PAEDIATRIC GASTROENTEROLOGY SERVICE
advertisement

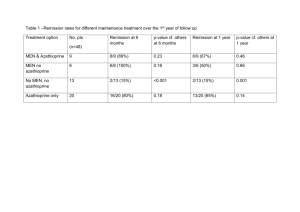
PAEDIATRIC GASTROENTEROLOGY SERVICE QUEEN’S MEDICAL CENTRE NHS TRUST SHARED-CARE PROTOCOL FOR AZATHIOPRINE Partnership Plan for Patient/Family/GP/Shared-Care Paediatrician/ Paediatric Gastroenterology Team Date: May 2006 Revision Date: May 2008 Objectives: To set out for you, your family and all concerned the important things about Azathioprine treatment. To explain how we will check the treatment is working and deal with the problems. To list side-effects you, your family and GP should look out for and when to refer back to us. How Azathioprine works? Azathioprine helps stop the white blood cells causing inflammation in the intestine, in Crohn’s disease and ulcerative colitis and in the liver in autoimmune hepatitis. How long does it take to work? Azathioprine takes about 3 months for its full effect. Problems can happen with Azathioprine and how do we deal with them We check your TPMT activity level which is an enzyme that breaks down the azathioprine and which will help indicate whether you are at increased risk of side effects and therefore need to increase the azathioprine more gradually or that you may only tolerate low doses. We list the key problems below. However, if anything else happens please discuss with your GP or the Paediatric Team. 1. Feeling sickly, being sick, or worsening diarrhoea: These may occur on starting Azathioprine. If they last longer than a couple of days contact us or your GP and we will reduce the starting dose of Azathioprine and build up more slowly. Some of the nausea may be reduced by taking with or after food. -1– 2. Feeling severely sickly, being sick a lot, or severe abdominal pain: If these occur you need to contact us and we will arrange to see you to rule out rare side-effects, such as inflammation of the pancreas gland. 3. Lowering the neutrophil white cells in your blood count: Azathioprine helps stop the white cells causing inflammation. However, it can lower the neutrophil white cells, which may cause you to have increased or difficult infections. If you have any problems with signs of a fever or an infection contact your GP or Paediatrician. We test your neutrophil white cell count regularly in the blood test to check that it is not dropping low and take action if required. 4. Abnormalities in the liver function tests: These tell us how your liver is working and we check those with the blood tests and will contact you if there are any problems or change of treatment needed. 5. Hair thinning: Hair loss can occur at the start of treatment and also as a result of the illness. This will settle and the hair will grow back. 6. Allergic rash/fever/mouth ulcers: These can occur as an allergic reaction anytime after starting Azathioprine. It is rare. If a rash occurs over your body and is itchy and unexplained, you should go to see your GP or Paediatrician. 7. Contraception and pregnancy: We will advise you should not become pregnant on Azathioprine without discussion as to the safety in pregnancy. It is important that you take adequate precautions with contraception. Please discuss this with us further if appropriate. 8. Chickenpox or contact with chickenpox: We advise that we should check your blood for immunity and chickenpox before we start the Azathioprine treatment. If you have past immunity to chickenpox in your blood you should have no problems if you are in contact with chickenpox or shingles. However, if you do come out in a chickenpox rash contact us immediately to start a course of a special treatment called aciclovir. If you have no immunity against chickenpox and have contact with chickenpox or shingles please contact us so that we can arrange for you to have a special treatment with zoster immune globulin, which helps prevent serious problems of severe chickenpox. -2– 9. Immunisations: While you are on Azathioprine (and/or prednisolone) you cannot have certain live vaccines, e.g. live poliovirus, BCG for tuberculosis, MMR. However, we do advise that you consider having a flu vaccine in the winter. So if you are offered immunisation/vaccinations while you are on Azathioprine please discuss it with your doctor or ourselves. 10. Sun Exposure: It is important when on immunosuppression to avoid excessive exposure to the sun and to wear a good effective sunscreen cream/ lotion. 