azathioprine maintenance therapy in pauci
advertisement

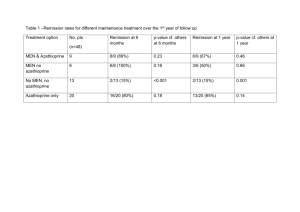
P267 AZATHIOPRINE: DOSING AND COMPLICATIONS IN PAUCI-IMMUNE RENAL VASCULITIS Stevens, K¹, McManus, S¹, Mark, P², Fox, J¹, Stirling, C¹ ¹Renal Unit, Glasgow Royal Infirmary, ²Renal Unit, Western Infirmary, Glasgow BACKGROUND: Pauci-immune renal vasculitis is an important cause of end stage renal failure in the UK, often affecting elderly patients who have a particularly poor prognosis. Previously we have looked at patient and renal survival and factors which predict outcome. Standard treatment comprises steroids and cyclophosphamide to induce remission; followed by a period of maintenance therapy with a less toxic immunosuppressant, usually azathioprine. There is a lack of consensus over both the optimal dose and the duration of azathioprine maintenance therapy. This study looked at azathioprine dosing, relapse rate and complications. METHOD: The computerised records and case notes of all patients diagnosed with pauciimmune renal vasculitis between 1996 to 2006 at the Glasgow Royal and Stobhill Hospitals were reviewed. Patient demographics and laboratory parameters at presentation were recorded including age, serum creatinine and ANCA status. Treatment regimes, related complications, disease relapse and the need for renal replacement therapy were noted. Infection and relapse was defined by both clinical and serological evidence. RESULTS: In this 11 year period there were 71 patients with pauci-immune renal vasculitis. Following induction of remission, 39 patients were eligible to commence azathioprine and of them 82% (n=32) were commenced on azathioprine as maintenance therapy. Median age was 61 years (range 16-79 years) and 10 patients had a diagnosis of microscopic polyangiitis. Median follow up was 1572 days (range 48-4865 days) from the date azathioprine commenced. Azathioprine was started at a median time of 98 days from diagnosis (range 1318 days). 12 patients were PR3/MPO positive at remission. Median creatinine was 250micmol/L at diagnosis (range74-742micmol/L) and 170micmol/L (range 65350micmol/L) at time of azathioprine therapy. 47% (n=15) of patients suffered a relapse at a median of 539 days (range 76-2769 days) from starting azathioprine. Of these, 87% (n=13) suffered more than one relapse. The mean starting dose of azathioprine in the relapse group was 1.47mgs/kg compared with 1.57mgs/kg in the group who did not. The mean maximum dose in those who relapsed was 1.3mgs/kg compared with 1.7mgs/kg in those who did not. 14 patients (5 of whom relapsed) had clinical/serological evidence of infection whilst on azathioprine; these patients were on a mean dose of 1.56mgs/kg of azathioprine compared with 1.4mgs/kg in those who did not suffer infection. 12 patients (4 of whom relapsed) experienced side effects with azathioprine; 9 of these patients were taking more than 1.5mgs/kg of azathioprine. 10 patients died during the follow up period. CONCLUSION: Our patients are on lower starting doses of azathioprine (the majority of our patients received less than 2mgs/kg of azathioprine) without significantly higher relapse rates compared with figures quoted in the literature. The differences in dosing may relate to the age of our population and the severity of vasculitis (our patients all had evidence of renal involvement). Additionally, we relied upon clinical judgement for identification of relapse and not a formal scoring system. In terms of what dose of azathioprine to use, the best evidence comes from a RCT and suggests 2mgs/kg. However in certain cases, particularly where patients are older it may be acceptable to start at a lower dose.