Erythropoietin stimulating agent conversion from Mircera ® to Eprex
advertisement
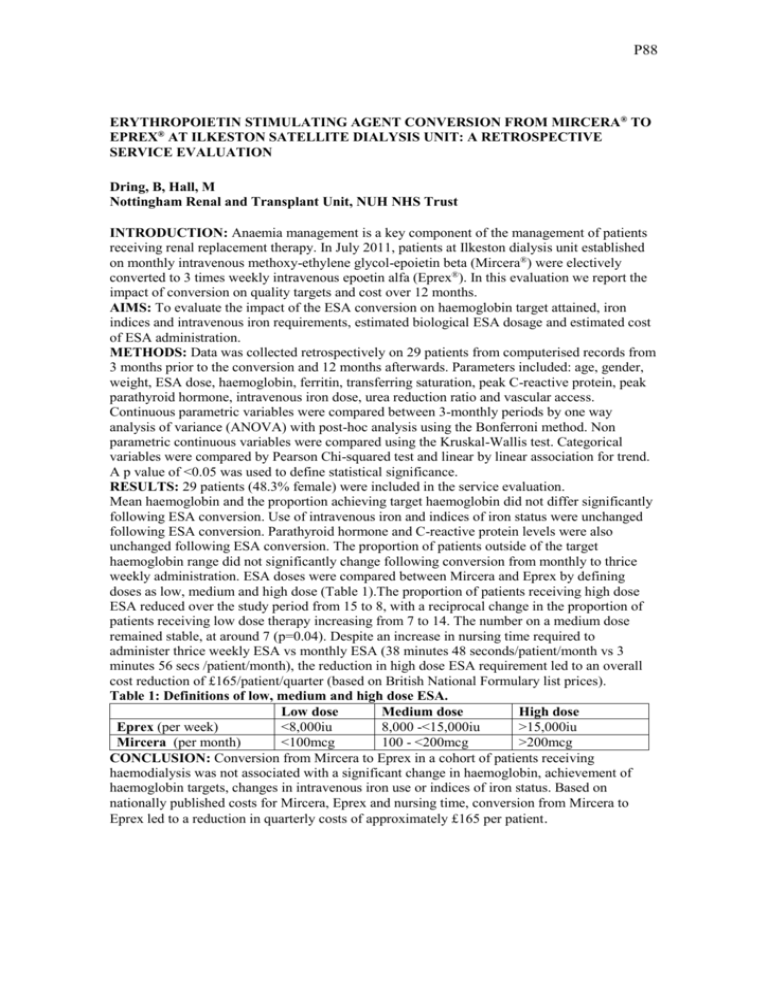
P88 ERYTHROPOIETIN STIMULATING AGENT CONVERSION FROM MIRCERA® TO EPREX® AT ILKESTON SATELLITE DIALYSIS UNIT: A RETROSPECTIVE SERVICE EVALUATION Dring, B, Hall, M Nottingham Renal and Transplant Unit, NUH NHS Trust INTRODUCTION: Anaemia management is a key component of the management of patients receiving renal replacement therapy. In July 2011, patients at Ilkeston dialysis unit established on monthly intravenous methoxy-ethylene glycol-epoietin beta (Mircera®) were electively converted to 3 times weekly intravenous epoetin alfa (Eprex®). In this evaluation we report the impact of conversion on quality targets and cost over 12 months. AIMS: To evaluate the impact of the ESA conversion on haemoglobin target attained, iron indices and intravenous iron requirements, estimated biological ESA dosage and estimated cost of ESA administration. METHODS: Data was collected retrospectively on 29 patients from computerised records from 3 months prior to the conversion and 12 months afterwards. Parameters included: age, gender, weight, ESA dose, haemoglobin, ferritin, transferring saturation, peak C-reactive protein, peak parathyroid hormone, intravenous iron dose, urea reduction ratio and vascular access. Continuous parametric variables were compared between 3-monthly periods by one way analysis of variance (ANOVA) with post-hoc analysis using the Bonferroni method. Non parametric continuous variables were compared using the Kruskal-Wallis test. Categorical variables were compared by Pearson Chi-squared test and linear by linear association for trend. A p value of <0.05 was used to define statistical significance. RESULTS: 29 patients (48.3% female) were included in the service evaluation. Mean haemoglobin and the proportion achieving target haemoglobin did not differ significantly following ESA conversion. Use of intravenous iron and indices of iron status were unchanged following ESA conversion. Parathyroid hormone and C-reactive protein levels were also unchanged following ESA conversion. The proportion of patients outside of the target haemoglobin range did not significantly change following conversion from monthly to thrice weekly administration. ESA doses were compared between Mircera and Eprex by defining doses as low, medium and high dose (Table 1).The proportion of patients receiving high dose ESA reduced over the study period from 15 to 8, with a reciprocal change in the proportion of patients receiving low dose therapy increasing from 7 to 14. The number on a medium dose remained stable, at around 7 (p=0.04). Despite an increase in nursing time required to administer thrice weekly ESA vs monthly ESA (38 minutes 48 seconds/patient/month vs 3 minutes 56 secs /patient/month), the reduction in high dose ESA requirement led to an overall cost reduction of £165/patient/quarter (based on British National Formulary list prices). Table 1: Definitions of low, medium and high dose ESA. Low dose Medium dose High dose Eprex (per week) <8,000iu 8,000 -<15,000iu >15,000iu Mircera (per month) <100mcg 100 - <200mcg >200mcg CONCLUSION: Conversion from Mircera to Eprex in a cohort of patients receiving haemodialysis was not associated with a significant change in haemoglobin, achievement of haemoglobin targets, changes in intravenous iron use or indices of iron status. Based on nationally published costs for Mircera, Eprex and nursing time, conversion from Mircera to Eprex led to a reduction in quarterly costs of approximately £165 per patient.