A Bloodless Approach for the Treatment of Perioperative Anemia. Clinical Orthopaedics and Related Research 1998;357:60-67 5. Goodnough LT, Monk TG. Erythropoietin Therapy in the Perioperative Setting. Clinical Orthopaedics and Related Research 1998;357:82-88 6. McCarthy JT. A Practical Approach to the Management of Patients with Chronic Renal Failure. Mayo Clinical Proceedings 1999;74:269-273 7. Spivak JL. The Biology and Clinical Applications of Recombinant Erythropoietin. Seminars in Oncology 1998;3(7):7-11 Prepared by Sybil Abraham, Pharm D Student Reviewed by Jennifer Bui, Pharm D 8/99 Prepared by Sybil Abraham, Pharm D Student Reviewed by Jennifer Bui, Pharm D