Azathioprine tablets for inflammatory arthritis, connective tissue
advertisement

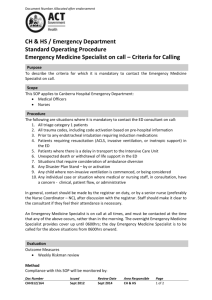
Shared Care Guideline Azathioprine tablets For the treatment of: Inflammatory arthritis, connective tissue disease and vasculitis in adults ( 16 years old) For the latest information on interactions and adverse affects, always consult the latest version of the Summary of Product Characteristics (SmPC), which can be found at: www.medicines.org.uk These guidelines are based on the monitoring criteria of the British Society of Rheumatology, published in the following reference: Chakravarty, K., McDonald, H., Pullar, T. et al. (2008) BSR/BHPR guideline for diseasemodifying anti-rheumatic drug (DMARD) therapy in consultation with the British Association of Dermatologists. Rheumatology 47(6), 924-925. Authors: Dr Kelsey M Jordan (Consultant Rheumatologist, BSUH NHS Trust) Dr Stewart E Glaspole (Pharmacist, BSUH NHS Trust/BHCPCT) AZASCG Document status Final/Draft: Final 13 Jan 2009 Date of next review if final: 13 Jan 2010 Page 1 of 9 Drug Name Azathioprine 25mg and 50mg tablets. Indications for use within the protocol Inflammatory arthritis, connective tissue disease and vasculitis diagnosed by a Rheumatologist, usually supported by indices of inflammation. Duration – most drugs require up to 3 to 4 months trial to assess efficacy (including the time required for dose stabilisation). Therapy is continued providing the drug is working and that any side effects are tolerated by the patient. Relapse is common after withdrawal of therapy. Background Azathioprine is used as a disease modifying agent to induce and maintain remission in several types of rheumatic disease. It can reduce inflammation and affect the immune system and is therefore used for a number of Rheumatological conditions. Pharmacology Azathioprine is an antimetabolite agent which has been shown to exert antirheumatic and immunosuppressive activity making it an effective drug in many rheumatological conditions. There are many suggested mechanisms of action with no single apparent pathway. Dosage and administration Prior to starting azathioprine, best practice recommends checking the TPMT (thiopurine s-methyltransferase) activity; this enzyme is involved in the metabolism of azathioprine and its activity is controlled by a genetic polymorphism. TPMT testing, initial dosing and subsequent dose adjustments will be the responsibility of the specialist team. The usual dose of azathioprine is between 1-3mg/kg/day. The maximum dose differs between individuals. Contraindications to use Azathioprine is contra-indicated in: Immunization with live vaccines (see additional cautions) Pregnancy and breast feeding except in clinically indicated cases (see section on pregnancy and lactation) TPMT deficiency (homozygous state): Avoid, can be fatal Individuals with Lesch-Nyhan Syndrome due to congenital hypoxanthine-guanine phosphoribosyl transferase (HGPRT) deficiency. Patients taking allopurinol (see interactions) AZASCG Document status Final/Draft: Final 13 Jan 2009 Date of next review if final: 13 Jan 2010 Page 2 of 9 Additional cautions All patients contemplating becoming pregnant must be seen by a consultant Rheumatologist at the earliest opportunity to discuss the complex issues surrounding therapy with azathioprine Patients receiving azathioprine must not receive immunization with live vaccines. Inactivated polio is available although suboptimal response may be seen Annual flu and pneumovax vaccination are recommended In patients receiving azathioprine exposed to chickenpox or shingles, passive immunization should be carried out using varicella zoster immunoglobulin (VZIG). Please contact the specialist team for more information. Monitoring The British Society for Rheumatology (BSR) recommends precise monitoring to be carried out for this drug. The requirements are summarised in the following table. a. Pre-treatment assessment b. Ongoing Monitoring c. Following FBC, U&E, creatinine, LFTs, TPMT assay. These tests will be carried out by the initiating hospital specialist. FBC and LFTs weekly for 6 weeks and continue every 2 weeks until dose stable for 6 weeks; then monthly If maintenance dose is achieved and stable for 6 months consider discussing with patient to reduce monitoring to 3 monthly. Repeat FBC and LFTs 2 weeks after dose change and then monthly. U&E and creatinine should be repeated 6 monthly (unless more frequent testing is clinically indicated). ESR and/or CRP every three months (not required but useful) changes in dose Additional monitoring Actions to be taken 9 WBC<3.5x10 /l Withhold until discussed with specialist team 9 Neutrophils<2.0x10 /l Withhold until discussed with specialist team Platelets<150x109/l Withhold until discussed with specialist team AST, ALT>twice upper limit of normal Withhold until discussed with specialist team Rash or oral ulceration Withhold until discussed with specialist team MCV>105 fl Check serum folate and B12 & TSH. Treat any underlying abnormality. If results