11. Drug Interactions: Azathioprine can interact with other medications which may cause adverse effects. Always check that your Doctor or Pharmacist is aware that you are taking azathioprine before any new medication is started. Checking blood tests on Azathioprine: We advise the following monitoring programme: The first 8 weeks – weekly full blood count, U&E’s, LFT’s with 2-weekly inflammatory markers, ESR, CRP and A1 acid glycoprotein. The second 8 weeks – 2-weekly full blood count, U&E’s, LFT’s, with 4-weekly inflammatory markers. The next 9 weeks – 3-weekly full blood count, U&E’s, LFT’s, with 6-weekly inflammatory markers. Then monthly full blood count, U&E’s, LFTs with 2 monthly inflammatory markers but could be more frequent if unwell. The first year of monitoring and after that monthly blood count, U&E’s, LFT’s, with 2-monthly inflammatory markers. After first year if stable to be assessed by Dr Charlton to move to 2 monthly full blood count, U&E’s LFT’s and 4-monthly inflammatory markers. Actions from blood tests: 1. Neutrophil count: -3– If falls below 1 x 10 9/L to stop Azathioprine, monitor full blood count, U&E’s, LFT’s weekly until blood count rises above 1 and restart Azathioprine at a lower dose as recommended by the Paediatric Gastroenterology Team. If it falls below 2 x 10 9/L and there are significant infections we also would consider stopping until count rose above 2 x 10 9/L. 2. Platelet count: If platelet count falls progressively and is below 120 x 10 9/L, this may be a sign of Azathioprine toxicity or disease activity and the patient should be reviewed by the team. A platelet count of higher than 400 is common in active disease and should fall with treatment. Patients should be asked to report any unexpected bruising or bleeding. 3. Raised liver enzymes (Alanine Transaminase/ALT): Elevated Alanine Transaminase/ALT of greater than 2 x normal on two occasions the patient should be reviewed by the Paediatric Gastroenterology Team to consider whether further action is required. Availability: Azathioprine comes as: Azamune 50mg tablets Imuran 25mg and 50mg tablets in blister packs Dosage: Dose and administration: Patients will be started on a low dose for 5 days and then build up to their planned maintenance dose. The usual maintenance is between 1.5 and 3mg per kg per day, which can be taken at one time or divided into two doses per day. If you miss your dose you can take it later the same day but you don’t take double the dose the next day. Take with or after food. Setting up treatment with your GP: A letter suggesting shared-care with your GP will be sent as soon as the decision is made to start Azathioprine. The letter will include details of your individual treatment plan and a copy will be sent to you and your parents as well as the other doctors. The patient will receive this either from the Azathioprine Partnership Plan and an information sheet, which will come with the medicines. We will give 4 week’s supply of Azathioprine. Your GP will be asked to take on shared-care and prescribe Azathioprine under this protocol. -4– Responsibilities: Paediatric Gastroenterology Team. Explain need for Azathioprine and side-effects/problems. Arrange blood tests before starting treatment: full blood count liver function tests chickenpox immunity test (anti zoster titres) TPMT level Negotiate with the patient their follow-up blood tests (when and where). Arrange with the GP and other hospital bloods to be taken and results to be sent to Paediatric Gastroenterology for review and plotting of flow sheets by Specialist Paediatric Nurses. Results will be reviewed by the nurses/doctors and the Nurse Specialist will plot the result and bring any changes/abnormalities to the doctor’s attention. The team will contact patient’s GP and other Paediatricians involved with advice on changes in the treatment plan. Regular follow-up in Paediatric Gastroenterology Clinic with shared hospital care plan, where appropriate. The team will discuss contraception and pregnancy with the patient (see advice above). Patient responsibilities: To agree and then follow-up plan of treatment with regular blood testing and follow-up. To contact us if any concerns or difficulty in following the treatment. To inform us or your GP if you are sexually active so we can discuss risks of Azathioprine in pregnancy and need for contraception. GP responsibilities: -5– To monitor the patient’s general health and contact us if any concerns. To help us with regular blood testing and sending on results. To prescribe Azathioprine on the agreed treatment plan. Available support and advice: Contact the Paediatric Nurse Specialist Gastroenterology 0115 9249924 ext: 65806 Sister Lucy Davies Bleep 80-6568 through switchboard Mon/Wed/Thursday Sister Annette Kitchin Bleep 80-6571 through switchboard Monday – Friday Dr Mary Weston Bleep 80-8883 Paediatric Registrar on call via switchboard Sharon – Dr Charlton’s Secretary 0115 9249924 ext: 62439 Out of hours Paediatric Registrar on-call through switchboard This guideline has been registered with the QMC Hospital Trust. However, clinical guidelines are guidelines only. The interpretation and application of clinical guidelines will remain the responsibility of the individual clinician. If in doubt please contact a senior colleague or expert. Caution is advised when using guidelines after the review date. Updated by: Dr C P J Charlton – Consultant Paediatric Gastroenterologist Dr M Weston – Staff Grade in Paediatric Gastroenterology Sister L A Davies – Paediatric Gastroenterology Nurse Specialist Sister A M Kitchin – Paediatric Gastroenterology Nurse Specialist Sachin Gohil – Paediatric Pharmacy May 2006-05-12 -6–