normal discuss with specialist team. Abnormal bruising or severe sore throat Withhold until FBC results available and discuss with the specialist team. AZASCG Document status Final/Draft: Final 13 Jan 2009 Date of next review if final: 13 Jan 2010 Page 3 of 9 Undesirable effects The most common side effects (affecting approximately 20% of patients) are flu-like symptoms (myalgia, headache, diarrhoea) which characteristically occur 2-3 weeks after initiating treatment and usually subside if treatment is continued. The most important complication is bone marrow suppression causing leucopenia or thrombocytopenia (both more likely to develop in those with a low TPMT activity) and is most likely to occur in the first few weeks of treatment. It is important that patients are informed that they should consult either their GP or specialist team1 should they develop symptoms of possible myelosuppression such as sore throat (or other signs of infection) or easy bruising. In the case of such presentation an urgent FBC should be carried out. A FBC must also be performed on any patient on azathioprine who becomes unwell as profound myelosuppression can develop between routine blood tests. If a patient is found to be myelosuppressed, azathioprine therapy should be stopped immediately and medical advice should be sought1 Should a FBC suggest myelosuppression (total white cell count <3.5x109 /l or platelet count < 100x109/l) or LFTs become deranged (progressive rise in AST/ALT) urgent advice from an appropriate consultant should be sought using the contact details provided. Relative neutropenia (<2.0 x109/l) requires close monitoring. Please note that lymphopenia should be expected (lymphocyte count <1.0 x109/l suggests compliance with treatment). Pregnancy and Lactation Women of childbearing potential should be advised to use effective contraceptive precautions. Evidence of mutagenicity is equivocal in men. In most cases, azathioprine should not be prescribed if there is a possibility of pregnancy, although there may be some circumstances where the benefit of continuing treatment outweighs the possible risks related to the unborn child. A careful assessment of risk vs benefit is advised. Women treated with azathioprine should not breast feed 1 See section on contacting the specialist team AZASCG Document status Final/Draft: Final 13 Jan 2009 Date of next review if final: 13 Jan 2010 Page 4 of 9 Interactions Allopurinol: Do not use. Discuss alternatives with a Rheumatologist if urate lowering drugs are required Warfarin: Azathioprine inhibits the anticoagulant effects of warfarin. Monitor INR and alter the dose of warfarin accordingly Phenytoin, sodium valproate, absorption of these drugs Angiotensin-converting enzyme (ACE) inhibitors: Co-prescription of azathioprine may cause anaemia (if significant, consider alternative to ACE inhibitor or different DMARD) Aminosalicylates i.e. mesalazine, olsalazine, balsalazide or sulfasalazine, may contribute to bone marrow toxicity Co-trimoxazole and trimethoprim can cause life threatening haematoxicity and should not be used in patients taking azathioprine carbamazepine: Azathioprine reduces the Consultant / hospital responsibilities It is the specialist team’s responsibility to: Identify those patients who will benefit from treatment with azathioprine Undertake pre-treatment monitoring as detailed above Perform the TPMT activity tests and select initiation doses Inform the GP of the reasons for initiating azathioprine Initiate and prescribe the medication. Decide on the dose and duration of therapy and subsequent dosage adjustments Ensure that patients understand the nature and possible complications of azathioprine and their role in reporting adverse effects promptly Agree to discuss promptly with the GP questions regarding treatment with azathioprine and review patients promptly if requested by the GP Provide the patient with monitoring blood forms whilst on treatment with copies of results sent to the GP (unless the GP chooses to take responsibility for both prescribing and monitoring) Undertake responsibility to act on pathology lab results (unless the GP chooses to take responsibility) Review efficacy of treatment at regular intervals and ensure any drug treatment changes are communicated to the GP Communicate any changes in frequency of pathology testing to the GP Provide access to back up and support facilities Report any adverse events to the CSM Evaluate any adverse events reported by the GP. AZASCG Document status Final/Draft: Final 13 Jan 2009 Date of next review if final: 13 Jan 2010 Page 5 of 9 GP responsibilities It is the GP’s responsibility to: Return the shared care agreement letter to the consultant to indicate agreement with this guideline. If for any reason the GP is unhappy with the arrangements they should contact the appropriate hospital specialist Prescribe azathioprine at the dose recommended by the hospital specialist. Any decision to alter or discontinue treatment should be taken after discussion with the hospital specialist Check for possible drug interactions when newly prescribing or stopping concurrent medication (see interaction section) Report any suspected or actual adverse drug reactions to the hospital specialist and the CSM Undertake an urgent full blood count to check for leucopenia in patients developing significant infection, or multiple mouth ulcers Patient responsibilities It is the patient’s responsibility to: Report side effects to any member of the health care team Patients are expected to attend for blood tests when required, to ensure safe and effective ongoing treatment. Information to the patient The outpatient clinic will provide the patient with information about their treatment. Information about the patient to be received by the GP from the consultant Please refer to the shared care request letter attached. Two copies of this letter will be sent to the GP for each patient initiated on therapy. Patient information to be received by the consultant from the GP In order for GPs to agree formally to this shared care protocol, it is requested that both the shared care request letters attached be signed and one returned to the hospital specialist requesting shared care. Contacting the specialist team If the patient’s Consultant is not available, one of the other Consultants or Specialist Registrars will be able to help. Please call the Rheumatology department at RSCH on 01273 696955 x4631/3553 or PRH on 01444 441881 x 5432/5984 Out of hours Urgent problems should be referred to the medical team on call, contacted via RSCH switchboard on 01273 696955 or the PRH switchboard on 01444 441881 AZASCG Document status Final/Draft: Final 13 Jan 2009 Date of next review if final: 13 Jan 2010 Page 6 of 9 References 1 Paice EW. Giant cell arteritis: difficult decisions in diagnosis, investigation and treatment. Postgrad Med J 1989;65:743–7. 2 Konstantopoulou M, Belgi A, Griffiths KD, Seale JR, Macfarlane AW. Azathioprine induced pancytopenia in a patient with pompholyx and deficiency of erythrocyte thiopurine methyltransferase. Br Med J 2005;330:350–1. 3 Imuran Summary of product characteristics 25 & 50mg: 23 July and 5 August, Glaxo Smith Kline. http://emc.medicines.org.uk 4 British National Formulary 54. Pharmaceutical Press, 2007. 5 Cronstein BN. Pharmacogenetics in the rheumatic diseases. Ann Rheum Dis 2004;63(Supp. 2):ii25–7. 6 Rivier G, Khamashta MA, Hughes GR. Warfarin and azathioprine: a drug interaction does exist. Am J Med 1993;95:342. 7 Jenner E. Immunisation against infectious disease. Bicentenary Edition 1996. Her Majesty’s Stationary Office, Department of Health, London UK. www.dh.gov.uk/ 8 Ramsey-Goldman R. Treatment of inflammatory rheumatic disorders in pregnancy: what are the safest treatment options? Drug Saf 1998;19:389–410. 9 Ostensen M. Disease Specific problems related to drug therapy in pregnancy. Lupus 2004;13:746–50. 10 Clunie GPR, Lennard L. Relevance of thiopurine methyltransferase status in rheumatology patients receiving azathioprine. Rheumatology 2004;43:13–8. 11 Tavadia SMB, Mydlarski PR, Reis MD et al. Screening for azathioprine toxicity: a pharmacoeconomic analysis based on a target case. J Am Acad Dermatol 2000;42:628–32. AZASCG Document status Final/Draft: Final 13 Jan 2009 Date of next review if final: 13 Jan 2010 Page 7 of 9 Confidential shared care request Consultant name Consultant address Date GP Name GP Address Azathioprine in inflammatory arthritis, connective tissue disease and vasculitis in adults ( 16 years old) Patient Name: Patient Hospital number: Patient Address: Patient NHS Number: Dear Dr. Your patient has been commenced on: Azathioprine, at a dose of: It would be appropriate for this patient’s therapy to be shared between primary and secondary care. The enclosed Shared Care Guideline provides additional information to support you in this. Please sign both copies of this letter to indicate your agreement and return one copy to my office; the other should be placed in the patient’s notes at your practice. Yours sincerely, Consultant name GP signature Print name AZASCG Document status Final/Draft: Final 13 Jan 2009 Date of next review if final: 13 Jan 2010 Page 8 of 9 Date Confidential shared care request Consultant name Consultant address Date GP Name GP Address Azathioprine in inflammatory arthritis, connective tissue disease and vasculitis in adults ( 16 years old) Patient Name: Patient Hospital number: Patient Address: Patient NHS Number: Dear Dr. Your patient has been commenced on: Azathioprine, at a dose of: It would be appropriate for this patient’s therapy to be shared between primary and secondary care. The enclosed Shared Care Guideline provides additional information to support you in this. Please sign both copies of this letter to indicate your agreement and return one copy to my office; the other should be placed in the patient’s notes at your practice. Yours sincerely, Consultant name GP signature Print name AZASCG Document status Final/Draft: Final 13 Jan 2009 Date of next review if final: 13 Jan 2010 Page 9 of 9 Date